Health inequality in Wales
ANEURIN BEVAN MEMORIAL LECTURE Saturday 18th October 2003
Professor Gareth Williams

School of Social Science Cardiff University
(speaker’s notes)
When Was Wales?
‘This is the first point to grasp about the history of this people. Wales is impossible. A country called Wales exists only because the Welsh invented it. The Welsh exist only because they invented themselves. They had no choice….. Men and women make their own history. But they do not make it in circumstances chosen by them.…’ (Gwyn A. Williams, When Was Wales?, Penguin, 1985, pp 3-5)
History is what you live
‘Graig level killed a few men, besides silicotics, arthritics, ripped flesh, smashed bones and damaged souls… Black historied all right, the Graig level, where we slaved in dust and water, where I worked with or in the same headings as Sid Hullen (dust, dead), Jimmy Shanklyn (rheumatic fever, dead), Walt James (dust, dead), Cliff Williams (TB, dead), my father (dust, arthritis, dead)… Just a small level, the Graig, where lads were punished by grinding toil, and before that weakened by the diet of beggars’
(Ron Berry, History is What You Live, 1998)
A history of ill-health
‘Standards of health were continually and insidiously undermined. Children, in particular suffered from malnutrition, rickets, diphtheria and pneumonia, with a fifth of Merthyr children in the late 1930s dying before they reached their fifth birthday. Average life expectancy in Merthyr was forty-six and a half years in 1932, and 65,000 of the inhabitants of the coalfield died ‘avoidable deaths’, due to the impact of poverty upon health, in the decade after 1926’
(Chris Williams, Capitalism, Community and Conflict: the south Wales Coalfield 1898-1947, 1998).
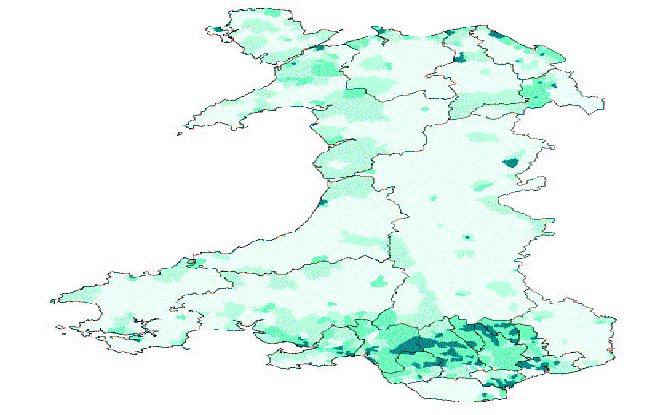
The Census 2001 – health
% of population with limiting long-term illness
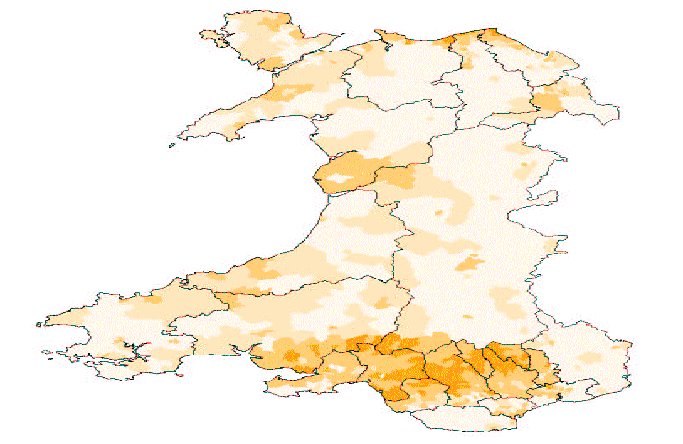
- Merthyr Tydfil 22%
- Blaenau Gwent 21%
- Rhondda Cynon Taff 21%
| Local Authority | Limiting long term illness | General health – not good | Permanently sick or disabled | Ranking % Permanently sick or disabled |
| Easington | 30.8% | 17.3% | 16.3% | 1 |
| Merthyr Tydfil | 30.0% | 18.1% | 15.9% | 2 |
| Neath Port Talbot | 29.4% | 16.4% | 13.6% | 4 |
| Blaenau Gwent | 28.3% | 16.5% | 13.8% | 3 |
| Rhondda Cynon Taf | 27.2% | 15.7% | 13.0% | 5 |
| Caerphilly | 26.3% | 15.0% | 12.1% | 7 |
| Carmarthenshire | 26.3% | 13.9% | 11.1% | 9 |
| Bolsover | 25.8% | |||
| Blackpool | 25.4% | 13.9% | ||
| Barnsley | 25.2% | 14.1% | ||
| Torfaen | 13.9% | |||
| Knowsley | 12.2% | 6 | ||
| Liverpool | 11.4% | 8 | ||
| Barrow in Furness | 10.8% | 10 |
% Economically inactive
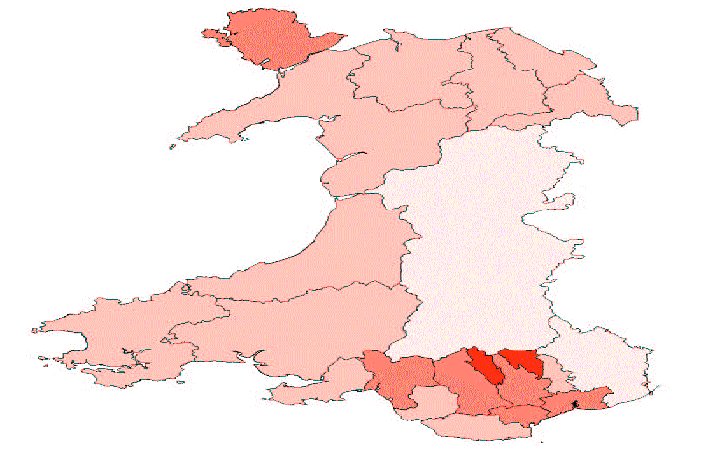
- Merthyr Tydfil 35%
- Blaenau Gwent 34%
- Neath Port Talbot 32%
% Household incomes of less than £10,000
- Merthyr Tydfil 66.4%
- Blaenau Gwent 64.4%
- Rhondda Cynon Taff 63.8%
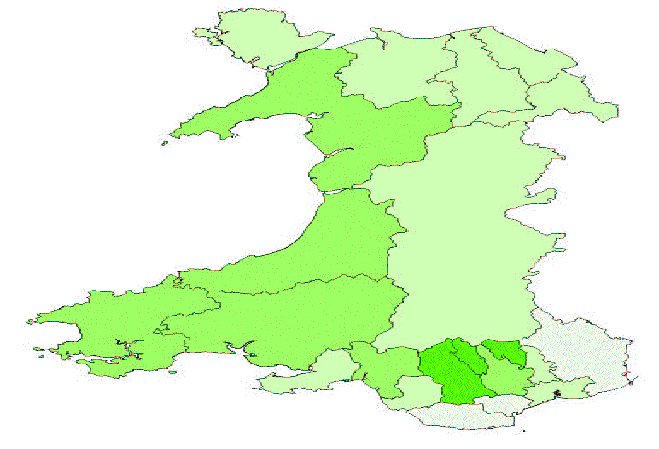
% Adults with no qualifications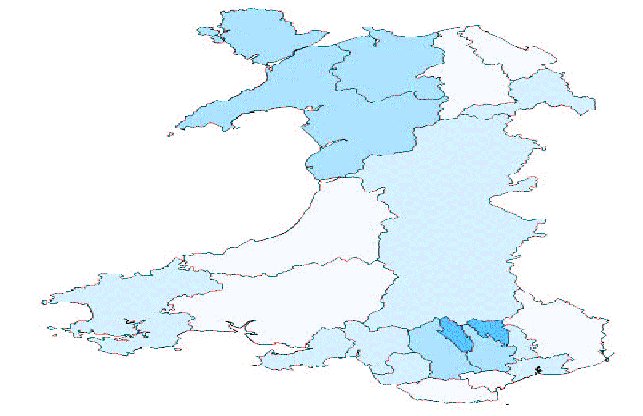
- Blaenau Gwent 37%
- Merthyr Tydfil 33%
- Gwynedd 30%
% Household without access to a car
- Merthyr Tydfil 43%
- Blaenau Gwent 43%
- Rhondda Cynon Taff 39%
South Wales: mining employment (1947-94)
| Date | Collieries | Workforce |
| 1947 | 214 | 114,930 |
| 1960 | 127 | 83,400 |
| 1970 | 52 | 38,000 |
| 1980 | 35 | 25,328 |
| 1990 | 3 | 1,200 |
| 1994 | 0 | 0 |
Coalfields Task Force
… we have been left in no doubt about the scale of deprivation and decline. But what makes the coalfields special is the context in which this decline has taken place. They have a unique combination of concentrated joblessness, physical isolation, poor infrastructure and severe health problems.
(CTF, 1998, para 1.2)
Not Just Economic Decline
‘[In South Wales] This was not just a case of localised economic decline but rather one of cultural crisis. The collapse of coalmining undermined a range of mechanisms of social regulation that were grounded in the politics of the workplace and the trades unions, but spread more widely into local society and politics. There was an acute sense of loss in places in which coalmines closed after decades of existence.’
Bennet, Beynon, Hudson, Coalfields Regeneration: Dealing with the Consequences of Industrial Decline, Bristol, The Policy Press, (2000)
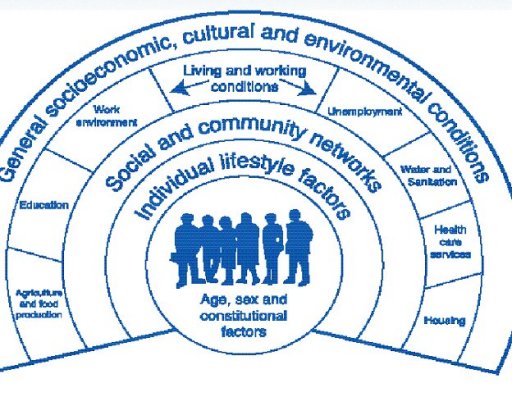
Determinants of health & well-being:
[From Dalgren and Whitehead]
Understanding Context
‘What is missing is a discussion of the relationship between agency (the ability of people to deploy a range of causal powers), practices (the activities that make and transform the world we live in) and social structure (the rules and resources in society). Without such an understanding, factors associated with people’s disease experiences within a context tend to be denuded of social meaning’ (Frohlich, K. et al, A theoretical proposal for the relationship between context and disease, Sociology of Health and Illness, 23, 2001, 776-797)
Experiencing Disadvantaged Places
- ‘I think the biggest health risk is mentally … ‘cause it’s a lot of pressure and there’s nothing really for you to do… you’re sort of segregated all the time’.
- ‘Smoking, drinking and drug-taking. I put it down to one thing … until money is spent on these areas … there doesn’t seem to be much point in trying to stop people smoking and what else. As long as the environment is going down the pan the people will go down with it’.
Divisions in Places
- it’s the people that live in the flats
- the private landlords are letting any Tom, Dick or Harry in now
- Young people today, they don’t respect anything
Agency and context
‘The doctor put me on Prozac a few months back, for living here, because it’s depressing. You get up, you look around, and all you see is junkies… I know one day I will come off, I will get off here. I mean I started drinking a hell of a lot more since I’ve been on here. I drink every night. I have a drink every night just to get to sleep. I smoke more as well. There’s lots of things…‘ (Single mother with one child living on a housing estate in a northern English town).
‘In the space of about six months about two years ago I buried five drug-related deaths. The youngest was 18 years of age and the oldest was a 27 year old mother who lived in one of the streets up here. And I knew her parents fairly well. She left a three year old boy for her parents to look after’. (Church Minister, Blaenau Gwent)
Context and structure
‘People talk not only about the effect on individuals; it’s the effect on the borough – everybody, regardless of whether they are employed by Corus or not. I think there is a huge concern that in an area that appeared to going downhill anyway this is the final nail in the coffin’ (Health Visitor, Blaenau Gwent)
Better health, better Wales (1998)
- Legacy of poor health
- Sustainable health and well-being
- Healthy lifestyle
- Healthy environment
- Partnerships for health
- Measuring progress
- Investing in the future
A Made in Wales Agenda
- ‘We will tackle the legacy of poor health in Wales by developing over the next 15 months clear and practical policies, tackling determinants of health, placing a greater emphasis on primary care….’ National Assembly for Wales, May 2000
A plan for the NHS in Wales
‘The Assembly has developed […] a number of strategies to counteract social exclusion and to create a socially inclusive Wales. It recognised the importance of building and supporting strong communities where the values of citizenship and collective action can grow […] This (Health) Plan builds on wide consultation over the elements that make it up and is part of the process of replacing elite policy making by participative policy development. Our policy here is to build on this commitment and to continue to enhance the citizen’s voice at the heart of policy (emphases in the original).
(National Assembly for Wales, Improving Health in Wales: a Plan for the NHS with its Partners, January 2001)
Structural change
- Local Health Boards: Responsible for bulk of health service funding; budget determined by new resource allocation formula
- Strategic Partnerships: LAs and LHBs under a duty to implement a local strategy and required to co-operate with NHS Trusts and other statutory and voluntary partners
- Health Commission Wales: responsible for commissioning of tertiary services
Emerging themes in Welsh health policy
- A health service not an illness service
- A primary care led service
- Making it local
- Citizens not consumers
- Equality of outcome
- Power comes from ‘voice’ not ‘choice’
- Investing today for tomorrow
Four health systems
- New producerism (Scotland)
- New managerialism (England)
- Policy stasis (N. Ireland)
- New localism (Wales) – ‘What Wales has really done is change the agenda’ (after Scott Greer, forthcoming)
Challenges for Welsh health policy
- Innovative experiment in a primary-care led, public health orientated health system
- Underpowered health service, with lack of policy capacity
- Instability of multi-agency partnerships
- Development of scientific and civic capacity
The future of Wales
‘Small wonder that some, looking ahead, see nothing but a vision of a depersonalized Wales which has shrivelled up into Costa Bureaucratica in the south and a Costa Geriatrica in the north; in between, sheep, holiday homes burning merrily away and fifty folk museums where there used to be communities’
(Gwyn A. Williams, When Was Wales? Penguin, 1985, p 303)
