5.1 This Chapter attempts to set the British health experience into the context of developments in other industrialised countries with which comparisons might reasonably be made. In the first part the focus is upon overall national levels and trends (specifically in mortality rates); in the second part data relating to experiences of inequalities in health are presented. International comparisons can sometimes throw additional light upon problems to which government policy is addressed, though clearly difficulties of interpretation derive from the influence of (the many unexamined) cultural and social structural variables. The health field is particularly complex in this sense when anything more than statistical description is attempted. Nevertheless, because the success of other nations (whether in raising income or reducing infant mortality) presents an inescapable yardstick by which national performance is always measured, the attempt to understand these successes is an essential input to analysis.
LEVELS OF HEALTH AND CHANGES OVER TIME
5.2 In part because morbidity data are not available for systematic international comparison the ‘relative health’ of nations tends to be expressed and understood, in terms of relative levels of mortality. Infant mortality is often taken to be the most valid measure.
Table 5.1 Perinatal and Infant Mortality
| Perinatal Mortality per 1000 live births | Infant Mortality per 1000 live births | |||||||||
|
1960
|
1971
|
1975
|
% Decrease 1960-1975
|
Annual % Decrease 1971-1975
|
1960
|
1972
|
1975
|
% Decrease 1960-1975
|
Annual % Decrease 1972-1975
|
|
|
England and Wales |
33.5
|
22.5
|
17.9
|
46.5
|
4.1
|
21.8
|
17.3
|
14.2
|
34.3
|
4.5
|
|
Scotland
|
38.1
|
24.8
|
18.5
|
51.3
|
5.1
|
26.4
|
18.9
|
14.8
|
44.0
|
5.4
|
|
Sweden
|
26.2
|
15.7
|
11.1
|
57.7
|
7.3
|
16.6
|
10.8
|
8.3
|
50.0
|
7.7
|
|
Norway
|
24.0
|
17.9
|
14.2
|
40.8
|
5.1
|
18.9
|
11.8
|
11.1
|
41.3
|
2.0
|
|
Denmark
|
26.5
|
17.5
|
12.7
|
52.1
|
5.5
|
21.5
|
12.2
|
10.3
|
52.0
|
3.9
|
|
Finland
|
25.3
|
16.9
|
13.9
|
45.0
|
5.9
|
21.0
|
11.3
|
11.0
|
47.6
|
1.4
|
|
Netherlands
|
25.6
|
17.8
|
14.0
|
45.3
|
4.3
|
16.5
|
11.7
|
10.6
|
35.7
|
3.1
|
|
France
|
31.8
|
22.8
|
19.5
|
38.7
|
4.8
|
27.4
|
16.0
|
11.1
|
59.8
|
10.2
|
|
W Germany |
36.3
|
25.6
|
19.4
|
46.5
|
4.8
|
33.8
|
22.8
|
19.7
|
41.6
|
4.5
|
|
(E Germany)
|
–
|
19.4
|
17.6
|
17.7
|
15.9
|
3.4
|
||||
|
USA
|
29.4
|
–
|
20.7
|
29.2
|
–
|
26.0
|
18.5
|
16.1
|
38.1
|
4.3
|
Table 5.2 Adult Mortality: Deaths Per Million
| Men | Women | |||||||||||
| 35-44 | 45-54 | 35-44 | 45-54 | |||||||||
| 1964 | 1969 | 1975 | 1964 | 1969 | 1975 | 1964 | 1969 | 1975 | 1964 | 1969 | 1975 | |
|
England and Wales |
2471 | 2298 | 2095 | 7330 | 7242 | 6985 | 1778 | 1737 | 1468 | 4382 | 4379 | 4298 |
|
Scotland
|
3245 | 3195 | 2817 | 9322 | 8757 | 8876 | 2029 | 2098 | 1896 | 5473 | 5646 | 5412 |
|
Sweden
|
2205 | 2292 | 2343 | 5223 | 5329 | 5736 | 1444 | 1494 | 1372 | 3546 | 3385 | 3056 |
|
Norway
|
2327 | 2395 | 2012 | 5664 | 5954 | 6009 | 1299 | 1299 | 947 | 2938 | 3288 | 2955 |
|
Denmark
|
2128 | 2311 | 2420 | 6126 | 5994 | 6865 | 1695 | 1886 | 1579 | 4000 | 4241 | 4529 |
|
Finland
|
4427 | 4758 | 4171 | 11462 | 10748 | 1746 | 1680 | 1430 | 4413 | 4343 | 3537 | |
|
Netherlands
|
2043 | 2086 | 1859 | 5811 | 6100 | 5897 | 1336 | 1473 | 1159 | 3421 | 3418 | 3159 |
|
France
|
3400 | 3650 | 3388 | 8200 | 8050 | 8288 | 1830 | 1773 | 1552 | 4145 | 4135 | 3681 |
|
W Germany |
2919 | 3051 | 3016 | 7724 | 7372 | 7504 | 1942 | 1919 | 1601 | 4461 | 4368 | 4164 |
|
USA
|
3836 | 4108 | 3469 | 9643 | 9627 | 8563 | 2315 | 2383 | 1908 | 5227 | 5098 | |
5.3 Tables 5.1 and 5.2 present the kinds of data which have often given rise to critical appraisal of the success, or otherwise, of health policy in Britain. Comparison on various possible bases yields the following results:-
i. 1975 Perinatal Mortality Rates
England and Wales (and Scotland still more so) had rates significantly above those of the 4 Nordic countries and of the Netherlands. France and Germany had rates similar to the British ones.
ii. Rate of Decrease of Perinatal Mortality
The overall decreases in perinatal mortality rates between 1960 and 1975 show that as a % of the 1960 rate,, England and Wale, and Scotland in particular, performed more than averagely well. However, if we then look at the annual % decrease over the more recent period (1971-75) it appears that the result for England and Wales at least was no longer satisfactory, and improvements were not up to those being achieved in any of the other countries, although rates of improvement since 1975 have been similar to Finland, France and West Germany.
iii- 1975 Infant Mortality Rates
When we turn to infant mortality (referring now to deaths in the first year, not week, of life) – to which socio-environmental factors are acknowledged to be of greater importance than for perinatal death – we find, once more, that the Nordic countries and the Netherlands show the lowest rates. Now, however, France is seen to have joined this group. There is then a significant jump to England and Wales, Scotland, Germany (West and East – the latter being substantially lower than the former), and the USA.
iv. Rate of Decrease of Infant Mortality
The decreases in infant mortality recorded between 1960 and 1975, as a % of the 1960 rates, show England and Wales to have done substantially less well than Scotland and indeed,, than any other country. By far the highest rate of improvement was obtained in France. In contrast to the perinatal rates, however, the relative performance of England and Wales, and Scotland in particular, was more creditable in the more recent period. Between 1972 and 1975 only France and Sweden recorded higher average annual rates of decrease.
v. Adult Mortality
The picture here is somewhat less clear. Certainly so far as younger men are concerned, the 1975 rate for England and Wales is adequate. Moreover, the general improvement recorded over the period 1964 to 1975 (or 6) was not paralleled in some of the countries with the lowest rates (Sweden for example, showed rising mortality among men). In the case particularly of women aged 45-54, however, the data offer little comfort.
5.5 How are such differences to be explained? One way is through comparison of the relative importance of causes of death. If Sweden is compared with England and Wales, taking rates of infant death for a number of major causes it becomes apparent that perinatal factors, and respiratory conditions are major contributants to the poorer British rate.
Table 5.3 Mortality rates under 1 year per 1000 Live births, for selected causes (1976)
| Sweden | England and Wales | difference | |
| Infections (A1-44) | 0.26 | 0.43 | 0.17 |
| Acute respiratory infections (A89) | 0.04 | 0.57 | 0.53 |
| Pneumonia | 0.13 | 1.02 | 0.89 |
| Accidents | 0.08 | 0.35 | 0.27 |
| Various anoxic and hypoxic conditions of preganancy | 1.43 | 2.96 | 1.53 |
| Other causes of perinatal mortality | 1.07 | 2.30 | 1.23 |
| Congenital abnormality | 3.03 | 3.45 | 0.42 |
5.6 Out of the difference in national rates of 5-9 (per 1000 live births), 2.8 is accounted for by the perinatal factors referred to above, and 1.4 by respiratory conditions/pneumonia. In other words, it is not difficult to see how both factors impacting before and during birth, and those which relate principally to the environment and care of the infant have their effect. The difference in death due to congenital abnormality is, relatively, slight. The fact that in Sweden, with its excellent record in perinatal and infant death, the congenital abnormality death rate remain comparable with the situation in England and Wales, has led some commentators to the view that there may here be an “irreducible minimum” beyond which progress is (given present knowledge) unlikely. (see eg Pharaoh and Morris 1979).
Table 5.4 Availability of Healthcare: Physicians, Nurses and Hospital Beds per 10,000 population
| Physicians | Nurses | General (non-psychiatric) Hospital Beds | ||||||||
| 1960 | 1969 | 1971 | 1975 | 1960 | 1969 | 1975 | 1960 | 1969 | 1971 | |
|
England and Wales |
10.5 | 12.1 | 12.7 | 11.0 | 20.8 | 29.6 | 37.5 | 46.0 | 40.7 | 40.7 |
|
Scotland
|
11.8 | 13.3 | 15.6 | 11.0 | 22.0 | 33.9 | 48.2 | 47.8 | 48.3 | 49.4 |
|
Sweden
|
9.5 | 13.0 | 13.9 | 16.2 | 28.6 | 38.2 | 71.1 | – | 67.1 | 69.4 |
|
Norway
|
11.8 | 14.1 | 14.6 | 18.3 | 28.1 | 34.4 | 73.6 | 55.8 | 50.2 | 46.1 |
|
Denmark
|
12.3 | 14.5 | – | 17.9 | 37.7 | 47.2 | 80.4 | 59.7 | 60.5 | 60.1 |
|
Finland
|
6.4 | 9.5 | 11.1 | 13.3 | 33.8 | 35.5 | 81.9 | 41.9 | 43.0 | 46.8 |
|
Netherlands
|
11.2 | 12.2 | 13.2 | 15.9 | – | 44.8 | 32.2 | 45.0 | 47.9 | 53.6 |
|
France
|
10.1 | 13.0 | 13.9 | 14.6 | 18.6 | 25.8 | 50.2 | 55.5 | – | 60.5 |
|
W Germany |
14.9 | 17.0 | 17.8 | 19.2 | 22.0 | 22.1 | 35.9 | 65.3 | 65.3 | 66.8 |
|
USA
|
13.4 | 15.5 | 15.4 | – | 27.9 | 33.5 | 63.7 | 41.4 | 46.5 | 46.7 |
5.7 Another approach might be via comparison of levels of provision of health care. Table 5-4 provides some information on overall levels of provision of physicians, qualified nurses, and (non-psychiatric) hospital beds. Apparently, the differences in number of physicians per 10,000 population are not extreme, and W Germany (the most generously endowed throughout the whole period) shows up relatively poorly in tables of relative mortality. Supply of nurses seems better to accord with the evidence of mortality. But the importance of medical care provision – however expressed has to be considered in relation to that of socio-environmental variables as principal determinants of relative levels of, and changes in, the health of nations.
5.8 Anderson is one who attempted such an assessment in the course of his comparisons of the health services of England, Sweden and the USA (Anderson, 1972). Among the factors mentioned by him are a greater emphasis upon child health in Sweden compared with the health of old people in the USA (but similar proportions of GNP devoted to health care); and differences in access between income groups (not treated in detail). The conclusion by which this author appears to set greatest store is this: “the dominant reason why the Swedish mortality rates are lower than in any state in the United States is a high minimum standard of living for everyone and a cultural homogeneity…….. Health services are, of course, also a factor in the low mortality rates, but the elimination of poverty in the United States in the sense true for Sweden would be more likely to bring mortality rates closer to Sweden than a policy limited to health services only” (P. 158)
5.9 A sophisticated statistical analysis by Fraser (1973) is of particular value. Fraser attempted to explain variation in infant mortality rates (taken to be a good measure of ‘relative health’) between 25 industrialised countries (including 5 from Eastern Europe). Dependent variables are infant mortality rates of ‘955 (actually the average of 1954-1956), 1960 (1959-61) and 1965 (1964-66) used singly and in combination. Independent variables introduced in the first analysis (which used linear regression equations) included: number of physicians per 10,000 people; number of nurses and midwives per 10,000 people; and number of hospital beds per 1,000 people as medical care variables. Demographic and geographic factors were represented by % population living in cities of 100,000 population; population density over the country as a whole; area of the country; % change in population. GDP per capital and % 15,2 year olds in higher education stood for socioeconomic factors (though the latter was properly recognised as a poor measure of average level of education).
5.10 Strong negative effect on infant mortality (in most repressions, i.e. when other variables are held constant) appeared with
– per capita GDP
– number of nurses and midwives per 10,000 population
– number of hospital beds per 1,000 population
– extent of urbanisation
5.11 Population density had a weak negative effect; area and % change in population no effect. The education variable produced internally inconsistent results whereas, most surprising of all, provision of physicians had a slight positive effect on infant mortality.
5.12 A second analysis based on a more limited number of countries for which relevant data could be obtained, showed a weak relationship between of income distribution and mortality (positive), and a weak positive between birth rate and mortality rate. Finally, ranking countries for which Abel-Smith had produced estimates of the proportion of health expenditure devoted to non-personal public health services, gave a good (negative) rank order correlation with infant mortality.
5.13 This study clearly emphasises the importance both of medical and eco-social factors; provision of nurses and midwives and of hospital beds are the most important ‘health service correlates’ of low infant mortality, and per capita GDP and extent of urbanisation of the population the most important socio-environmental ones. The author considers that further work on income distribution and % preventive health expenditure is merited. Whilst correlations of these sorts do not, of course, ‘prove’ that these are the determinants of the rate of infant mortality prevailing in a given country they have to be seen as suggestive for policy and research.
5.14 A similar approach, used recently by Cochrane et al (1978), took 1970 mortality rates among different age groups as the dependent variable. Their study utilised data for 18 Western industrialised countries. Independent variables were mostly similar to Fraser’s, but included also various aspects of diet and per capita cigarette and alcohol consumption. These authors found that the major negative effects on mortality rates seem to derive from per capita GNP, population density, the proportion of health expenditure from public funds, and per capita sugar consumption. Once more, increasing provision of physicians accompanied increasing rates of mortality.
5.15 A weakness of both studies (acknowledged by Cochrane et al) is the limited attention paid to the importance of distributional characteristics of the economic and social structures, and of the existence of inequalities in access to, and use of, health services.
5.16 High overall national levels of infant mortality might in some case be due to the effects of poverty (or other forms of deprivation) on certain groups within the society. As we have seen, it was to the differences in extent of inequality prevailing in Sweden and the USA that Anderson attributed the lower infant mortality rate of the former.
5.17 Some data relevant to further investigation of this problem are given in Table 5.5 though the significance of factors of this kind must await further statistical demonstration.
Table 5.5 Comparison of Inequalities of Pre-tax income and of education
| Gini coefficients for income inequality | Gini coefficients for education inequality | |
| UK | 0.38 | – |
| Sweden | 0.39 | – |
| Norway | 0.35 | – |
| Denmark | 0.37 | Males 0.144; females 0.131 |
| Finland | 0.46 | – |
| Netherlands | 0.42 | 0.167 |
| France | 0.50 | Males 0.172; females 0.159 |
| W Germany | 0.45 | – |
| USA | 0.34 | 0.190 |
5.18 Regional disparities in provision of medical service, studied by the RAWP are not unique to Britain and, insofar as these are associated with regional health inequalities, may also be relevant to overall national rates. In fact, insofar as broadly aggregated data give an accurate picture, the regional distribution of physicians is more equitable in England than is the case in comparable European countries, as shown in Table 5.6
Table 5.6 Regional Variations in No. Physicians per thousand population: Highest and Lowest Areas
| England | France | Germany | Netherlands | |
| Average | 1.06 | 1.47 | 1.74 | 1.36 |
| Highest | N.W. Thames 1.31 | Paris 2.18 | W Berlin 2.97 | Utrecht 2.10 |
| Lowest | Trent 0.91 | Basse Normandie 0.98 | Nieder Sachsen 1.41 | Friesland 0.92 |
| Ratio Highest/Lowest | 1.4 | 2.2 | 2.1 | 2.3 |
Inequalities in Health
5.19 Whereas in the UK mortality statistics and morbidity data, obtained for example through the GHS are routinely presented by social class (according to the occupation-based definition of class discussed elsewhere in this report) the same is not true of other countries. Whether or not because social class is a less politically salient dimension of social stratification than is the case in the UK and because other dimensions are of greater importance, health inequality data are more commonly presented on a geographic or, as in the USA, ethnic basis. To be sure, in those Nordic countries made up of industrialized densely populated southern regions and cold rural northern regions with sparse and declining populations, this is unsurprising. The fact is, therefore, that international data expressing the extent of health inequalities are not readily presented on a comparable basis. Moreover, where social or occupational groupings are used these are not strictly comparable with the groupings used in Britain by the Registrar-General. Additionally, the overall social class compositions of countries are far from identical. Nevertheless, though the data we have collected relate variously to regional, industrial, occupational or income groups, they do permit some attempt at answering the question which we are here addressing: are the health inequalities in England and Wales, for which we have presented abundant evidence, encountered also in Europe and the USA?
5.20 The best way of dealing with our somewhat disparate data is to make country by country comparisons with England and Wales.
Denmark
5.21 Denmark has lower perinatal and infant mortality rates than England and Wales 5.1) and has succeeded in reducing the latter (though not the former) by more than have we. In England and Wales the ratio of class V to class I for neonatal mortality is 2, with regular class increments. Table 5-7 shows the Danish situation.
Table 5.7 Denmark: Neonatal Mortality Rate by Occupation
| 1970 | 1972 | 1974 | |
| Self employed | 10.9 | 8.1 | 5.7 |
| Salaried employee | 9.9 | 9.8 | 7.5 |
| Skilled worker | 10.1 | 8.9 | 8.1 |
| Unskilled worker | 13.5 | 11.3 | 9.0 |
| Other/unknown | 11.1 | 10.2 | 8.8 |
| All | 11.0 | 9.7 | 8.0 |
5.22 here too there is evidence of social inequality, though it is smaller than in England and Wales. The neonatal mortality rate for unskilled workers in Denmark has fallen by about the same percentage as for the country as a whole. This is not so of the UK.
Finland
5.23 Finland is a country which, although enjoying low rates of perinatal and infant mortality, suffers very high rates of adult mortality: far above those of England and Wales. the existence of regional disparities in adult Finnish mortality is well-known: but differences between socail groups are to be found too, as shown in Table 5.8. The ratio of the index for male unskilled workers IV to that for I, (1.9)is somewhat higher than the ratio of SMR’s for social classes V:I in England and Wales (1.8), although the inequality found in Finland among women is lower than in England and Wales.
Table 5.8 Finland: Age adjusted mortality indices (1970) by social group
| Male | Female | ||
| I | Higher admin or clerical employees, comparable employers, and people with academic degrees | 78 | 95 |
| II | lower adminor clerical employees, and comparable employers | 95 | 100 |
| III | skilled and specialised workers | 92 | 102 |
| IV | unskilled workers | 148 | 108 |
| V | farmers | 87 | 96 |
France
5.24 The French data shown in table 5.9 refer to men aged 45-64 (unstandardised for age), excluding those classified in the census as ‘inactive’ (16% of the total, and with a very much higher mortality rate) and excluding three regions of France in which a very high proportion of deaths are attributed to unspecified, or inadequately specified causes. Although the extent of the inequality indicated is presumeably increased by the greater number of occupational groupings compared to England and Wales, it does seem that relativities are comparable with those of England and Wales.
Table 5.9 France 1968 Mortality rates among economically active men aged 54-64 (unstandardised)(per 100,000)
| I | higher cadres (administrators etc) | 699 |
| II | industrialists, liberal professions, large commercial proprietors | 919 |
| III | middle cadres (including teachers, medical/social service personnel, army, police | 928 |
| IV | artisans and small shopkeepers | 1225 |
| V | farmers | 1117 |
| VI | employees (including service workers, clergy) | 1392 |
| VII | qualified workers | 1589 |
| VIII | agricultural workers | 1520 |
| IX | other workers (including miners) | 1169 |
| All | 1189 |
If those classified as ‘inactive’ are included the overall rate rises from 1189 to 1443. Thus though the classifications within I, II and III on the one hand and VII, VIII and XI on the other do not correspond to that used in GB, the pictureof distinctly higher mortality rates in the latter group is comparable with the British.
5.25 Pronounced differences in infant mortality rates also exist in France, both between socio-economic groups and between regions.
Table 5.10 Rates of Infant, Neonatal and Post neonatal death by socio-professional group of father (per 1000 legitimate live births)
|
1956-1960
|
1970-1972
|
|||||
| Infant | Neo-natal | Post neonatal | Infant | Neo-natal | Post neonatal | |
| liberal professions, higher and middle cadre | 17.0 | 12.4 | 4.6 | 11.6 | 8.7 | 2.9 |
| employees | 24.9 | 19.7 | 8.2 | 14.7 | 10.8 | 3.9 |
| industrial and commercial proprietors | 25.4 | 17.4 | 8.0 | 15.0 | 11.2 | 3.8 |
| skilled workers | 28.1 | 17.7 | 10.4 | 26.2 | 11.4 | 4.8 |
| specialised workers | 32.9 | 19.6 | 13.3 | 19.0 | 13.2 | 5.8 |
| agricultural workers | 35.3 | 21.0 | 14.3 | 19.8 | 14.0 | 5.8 |
| labourers | 44.8 | 23.1 | 21.7 | 25.7 | 16.5 | 9.2 |
| All | 29.6 | 18.4 | 11.2 | 15.9 | 11.4 | 4.6 |
5.26 Table 5.10 shows that so far as the first year of life is concerned the ratio between mortality in the most favoured group (liberal professions etc.) and the least favoured (labourers) fell slightly (2.6 to 2.2). There was no change in the ratio of neonatal rates (first month), which remained at about 1.9. In the case of post neonatal death rates, however, the least favoured social group has improved its relative standing most strikingly (ratio of 4.7 falling to 3.2). This latter change is in striking contrast to that noted for great Britain, and seems to imply a greater levelling in the socio-environmatal factors most particularly implicated in post neonatl death in the case of France than in that of Britain.
5.27 A factor of 2 separated the area of France enjoying the lowest infant mortality rate in 1970-72 (Ile de France including Paris, 13.0 per 1000 legitimate live births) from that with the highest rate (Corsica, 24.6 per 1000). In 1956-60 these 2 areas, still ranked first and last, had equivalent rates of 21.8 and 40.2 – ie there had been no change in the ratio.
5.28 The interaction between Socio-economic and regional disparities can be shown by the cross tabulation of infant mortality rates by occupation and region simultaneously. Dinh and Hemery show that, for the group “liberal professions and higher and middle cadres”, the infant mortality rate in 1970-72 ranged from 10.2 in Haute-Normandie and Rhone-Alpes to 17.6 in Corsica; moreover, in 2 areas (Franche-Comte, Languedoc-Rousillon) “industrial and commercial proprietors” actually had lower rates. Similarly, for “labourers”, the range was from 18.3 (Pays de la Loire) to 33.4 (Franche-Comte’); and once more in 2 areas (Corsica and Aquitaine) the group “specialized workers” showed up less well. In terms of the ratio mortality rates between “labourers” and “liberal professions” there was also a considerable range, from 1.4 (Corsica, Aquitaine) to 2.7 (Britanny).
W Germany
5.29 In the German case it seems necessary to use regional disparities as an indication of the existence of health inequalities. Those presnted in Table 5.11 relate to infant mortality (first year) and to early neonatal deaths (first 7 days). Table 5.1 showed that on both these indicators the German experience is less favourable than that of England and Wales.
Table 5.11 W Germany 1974: Infant mortality and early neonatal mortality rates by Land.
| Land | Infant mortality per 1000 live births | early neonatal mortality per 1000 live births |
| Schleswig-Holstein | 18.0 | 10.5 |
| Hamburg | 19.0 | 11.2 |
| Niedersachsen | 21.9 | 13.5 |
| Bremen | 25.9 | 12.1 |
| Nordrhein-Westfalen | 23.2 | 14.3 |
| Hessen | 21.5 | 13.3 |
| Rheinland-Pfalz | 22.3 | 12.6 |
| Baden-Wurttemberg | 17.9 | 11.4 |
| Bayern | 20.4 | 13.2 |
| Saarland | 25.6 | 15.7 |
| W Berlin | 18.7 | 9.3 |
| All | 21.1 | 13.0 |
5.30 Both rates, but particularly the infant mortality rate, show substantial variation. The same is true for England and Wales. The range in infant mortality rates for the German Lander is from 17.9 (Baden-Wurttemberg) to 25.9 (Bremen): a difference of 8.0 or 40% of the lower figure. the comaprison may be made with the RHAs of England and Wales. The lowest infact mortality rate here (1975) is Oxford (12.68 per 1000 live births), the highest Yorkshire (17.93) – a difference of 5.2 or about 40% of the lower figure.
Netherlands
Here too social class or occupation categories do not seem to be employed in analyses of inequalities in health: provincial differences are, however, available. Table 5.12 shows variation in adult mortality rates between the Dutch provinces, standardised for age. Table 5.2 showed that in terms of crude death rates (as indeed for infant and perinatal death rates) the Netherlands was ‘healthier’ than England and Wales overall.
Table 5.12 Netherlands 1971: Age Standardised Adult Mortality per 10,000 population.
| Province | Males | Females |
| Groningen | 88.8 | 71.6 |
| Friesland | 84.9 | 71.9 |
| Drenthe | 88.0 | 76.8 |
| Overjssel | 89.7 | 73.1 |
| Gelderland | 93.6 | 77.4 |
| Utrecht | 93.8 | 70.5 |
| Noord Holland | 94.5 | 73.0 |
| Zuid Holland | 92.4 | 71.4 |
| Zeeland | 80.9 | 68.5 |
| Noord Brabant | 95.5 | 97.4 |
| Limburg | 101.4 | 82.7 |
| All | 92.8 | 74.3 |
5.32 Once more, comparison may be made with OPCS statistics giving SMRs by English and Welsh RHAs. the range in SMRs among males is from 87 (Oxford), 88 (East Anglia) to 113 (North West) and 111 (Northern); for females the range is distinctly smaller, from 92 (Wessex) and 93 (East Anglia) to 108(Northern) and 110 (North West). Allowing for the different bases on which the two sets of figures are given, the ranges from highest to lowest do not seem very different. the superior performance of the Netherlands seems, rather, to be reflected in the distribtion of provinces within this range.
Norway
5.33 Like the Netherlands, Norway distinctly surpasses England and Wales in its rates of perinatal, infant, and adult mortality. Norwegian statistics give standardized mortality rates for the 20 Norwegian counties, in relation to the national average, for adult males and females. The picture differs somewhat between the two groups. In both cases, however, the highest rates are found in Finnmark (the most northerly and very sparsely populated part of the country): 122 for men and 118 for women (1969-72). In the case of men the next highest rate is found in the Oslo area (the industrialised capital in which over 10% of the population live): whereas in the case of women it is in Troms (a county also many hundreds of miles into the Artic circle). These rates are 111 and 110 respectively. The southern regions of more moderate climate which are not industrialised have much lower mortality rates. Leaving aside Finnmark, the range for men is 85-111 and for women 95-110. However if Troms also is omitted, the range for women falls to 95-104, the figure for Oslo being 99 (ie less than the national average). Clearly, in the case of Norway climatic factors render such comparisons of uncertain value.
5.34 Also available are morbidity data, more or less comparable with those given in the GHS, on an income basis.
TABLE 5.13 NORWAY 1975. MORBIDITY BY AGE AND INCOME: PERCENTAGE OF ALL IN EACH GROUP
| persons in multi-person households | single persons, all ages over 16 | ||||||
| annual income | 0-6 | 7-15 | 16-30 | 30-49 | 50-66 | 67+ | |
| under 15000 kr | 35 | 31 | 36 | 52 | 74 | 80 | 78 |
| 15,000 – 29,999 kr | 29 | 30 | 44 | 54 | 76 | 78 | 75 |
| 30,000 – 49,999 kr | 33 | 36 | 45 | 54 | 72 | 78 | 58 |
| 50,000 – 79, 999 kr | 31 | 34 | 42 | 52 | 65 | 77 | 58 |
| over 80,000 kr | 24 | 32 | 39 | 48 | 60 | 67 | – |
(1) ‘Morbidity’ is defined as persons sick on 1 October and/or at least 1 day of restricted activity in the period 1-15 October. Source: Central Bureau of Statistics, Oslo (1977)
These data suggest something of an income gradient in morbidity among single persons and among the older members of multiperson households, though not among 16-49 year olds.
Sweden
5.35 Sweden has the lowest perinatal and infant mortality rates in the world and, moreover, is succeeding in continuously reducing them. The Swedish situation in this respect is of particular interest.
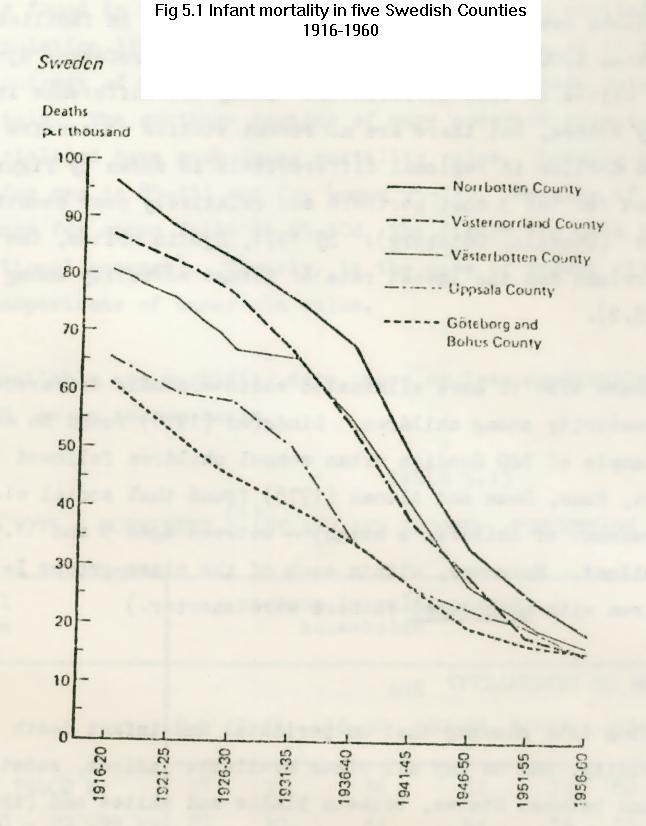
5.36 Early in the century Sweden suffered from substantial differentials in infant death rates on both a geographical and an income basis. Thus, among legitimate infants born in Stockholm between 1918 and 1922, the infant mortality rate in families with an income over 10,000 S Kr was 14.3 per 1000, in families with an income of less than 4,000 S Kr it was 48.9 per 1000. Professor Sjolin of Uppsala University writes of this differential “Today the difference is probably completely erased, but there are no recent studies to confirm it”. (Sjolin 1975). The decline in regional differentials is shown by Figure 5-1 which compares rates for the 3 most northern and relatively poor counties with 2 southern counties (Uppsala, Goteborg). By 1971, Sjolin writes, the northern county of Vasternorrland had the lowest rate of infant mortality among all the Swedish counties (8.2).
5.37 Moreover, Sweden seems also to have eliminated socioeconomic differences in height and age of maturity among children. Lindgren (1976) found no such differences in a sample of 740 Swedish urban school children followed from age 9-17 (By contrast, Rona, Swan and Altman (1978) found that social class remains an important determinant of children’s height – between ages 5 and 11.5 years – in England and Scotland. Moreover, within each of the class-groups I+II+IIIN; IIIM; IV, V: children with unemployed fathers were shorter.)
USA – THE REDUCTION OF INEQUALITY?
5.38 Instead of presenting data showing that on perinatal and infant death rates, on self-reported morbidity, and on any all other available indices, substantial gaps are to be found between States, between blacks and whites and (though data are scarcer) between occupational groups, we shall here take up the question of changing inequalities. Recent studies by Lerner and Stutz, Chase, and Wilson and White represented attempts at assessing the effect of the poverty programmes of the 1960s (the decade of the ‘Great Society’) upon health inequalities in the USA. These three studies focused respectively on adult mortality rates, infant mortality rates, and morbidity/utilization of health services.
5.39 The decade 1960-70 was one in which, for the national as a whole, the overall mortality rate continued to decline, and income rose substantially. Lerner and Stutz looked at corresponding changes in differences between whites and non-whites, and between the 10 highest and 10 lowest income states, on the indicator of adult mortality rate, in this period.
Table 5.14 USA 1960-70 Changes in age adjusted mortality rates by state – income and race
| 1959-62 | 1969-71 | change | ||
| whites | high income states | 743.9 | 690.4 | -7.2% |
| low income states | 738.9 | 729.8 | -1.2% | |
| non-whites | high income states | 998.3 | 927.1 | -7.1% |
| low income states | 1102.4 | 1048.3 | -4.9% |
5.40 Thus, although the relative positions of whites and non-whites did not change greatly, the gap between rich and poor states (taken as roughly reflecting rich and poor individuals) actually widened. This is attributed to the greater availability of medical advance in rich states, greater Medicaid expenditure in rich states, and selective emigration.
5.41 By contrast, Chase found that (using ‘white’ and ‘all other’ “as a substitute” for rich and poor): “Since 1960…….. the gap between the two race groups narrowed. This pattern was in contrast to that in the 1950s when the differences between the racial groups increased. In 1960 infant mortality rates for the two major groups differed by 20.3 per 1,000 live births. By 1972 the difference between them was 11.3 per 1,000, the narrowing of the gap since 1960 was greater after the first four weeks of life……. when socio-economic factors predominate than in the neonatal period.
5.42 Finally, Wilson and White’s study, which used data from the Health Interview Survey, defined the poor as “persons whose family income was in the lowest 20% of the population” (ie less than $3,000 in 1964; less than $6,000 in 1973). These authors first showed that there had been a greater reduction among the poor in the proportion who had not seen a physician in the previous two years.
Table 5.15 USA: % with no doctor visit in previous two years (all ages)
|
white
|
all other
|
all
|
||||
| poor | non-poor | poor | non-poor | poor | non-poor | |
| 1964 | 25.7 | 17.1 | 33.2 | 24.7 | 27.7 | 17.7 |
| 1973 | 16.8 | 13.2 | 18.5 | 15.3 | 17.2 | 13.4 |
5.43 On the other hand there was no evidence for any decline in morbidity-differentials as illustrated by table 5.16
Table 5.16 USA % population reporting limitation of activity due to chronic illness
|
white
|
all other
|
all
|
||||
| poor | non-poor | poor | non-poor | poor | non-poor | |
| 1964 | 28.0 | 9.0 | 16.9 | 7.2 | 25.1 | 8.9 |
| 1973 | 27.2 | 9.9 | 20.6 | 8.6 | 25.6 | 9.7 |
5.44 These studies taken together indicate that the medico-social programmes of the 1960s were associated with (since causality cannot be assumed) reduction in infant mortality differentials (though not adult mortality differentials) and improved utilisation of medical services by the poor relative to the non-poor (but no reduction in differentials in morbidity).
5.45 In so far as this is an accurate picture, it might cobnceiveably be seen as indicative of the relative feasibility of influencing the various indicators of ‘health inequality’ with which we are concerned.
5.46 A recent French study also throws some light on obstetric trends. Roumeau-Rouquette et al attempted to assess the effects of laws promulgated in France in 1970-1971 requiring all pregnant women to attend at least 4 prenatal consultations (at 3, 6, 8 and 9 months) and requiring examination of all newborn infants by a doctor in the first week of life. Additionally, prenatal consultation with a doctor qualified in obstetrics and additional consultations by those assessed as ‘at risk’ were recommended. These authors carried out a study of a representative sample of about 1,000 pregnancies in the Rhone-Alpes region in July 1972 and in June 1975 (Rumeau-Rouquette et at, 1977), to assess the effects principally upon patterns of use of services, but also upon outcome. Overall, the proportion of women having less than 4 consultations fell from 14.4% to 10.6% and the number with an obstetrician responsible for prenatal surveillance rose from 56.5% to 69.3%. At the same time, however, there was a rise in the average educational level of the mothers, in the standard of housing, in the use of contraception, and in the percentage of mothers working, and a fall in the percentage of mothers who already had 2 or more children. So far as outcome was concerned, it was found that the distribution of birthweights was unchanged, but the rate of anomalies or pathologies at birth’ fell from 23.8% to 15.6%.
5.47 The adequacy of prenatal surveillance as a function of various ‘class’ factors showed a complex pattern of change. In 1972 inadequate surveillance (total of less than 4 consultations or first consultation after 3 months) was associated with immigrant status (mother or father), no post-primary education (mother or father), number of children, and manual employment of father. By 1975 the association with educational level of mother and number of children had both fallen considerably. There was no clear change on the basis of manual/non-manual employment of father.
48 So far as policies designed specifically to reduce the overall incidence of perinatal and infant mortality (and the associated morbidity among survivors) are concerned, the successes of France and Finland are of particular significance. Finnish success in reducing these rates is attributed by the Wynns most particularly to
1. reduction in the hazards of childbirth for larger babies (over 2500g birthweight).
2. reduction in the proportion of babies born at below 2500g.
5.49 The Finns, they report, have not “improved the chances of survival of the reduced number of frail babies that that continue to be born in Finland” (M Wynn and A Wynn 1974). Similarly, Geijerstam attributes much of Sweden’s low perinatal mortality rate to the low incidence of low birth weight (Geijerstam, 1969). Nutrition seems to be crucially related to the incidence of low birth weight (see chapter 6) and it is perhaps worth noting at this point that antenatal clinics in Finland typically recommend the consumption of 1-1 ½ litres of milk per day by the pregnant woman – considerably more than is recommended in England. There is, of course, a typically large difference in the consumption of dairy products between England and Finland – among all income groups – a fact which may show up both in perinatal and adult mortality rates (though in opposite senses).
5.50 It is generally agreed that the high rates of attendance for antenatal care characteristic of Nordic countries are importantly related to low rates of morbidity and mortality. In Finland, a 1944 law required the establishment of a least one Maternal Health Centre in each local authority area. At that time, according to the Wynns, 31.3% of pregnant women who subsequently gave birth were registered: by 1968 99.3% were registered at one of the Health Centres. (The figure for Sweden is also over 95%.) Moreover, by 1968 also 91.2% were attending for first examination by the end of the 4th month of pregnancy, By contrast, it seems likely that only about 50% of women have registered by this stage in England and Wales, and in some areas the figure is undoubtedly very much lower. In Scotland, in 1973, only 64.7% of married social class IV women and 59.5% class V had registered by the 20th week of pregnancy (Brotherston, 1976).
5.51 In Finland, the procedure then is that all women deemed to be at risk (for example, by virtue of a previous failed pregnancy, hypertension, etc) are referred from the Health Centre to the antenatal department of a major central hospital, either for one consultation or for all). This accounts for about ¼ of all the women.
5.52 In both Finland and Sweden domiciliary deliveries have virtually disappeared and in both countries policy is to concentrate delivery in major specialized centres.
5.53 If surveillance of all pregnant women from an early stage of their pregnancies is crucial, as seems generally agreed, the question naturally arises as to how this may be facilitated. (It is perhaps also worth adding that since those hardest to reach are likely, by virtue of their circumstances, to be at particular risk, there is likely to be an increasing ‘marginal rate of return’ on coverage of the last few per cent. The gain between 90% and 95% could be as great as that secured by increasing coverage from 80% to 90%.) Both Finland and France have made use of financial incentives.
5.54 In Finland, only mothers who go for examination to a doctor, midwife or Maternal Health Centre within the first 4 months of their pregnancy can receive the maternity grant. In 1974 this could be taken as a cash grant of 80 FMK (£10) or in the form of a baby ‘Kit’ (which the Wynns estimated to be worth double) which most took. The view is that this relatively modest grant served as the necessary inducement at times and among groups of low income. Attendance now is simply taken for granted by all. It might also be noted that travel to the Health Centres is subsidized.
5.55 In France, maternity grants were initially seen as an instrument of ‘natalist’ policy. Between 1946 and 1975 they were paid only where 1. a baby was conceived within 2 years of marriage, or 2. the mother was less than 25 years old, or 3. the interval between births was not more than 3 years (Doguet, 1978). Today the grants which form part of a rather complex French ‘family policy’, are seen specifically as a means of reducing perinatal mortality and birth handicap. To this end the total grant of 1620 francs (£190) is paid in 3 instalments: at the end of 3 months, 6 months and 8 months of pregnancy (dates judged to be of significance for the detection of anomalies). Proof of attendance for these examinations is necessary for receipt of the sums due. A fourth examination, in the 9th month, is also required according to a law of 1971.
5.56 A recent secondary analysis of survey data relating to 11,000 1972 births shows that among french-born mothers (where the father also was born in France) 14% had 3 or less ante-natal examinations, and 9% attended for their first examination after 3 months of pregnancy. These figures rose to 27% and 16% for non-French (migrants) (and to 35% and 16% for the North African-born in the migrant group). However when those mothers who were French-born but were also both married to a manual worker and had received no post-primary education were considered alone they also rose to 20% and 12% (Kaminski et al , 1978). Thus, although there are both class and ethnic differences in this respect in France, like those in Britain, the overall rate of attendance seems to be distinctly better.
5.57 In both France and Finland financial incentives also play a part in ensuring post-natal medical examination.
5.58 In Finland, the Maternity Health Centres are informed of all births to mothers registered with them. The mother is visited by a midwife within 48 hours of returning home, who has the duty of ensuring that the child is registered at a Child Health Centre. Today, over 90% of children are registered within 1 month of birth. The proportion of those registered with the first year rose from 84.7% in 1957 to 94.2% in 1969. Each child is seen 10-11 times in the first year (twice by a doctor), and then twice a year between the ages of 1 and 6 by Health Centre staff. This is higher than in Britain, where the National Child Development Survey found a figure of about 80%. Official statistics show that of children born in England in 1974 90.1% attended a child health clinic in 1976. However, in some AHAs the figure is very much lower: eg Birmingham 71.2%, Camden/Islington 70.6%, Salford 68.2%, Cornwall 62.4%. The Wynns point to the important contribution made by these staff beyond the assessment of purely medical well-being. They teach parents about nutrition, the care of minor ailments, dealing with behaviour problems and the importance of mental stimulation of the child. It appears that parents increasingly go there for advice on aspects of child behaviour.
5.59 In both Finland and France financial incentive is used here too. In Finland a maternity allowance (at the rate of sick pay) is paid all insured working women for the period 18 working days before birth to 36 working days after. It is paid in 3 instalments, the third only after attendance for post-natal medical examination. In France, there exists a post-natal allowance of 2130 francs (about £240), also paid in 3 instalments. For the first, the child must be examined within the first week of life, for the second within the 9th month, and for the third within the 24th month.
5.60 As well as these incentives, it is important to note that in Finland, where an appointment at the Health Centre is missed, a midwife or health visitor Visits the home. This is felt to be very important and is, of course, made possible by very much more generous staffing levels. Also regarded as important to Finnish practice is the accountability for coverage required of Finnish public health services. The implications of this for the UK are discussed in Chapter 7.
5.61 It is clear from these experiences that strenuous efforts to increase the coverage of ante-natal and child health services to near 100% yield major benefits for perinatal and infant mortality rates. It is not possible unambiguously to conclude that the financial incentives used in Finland and France are themselves directly responsible for the improved rates of attendance (and consequent reduction in death and, inevitably, in perinatal morbidity). But irrespective of this the ‘outreach’ capacity of the Finnish system (following up all missed appointments etc) must be stressed. So too, in our view, must the importance of adapting the functioning of these health centres to the needs and the difficulties of those whose attendance must be secured.
5.62 It is worth noting, also that the obligations upon women in France to attend antenatal care in force since 1971, intended to increase coverage form part of a broader attack on handicap of perinatal origin (Wynn and Wynn, 1976). Other measures include improvement in equipment and staffing of major obstetric departments; establishment of more ICUs for newborn infants; regulation as to minimum standards of equipment, staffing, size etc binding on all establishments with maternity units, whether public or private. This latter has led to the closure and amalgamation of many small units. Moreover, it now appears that concern in France is not with coverage of antenatal care (which is adequate) but with the poor quality, and often perfunctory nature, of the examinations given. Also, the striking reduction in ‘class’ differential in post neo-natal mortality rates suggests some levelling in social, economic and environmental conditions. It is noteworthy that, between 1956-60 and 1970-72 this reduction has been much greater than the (negligible) reduction in the class differential in neo-natal rate – implying a greater relative levelling of environmental conditions than in obstetric care.
CONCLUSIONS
5.63 Comparison of the British experience with that of other industrialised western countries, on the basis of commonly used overall mortality rates, shows that British perinatal and infant mortality rates are distinctly higher than those of the 4 Nordic countries and of the Netherlands, and comparable with those of Western Germany. The rate of improvement in perinatal mortality enjoyed by Britain over the period 1960-75 was as good as that of most other countries though the rate of gain is now poor. Moreover in the case of infant mortality all comparable countries have done better, especially France. Adult mortality patterns especially in the younger age groups, compare reasonably with other countries.
5.64 Why, then, might it be that infant mortality in particular presents so dismal a picture? Analyses quoted earlier suggest that infant death rates are associated with a number of characteristics of socio-economic and health systems. Low infant death rate seems clearly to be associated with per capita GDP, and there is some evidence for an association with an egalitarian income distribution (In other words distributional aspects of society – and the extent of income inequalities – may be related to national performance in the infant mortality rankings). So far as health policy is concerned, it seems that extent of provision of nurses and midwives, and of hospital beds, are more important than provision of physicians. Not unrelated, it seems that a relative emphasis upon preventive antenatal, and child health services within health policy is required. International comparison here may thus have implications for policy.
5.65 It is possible, of course, that the superior performance of Sweden, Netherlands etc might be attributed to difference principally in the extent of internal inequalities. Thus, if the perinatal mortality rate for all England and Wales were equal to that of social classes I and II or the infant death rate equal to that obtaining in Oxford RHA, there would be little difference between these countries and ours. The second question, then, is whether the inequalities in health between social classes and regions, found in Britain, also exist elsewhere
5.66 Briefly, the evidence of section II – although disparate and not permitting comprehensive comparison – suggests that they do. The evidence relating to France and Germany (in the first case on an occupational basis in the second on a regional basis) indicates disparities broadly corresponding to those of Britain. Finland also seemed comparable. So too did the Netherlands, at least in terms of the total range of regional inequality noted. Only in the cases of Norway and Sweden did a significantly smaller inequality appear to obtain. Moreover, in both these cases the extent of regional inequality (at least on the index of adult male mortality rate) seems to have fallen consistently over the years. American evidence on changing inequalities suggests an improvement in the case of infants and access to medical services, but not in adult mortality or morbidity.
5.67 If the evidence for changes in the extent of inequalities is slight (and in the American case ambiguous) that for the success of specific policies designed to reduce inequalities is slighter still. Clearly, as the study by Rumeau-Rouquette et al showed, various dimensions of comparison can produce discrepant results, and changes in extraneous variables may often interfere. Of course, this study also suggested that reductions in inequality of access to, or utilisation of, prenatal care can come about.
5.68 None of the results quoted enable us to deal with the question of the relative importance of inequalities in provision or utilisation of health services on the one hand and other forms of inequality on the other in determining inequalities of outcome. (Although it is noteworthy that provision of physicians is more equal on a regional basis in England than even in the Netherlands.) An aspect of this question is that of the intervention of social class or related factors between morbidity and use of health services. Is it commonly the case that working class or low income individuals or families have less recourse to the health services when they are sick? There are relatively few studies to draw upon.
5.69 One important one was carried out by Purola et al in Finland in 1964, just prior to the introduction of much expanded health insurance (Sickness Insurance Act) which for the first time covered primary medical care. Methodologically this study, like the General Household Survey, was based on a questionnaire administered to a representative sample of non-institutionalised families (not households). Questions covered self-reported morbidity, use of health services, income etc. The most important conclusion for our present purposes was that the number of consultations with a GP in a given period of time was proportional to income, when number of days of reported sickness was held constant. A similar relationship obtained in the case of the chronic sick. On the other hand, the number of days spent in hospital was not a function of income. Moreover, since it was known that incomes in rural areas were lower than in urban areas, and had been established that distance to physicians were greater in rural areas and that consultation rates were inversely proportional to distance, the effects of income were examined holding both morbidity and distance constants The effects of income, on GP consultation rates and those of distance were independent of each other (Purolat 1968).
5.70 The Finnish Sickness Insurance Act was designed to reduce the financial disincentive to making use of physicians’ services. It does not appear however that organisational or financial arrangements can wholly compensate for income inequalities in bringing about parity of usage.
5.71 An analysis by Salkever of data collected in 5 countries with very different health systems (Liverpool, Helsinki, Lodz, Baltimore and NW Vermont, and an area of Saskatchewan) – in the context of a WHO study – throws some light on this (Salkever, 1975). Relating probability of contacting a physician to an index of (perceived seriousness of condition; days restricted activity; days in bed), for various income levels, Salkever found first that in all cases except Saskatchewan low income children fared worse. That is, their reduced utilisation was independent of the organisation and costs of health care. Among adults, it appeared that the clearest association of low income with low utilisation was found in Liverpool. If American and French experiences are any guide, this is one aspect of the cause of health inequality which can be corrected.
Chapter 5 REFERENCES
Anderson OW: Health Care – Can there be Equity? ( NY Wiley, 1972)
Chase HC: “Infant mortality and its concomitants 1960-1972” Medical Care 15. 8 (Aug 1977) 662
Cochrane AL, A St Leger and F Moore: “Health service ‘input’ and mortality’output’ in developed countries” J Epidem and Community Health 32 (1978) 200
Denmark: Medicinsk F/dselsstatistik (Copenhagen, 1970
Derrienic F, P Ducimetiere et s Kritsikis: ” La mortalite cardiaque des Francais actif d’age moyen selon leur categorie socio-professionelle et leur region de domicile” Rev Epidem et Sant Publ. 25 (1977)151
Dinh Quang Chi and S Hemery “Disparites regionales de la mortalite infantile” Economic et Statistiques (1977) 85_, 3-12
Doguet M L “Les prestations familiales en France: Bilan et perspectives” Rev Fr des Affaires Sociales 32, 1 (Jan-Mar 1978) 3-48
Eurohealth Handbook 1978 (N Y and Brussels: Robert S First, 1978)
Fraser R D : “An international study of health and general systems of financing health care” Int J Health Services 3, 3(1973)369
Geijerstam G: “Low birth weight and perinatal mortality” Pub Health Rep 81+ 939-^8 Nov 1969
Germany: Bevolkerung und Kultur, Reiche 7- Gesundheitswesen 1974 (Wiesbaden:Statistiches Bundesamt, 1974
Kaminski M, B Blondel, G Breart, M Franc, C Du Mazaubrun: “Issue de la grossesse et surveillance prenatale chez less femmes migrantes. Enquete sur un e’chantillon representatif des naissances en France en 1972” Rev d’Epidem et de Sante Publ 26, 1(1978) 29-46
Lerner M and R N Stutz:”Have we narrowed the gap between the poor and the non-poor? Narrowing the gaps 1959-61 and 1969-71 -Mortality” Medical Care 15, 8 (Aug 1977) 620
Lindgren, Gunilla: Height, weight. and menarche in Swedish urban school children in relation to socio-economic and regional factors” Annuals Human Biol 3 (1976), 6, 501-28
McKinsey: Health Care – the Growing Dilemma (N Y, 1974
Maynard A: “The medical profession and the efficiency and equity of health services” Soc and Econ Admin 12, 1 (1978)3
Morris J N “Scottish Hearts” Lancet 3.11 1979
Naytia S: “Social group and mortality in Finland” Brit J Prev Soc Med 31 M 1977) 231
Netherlands: Compendium Gezondheidsstatistiek Nederland (Centraal Bureau voor de Statistiek, 1974.
Norway: Sosialt Utsyn 1977 (Oslo: Statistisk Sentralbyra”, 1977)
OE C D: Education and Distribution of Income (Conference of Policies for Educational Growth, Background study No 11. 1970. Unpublished) .
Paukert, F. “Income distribution at different levels of development a survey of evidence” Int Labour Rev 108 2/3 (1973)3
Pharaoh P 0 J and J N Morris “Postneonatal Mortality” in P E Sartwell (ed)
Epidemiological Reviews1 (1979) pp1?0-l83
Purola,T., E Kalimo, K Nyman, and K Sievers: The Utilization of the Medical Services and its Relationship to Morbidity, Health Resources and Social Factors (Helsinki, Research Institute for Social Security, 1968)
Rona R J , A V Swan and D G Altman “Social factors and height of primary schoolchildren in England and Scotland” J Epidem and Comm Health
Rumeau-Rouquette C et al “Evaluation epidemiologique du programme de Sante en perinatologie. I Region Rhone-Alpes 1972-1975” Rev Epidem et Sante Publ. 25_ (1977)10?
Salkever, D S “Economic class and differential access to care: comparisons among health care systems” Int J Health Services 5 (1973),3,373
Sjolin S: “Infant mortality in Sweden” in Helen M Wallace(ed) Health Care of Mothers and Children in National Health Services (Camb Mass, Ballinger, 1973)
Wilson H W and E L White: “Changes in morbidity, disability and utilization differentials between the poor and the non-poor. Data from the Health Interview Survey 1964 and 1973” Medical Care 15, 8 (1977)636
Wynn M and A Wynn:The Protection of Maternity and Infancy. (A study of tt Services for Pregnant Women and Young Children in Finlad with some comparisons with Britain) (Council for Childrens Welfare, London, 197^).
Wynn Mand A Wynn:Prevention of Handicap of Perinatal Origin (An introduction to French policy and legislation) (London; Foundation for Education and Research in Childbearing, 1976)
