Dr Katy Gardner Liverpool 3/2/06
“The imperative for reform is urgent and growing. People want more from their public services, to match the choice, customer service and personalisation they can get from their bank, supermarket or on-line shopping.”
Patricia Hewitt Secretary of State for Health December 2005
“Inequality in health is the worst inequality of all. There is no more serious inequality than knowing that you’ll die sooner because you’re badly off”
Frank Dobson, 1997 (Secretary of state for health 1997-1999)
The ideal of Choice
- Woman’s right to choose.
- Choice is about empowering and engaging people, about giving people control.
- But it must be real and it must be equitable.
What is “Choice”?
- Choice in NHS is limited necessarily (see discussion re Herceptin), personal choice must be weighed against public good
- The paradox of choice: real choice, too much choice. Recent US survey results.
- “Choose and book”
- What value does it add to health care?
A diary of CHOICE:
- January 2006: Choose and book. All patients to have the choice of four providers.
- May 2005: a confused patient on a Friday night. Barriers: language, literacy, health literacy and transport
- November 2002: how do we make choice of provider equitable?
Why are we getting it?
- Govt using it to drive up quality and drive down waiting times. But presupposes “informed” choice.
- Evidence that contestability will drive up quality is lacking.
- Govt also wants to “personalise” care but there are costs.
- Patient choice pilot (London) used “Patient Care Advisors”:a great idea and resource intensive. And free transport was provided!
Do people want it?
- In surveys most people said they would like choice of provider but want a health professional to help them choose.
- Heart surgery pilot. Of eligible people only 46% accepted choice of provider.
- London choice pilot: most people favoured the idea of choice (transport and PCAs available).
- 2/3 of people eligible for alternative provision accepted it.
-
CHOICE in secondary care
-
- Choose and book : good in principle
- Who is choosing really?
- Are patients empowered to choose?
- Has anyone got enough inofmormation to make an informed choice?
- Will local providers improve or deteriorate?
- Introduction of private providers increases the cost (PFI, ITCs)
CHOICE in primary care
- Double registration for people who work: NO!
- Choice of provider for long term condtions? Empowerment in the key.
- Possible introduction of alternative providers: this could be good! GPs already “small businesses”
- Primary care in 10 years will look completely different.
- Standards ? raised but fragmentation ? occur.
- Are we diverting energy instead of grasping the clinical governance nettle?
The reality of CHOICE
- Four providers in Merseyside
- No patient advisors (used in London)
- No free transport
- Lack of useful information
- If one provider is continually preferred their wiating time will increase!
Patient empowerment
- Choice cannot be a substitute for public involvment in the NHS
- How much choice does patient have at present in choice of their GP?
- Health literacy still poor for many people. They may favour choice in prinicple but is it a “real” choice?
- Patients as a whole may be less empowered: abolition of CHCs, demise of health forums
- Individual verses the collective good
Instability and fragmentation: jargon
- PBR
- PBC
- ITCs
- PPIs
- HMOs
- APMS
- Contestability
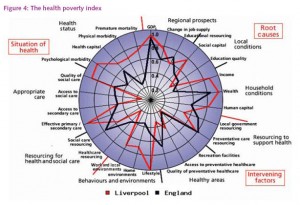
Hidden inequalities
- The choice agenda is expensive: buraucracy, capacity, diversion of resources:
- What are the interventions that will really save lives and improve health outcomes?
- Public health told its evidence is wooly or lacking but where is the evidence that Choice improves health?
Hidden costs
Government has put a lot of new resources into NHS. But where have they gone?
- New contracts (doctors)
- Agenda for change
- PFI,
- Treatment Centres
- Choose and Book
- Backlog from previous underfunding
The future……………..
- Real informed choice or greater inequlities?
- Wanless “fully engaged” or pseudo engagement?
- “amplify the voice of the disadvantaged” (IPPR 2005)
- Crucial role for advocacy, and for voulunatary and community services but with no funding hopless.
- What do people want? Quality services close to home.
