Chapters 2, 3 and 4 of Prof Stephen Harrison‘s book, published by Avebury 1994, reproduced by permission. (Not all the tables are reproduced)
2 Management in the NHS: Before and after Griffiths
This chapter has three main purposes. The first is to provide a general background against which the rest of the study may be read. The second is to establish that notions of more individually accountable management, in particular a chief executive or general manager, have on several occasions in the history of the NHS been considered and rejected. The third is to show that such notions, if implemented, would represent a radical departure from earlier NHS practice.
The chapter is divided into five sections. The first provides an overview of developments in the organisation and management of the NHS from its foundation until immediately before the commissioning of the Griffiths Report in 1982. This overview shows a consistent and growing interest in the topics of management and organisation. The second section looks beyond these formalities to the actual practice of management in the service, finding an official and institutionalised unwillingness to challenge the medical profession in the way implied by conventional notions of management. The third section gives an overview of the analysis and prescription offered by the Griffiths Report of 1983. The fourth section summarises the central argument of the chapter; the proposal to introduce general management was radical but not new. The chapter concludes with a postscript which describes the further and subsequent set of radical organisational arrangements associated with the white paper Working for Patients (DoH et al 1989).
Overview: 1948-82
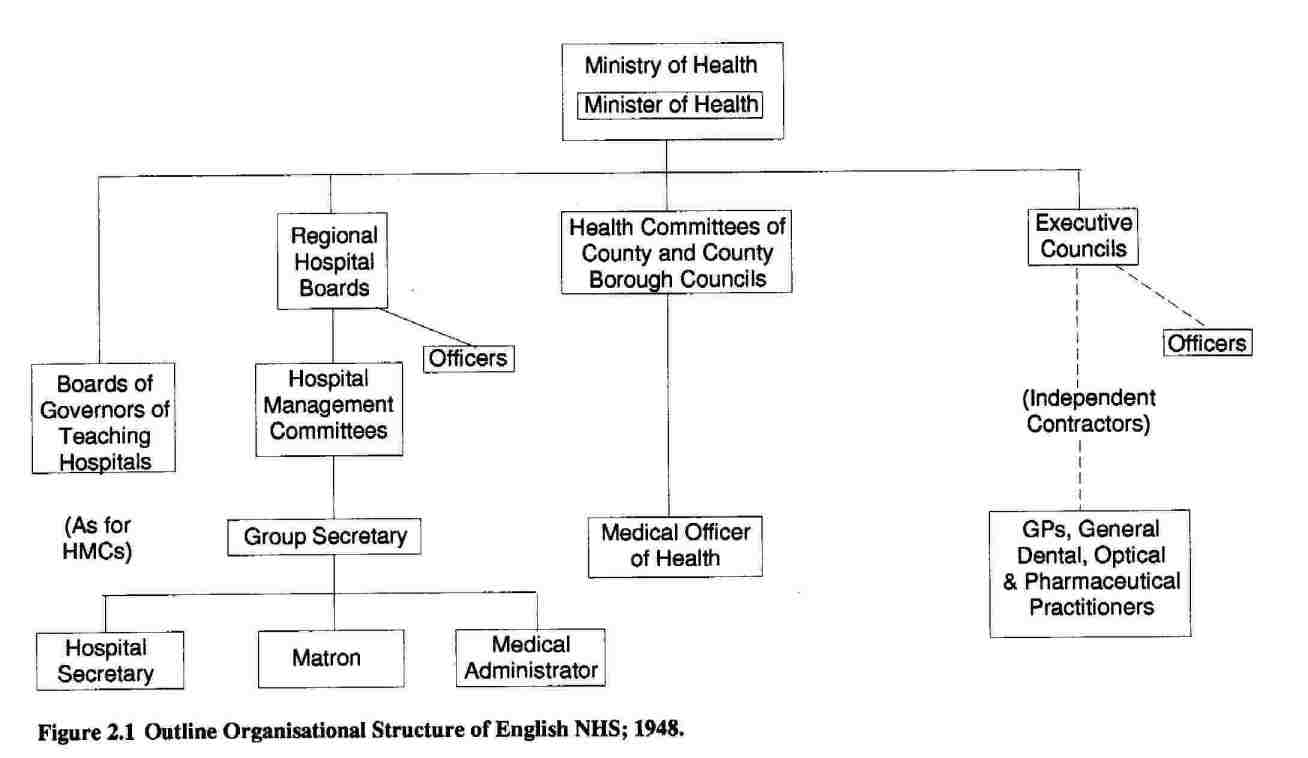
In 1948, the newly-created NHS took the form of a ‘tripartite’ structure, a political compromise between the Labour government and various provider groups (Willcocks, 1967, p. 105), in which control of primary care was separated from that of community services, which in turn was separated from that of hospital services. The initial management arrangements for these three parts of the service very much reflected what had gone before. In the case of primary care, General Medical Practitioners (GPs), General Dental Practitioners, Pharmacists, and Opticians were self-employed practitioners whose contracts were administered by Executive Councils upon which the four professions were themselves heavily represented. This arrangement differed little from that made following Lloyd George’s National Insurance Act of 1911 (Willcocks, 1967, p.75). The staff of the Executive Council, whose role was to maintain GPs’ lists of patients and to receive practitioners’ claims for payment, was headed by an Administrator with managerial control only over the staff, not the practitioners.
The second arm of the tripartite arrangements was provided by local government: County Councils and County Borough Councils. These bodies lost their former duties and rights to provide hospital services, remaining responsible for preventive services, maternal and child welfare, health visiting, home nursing, ambulances, and the school medical service (Levitt, 1979, p. 19). Such local authorities appointed a health committee of councillors, to whom the Medical Officer of Health (MOH) was responsible for the above services. Although it was widely perceived by MOsH that they had lost a great deal of executive authority as a result of the loss of local authority hospital services (and District MOsH lost a great deal more to County MosH), they nevertheless remained, in effect, chief executive officers with formal authority over all their staff, including other doctors (Lewis, 1986, pp. 46-9).
Hospital authorities constituted the third part of the structure. Great Britain was divided into nineteen (later twenty) Regions, each containing a medical school and each controlled by a Regional Hospital Board (RHB) responsible to the Minister of Health. Groups of hospitals (occasionally single large hospitals) within each Region were presided over by Hospital Management Committees (HMCs) or Boards of Governors in Scotland. Groups of English hospitals with medical undergraduate teaching functions were run by Boards of Governors, who, unlike HMCs, were responsible noi to the RHB but directly to the Minister of Health. The membership ol Boards and Committees was part-time, honorary, and appointed rather thar elected (see Watkin, 1978, pp. 24-26): doctors were heavily represented (Allsop, 1984, p. 17). Boards and Committees employed a chie administrative officer (often known as the Group Secretary), and individual hospitals were normally managed on a day to day basis by a triumvirate consisting of Hospital Secretary, Matron, and Medical Superintendent or medical administrator (Central Health Services Council, 1954, pp. 12-14) The ‘tripartite’ arrangements are outlined in Figure 2.1.
It was not long, however, before these management arrangements, and management more generally, were to come under a scrutiny to which they have been subject, and with increasing intensity, ever since. Even before the advent of a Conservative Government in 1951, concern had been growing about the costs of the NHS, which had consistently exceeded estimates (Klein, 1983, pp. 33-40). The Guillebaud Committee, established in 1953 to investigate the cost of the NHS, made it clear in its report that there was no financial crisis; rather, estimates had failed to allow for demographic change or the occurrence of inflation. Nevertheless, it went on to call, in very general terms, for more emphasis on ‘oversight and supervision of the service’ (Committee of Enquiry, 1956, para 211). At roughly the same time, the Bradbeer Committee was responding to the uncertainties about management relationships expressed by NHS managers from widely differing pre-NHS backgrounds. The Committee legitimised the existing trend for HMCs to have one chief administrator at Group level but a triumvirate arrangement at hospital level (see above); it opposed the appointment of matrons or medical officers at group level, and (like Patients First twenty-five years later: see below) argued that lay departmental heads within a hospital should be responsible to the Hospital Secretary (Central Health Services Council, 1954, paras. 20, 28, 196).
Bradbeer had reported before Guillebaud, so that the latter had been able to endorse the former’s conclusions about the virtues of the triumvirate model of hospital management. This conclusion was vigorously criticised by the National Association of Hospital Management Committee Group Secretaries in their commentary on Guillebaud; though they stopped short of proposing a general manager for the hospital, they sought a more substantial role for the hospital secretary than implied by either Bradbeer or Guillebaud:
The suggestion that … administration … undertaken by a doctor “can have an important bearing upon hospital efficiency and costs” is all too true, but not, it is feared, in the sense intended … It is little short of ludicrous that great economy … shall be claimed as a merit of “medical administration” … The Guillebaud Committee has clearly and rightly regarded the “comprehensive” administrator as essential … but it should be clearly understood that this … cannot exist side by side with any theory of “medical administration” (National Association of Hospital Management Committee Group Secretaries, 1957, para 17).
Guillebaud had called for more attention to be given to the recruitment training and promotion prospects of NHS administrative staff and these were the subjects of the subsequent Noel Hall (1957) and Lycett Green (1963) Reports (Watkin, 1975, pp. 159, 175).
The first decade of operation of the NHS had provided the occasion for the medical profession to call for a review of it; the Porritt Committee produced a wide-ranging Report on behalf of the British Medical Association (BMA) and the Royal Colleges. Notable amongst its recommendations was its call for the integration of the three parts of the tripartite structure, though without changing the employment status of doctors. In each locality the three parts of the service would be separately managed by a medically qualified administrator, though at the level of the individual hospital the Bradbeer recommendations (see above) were endorsed (Medical Services Review Committee, 1962, paras. 77, 85, 425). Simultaneous with Porritt’s deliberations, the Hospital Plan for England and Wales was being produced (Ministry of Health, 1962); this was to result in the concept of the ‘district general hospital’, offering a comprehensive service from 600 to 800 beds, together with appropriate outpatient and diagnostic services (Allen, 1979, p. 72). It also provided the occasion for an enhanced management role in planning and commissioning capital developments.
The period of Labour Government from 1964 to 1970 was also to provide a sustained, if diverse, emphasis on questions of management. A 1966 paper on the management functions of hospital doctors noted that ‘the industrial manager works in a…unified and clear environment; his responsibilities are…readily definable and his work is…easily evaluated… In British hospital management, these supportive and critical elements are lacking’ (Advisory Committee, 1966, pp. 8-9). The paper went on to urge Consultants to improve management by improving the scientific scrutiny of their work (p. 9). In Scotland, however, the Farquharson-Lang Report was recommending that RHBs and local Boards should employ a ‘chief executive’ and moreover felt ‘reluctantly obliged to disagree with the conclusion [of the BMA] that the chief executive…must, inevitably, be a medically qualified person’ (Scottish Health Services Council, 1966, pp. 62-63). Although the Report was publicised in England, this particular conclusion was not (Watkin, 1975, p. 195).
Although Farquharson-Lang had implied that the desirability of a chief executive was widely recognised, in England this was not unanimous. In the same year as Farquharson-Lang, the Salmon Committee (covering Scotland as well as England) reported on the subject of a management structure for senior nursing staff. It concluded that, notwithstanding Bradbeer (see above), senior nurses had insufficient status, and went on to propose a hierarchical structure for the profession, to include a chief nursing officer at Group level (Ministry of Health, 1966, pp. 4, 60-61). The Salmon Report was accepted in principle by the Minister and introduced, initially on a pilot basis, between 1967 and 1972 (Watkin, 1975, p. 318). The Mayston Report soon afterwards applied similar principles to local authority nurses (Watkin, 1978, p. 113).
Nevertheless, Farquharson-Lang found some support from south of the border. In what may well have been a reaction against Salmon, a joint working party of the Institute of Hospital Administrators (IHA) and the King’s Fund criticised Bradbeer on different grounds, accusing it of having ‘failed to grasp the nettle that someone had to be in command of the [hospital] with authority over all the rest of the staff (Joint Working Party, 1967a, p. 24). The report went on to choose the term ‘general manager’ (pp. 32-34) for such a person, responsible to whom would be, amongst others, a medically qualified Director of Medical and Paramedical Services (p. 38 ff). In what transpired to be a prophetic statement, the Working Party noted that its recommendations might not be immediately acceptable to doctors, and might take more than ten years to come about (p. 42).
During the same period, the medical profession itself had begun to look at the relationship between NHS management and hospital medicine; a joint committee of the Ministry of Health and the profession produced in 1967 the first of three ‘Cogwheel Reports’ (so named after the logo on their cover), which urged doctors to recognise their essential interdependence with each other and to set up specialty based ‘divisions’ within hospitals, each sending a representative to a ‘Medical Executive Committee’. The Chairman of this latter body would act as the chief medical spokesman (sic) for the hospital or group of hospitals (Joint Working Party, 1967b, pp. 2-4). The Ministry quickly commended the Report to HMCs and Boards of Governors and medical staff in many districts began to organise themselves either along the lines recommended or some variation of them, though progress was uneven across the country (Watkin, 1975, p. 244). Parallel developments occurred in Scotland as a result of the Brotherston Report (Watkin, 1975, pp. 245-7).
Other health service professions were also interested in management, albeit in a more direct way than the doctors; following Salmon (see above), the Zuckerman (1968) and Noel Hall (1970) Reports recommended management career structures for scientists and technicians, and pharmacists respectively, employed in the NHS (Watkin, 1975, pp. 341-349).
The late 1960s also saw the first applications to the NHS of quantitative management techniques, such as organisation and methods study. Originally used as an aid to planning, such techniques became widespread after 1967 as a means of introducing payment-by-results schemes for hospital manual workers, since current government pay policy required productivity increases in return for pay increases (National Board for Prices and Incomes, 1967).
It will be recalled that the Porritt Report (see above) had suggested a degree of administrative unification of the tripartite structure of the NHS; also, by the mid-1960s consideration was being given to the reorganisation of local government (Alexander, 1982, p. 6). It was not surprising therefore that in 1968 the then Labour Minister of Health, Mr Kenneth Robinson, published a Green Paper (consultative document) on the administrative tructure of medical services (Watkin, 1975, p. 166). As Klein (1983, p. 90) notes, there was a widespread consensus that greater integration of services was required, together with widespread recognition that medical opposition made the transfer of health services to local government a political impossibility. By later in the same year the Ministry had been amalgamated (also in pursuit of greater integration of social policy) into the new Department of Health and Social Security (DHSS) under Mr Richard Grossman, and in 1970 the latter published a second Green Paper in which it was announced that a reorganisation would take place, with health services (defined in terms of the roles of the health professions) to be administered by (in England) some 90 area health authorities, each sharing boundaries with the local government authority responsible for social services (DHSS, 1970, pp. v-vi). Each authority would be advised by a Chief Administrative Medical Officer, a Chief Nursing Officer, a Chief Administrative Officer, and a Chief Financial Officer (DHSS, 1970, p. 20). (Owens and Glennerster [1990, p. 11] are mistaken in their assertion that a chief executive was proposed.)
After the election of a Conservative Government in 1970, the new Secretary of State for Social Services, Sir Keith Joseph, published a White Paper (DHSS, 1972a) setting out the government’s reorganisation intentions; although there were some differences, including the retention of a regional tier of organisation and some explicit references to effective management, the ‘successive proposals … show a remarkable degree of continuity’ (Klein, 1983, p. 91). Consideration of possible management arrangements had already begun, and by this time there was little, if any, support for the notion of a chief executive officer; intellectual leadership in this area lay in the Health Services Organisation Research Unit at Brunei University, whose members and those influenced by them concluded that doctors could not be made managerially responsible to non-doctors (see, for instance, Jaques, 1978, p. 141; Naylor, 1971, p. 33). Moreover, by this time the claims of the health professions to managerial roles of their own had been added to by the Hunter Report, which recommended the creation of a new medical specialty of Community Medicine whose responsibilities would include planning and management (Working Party, 1972, p. 23). As Lewis (1986, p. 116) puts it, ‘doctors had to be persuaded to become actively involved in the management of the service, and it was in this context that the role of the community physician as a “linkman” [sic], inspiring the confidence of both clinicians and administrators, was perceived as crucial.’
It was, however, the so-called ‘Grey Book’ (DHSS, 1972b) which set out the definitive philosophy (even though some of its details in respect of paramedical occupations were later modified) for the management arrangements in the reorganised NHS. Produced by a joint group of DHSS and NHS officers and heavily influenced by the Brunei philosophy of role clarity within organisations, the Grey Book recommended a system of consensus decisionmaking by multi-disciplinary management teams consisting of administrator, treasurer, nurse, and doctors. The reorganised structure of the NHS was implemented, along the reorganisation of local government, in April 1974, by which time a Labour government had been returned to office. (For a more detailed account of the structure, see Levitt, 1979.)
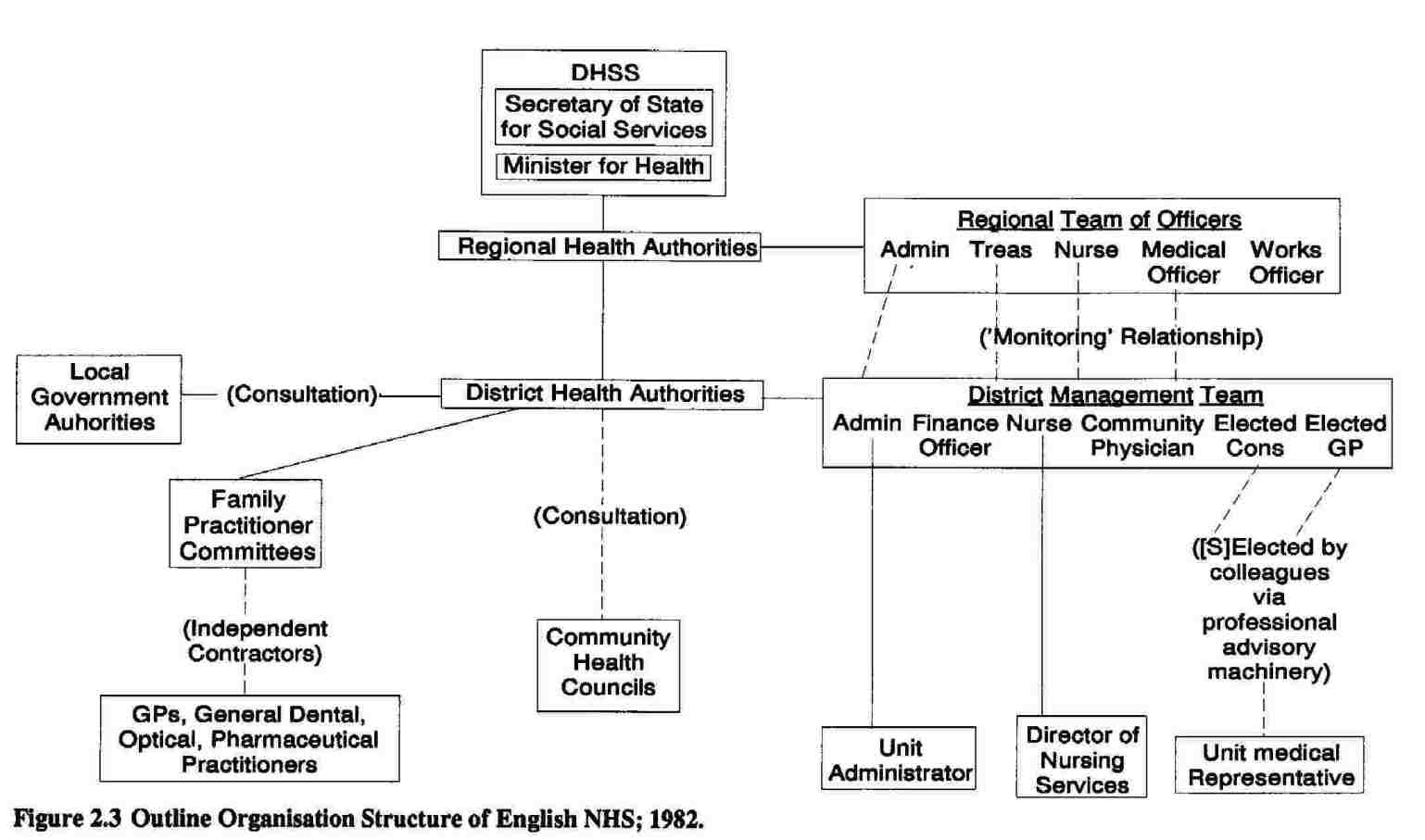
The new arrangements preserved non-elected health authorities (Regional Health Authorities and Area Health Authorities in England) with reduced medical membership; the lower tier was coterminous with the tier of local government responsible for social services, and such area authorities were often divided into two or more non-statutory Districts, each nominally based on the catchment area for a district general hospital. Primary care services were not fully integrated; the contracts of GPs and other independent practitioners were, in England and Wales, held by Family Practitioner Committees (FPC) established by each area authority and consisting of members of the relevant professions and of local and health authorities. FPC staff were managed by a single administrator along the lines of their predecessor Executive Councils. Community Health Councils (CHCs) were created to represent the consumer interest.
Management at Region, Area, and District levels was to be conducted by multidisciplinary management teams. Regional Teams of Officers comprised an Administrator, Treasurer, Nurse, Medical Officer (from the new specialty of Community Medicine: see above) and Works (building, engineering and related professions) Officer. Area Teams of Officers comprised the first four of the above. District Management Teams (and Area Teams where there were no Districts) comprised an Administrator, Finance Officer, Nursing Officer and Community Physician, together with a hospital consultant and GP elected to part-time membership by their respective colleagues.
Although individual team members were to have personal responsibility for their own spheres of work, issues or decisions which were multi-disciplinary or strategic were to be handled collectively. The mode of decision making by such teams was to be consensus, ‘that is, decisions … need the agreement of each of the team members’ (DHSS, 1972b, p. 15; for a review, see Harrison, 1982). It should be noted that, in England, there was no authority relationship between teams at different levels, only between the Authorities themselves, with team members responsible to their respective Authorities. Rather, the relationship between teams was intended to be one of ‘monitoring’; the higher level possessed the right to give advice and obtain information, but not directly to instruct the lower level (Levitt, 1979, p. 48). Disagreements either between teams, or amongst members of a particular team were to be settled by reference to the appropriate health authority, though in practice there was considerable reluctance to use this procedure (Harrison, 1982). The reorganised arrangements are summarised in Figure 2.2.

The 1974 reorganisation can be seen as the culmination of a longstanding trend towards managerial specialisation. Specialist finance and supplies officers had emerged during the 1950s and 1960s, as had specialist managers in such areas as catering, laundry, and domestic work in a period when nurses were increasingly seeking to shed responsibility for ‘non-nursing duties’. The professional building and engineering (‘Works’) function had also developed along with the increasing complexity of health building and technology. In the late 1960s and early 1970s specialist planners and personnel officers had been employed in response, respectively, to activity generated by the Hospital Plan (see above) and to increasing trends in unionisation and employment legislation (Barnard and Harrison, 1986, p. 1220). Reorganisation formalised this trend and added to it managerial hierarchies in a number of health professions not already thus organised: dentistry, chiropody, speech therapy, physiotherapy, occupational therapy and dietetics (Levitt, 1979, p. 144 ff).
The 1974 Reorganisation was completed by the introduction in 1976 of a planning system. This took a cyclical format. DHSS guidelines on national policies and resource assumptions were issued to RHAs, amplified by them and issued to Area Health Authorities, again amplified and issued to District Management Teams (DMTs) who were then responsible for preparing a district operational plan; the resulting plan was fed upwards for approval or review at Area level, aggregated into Area plans fed to Region, and into Regional plans fed to DHSS (DHSS, 1976). The system, though it involved a good deal of consultation with various interests as well as the opportunity for plans at a higher level to be amended as a result of comments from the lower, can be seen as a variety of classic chain-of-command management.
Although substantial numbers of NHS professionals and managers had benefitted considerably from the introduction of the new structure, there was a degree of disillusionment at its complexity and at what proved to be difficult relationships between the various levels of organisation (Ham, 1985, p. 30). This dissatisfaction extended to the relations between DHSS and the NHS, as a result of which the Secretary of State for Social Services, Dr David Owen, invited the Chairmen of three RHAs to report on the matter. The report, completed in the autumn of 1976, concluded that the Secretary of State’s personal accountability to Parliament for the detailed conduct of the NHS, coupled with the Permanent Secretary’s role as Accounting Officer for all its expenditure, led to administrative complexity that was ‘almost totally baffling’ with too much Departmental interference in detail, and excessively slow decisionmaking (Klein, 1976, p. 1804). The remedy proposed was to pass a good deal of the parliamentary accountability to RHAs; by this time, however, Mr David Ennals had succeeded Dr Owen and the issue had become a matter for the newly established Royal Commission (see below).
Moreover the period after 1974 was a difficult one for the NHS for other reasons. Firstly, it was a period of relative economic restraint; in 1976 the Treasury introduced the ‘cash limits’ system of financial allocation to the public sector. This replaced the previous system of allocation in volume terms and meant that NHS hospital and community health services (though not Family Practitioner Services) were no longer automatically protected against inflation in the costs of its manpower or other resources (Klein, 1983, p. 109). A system of central control of management costs was also introduced (Levitt and Wall, 1984, p. 60). The introduction in 1978 of the formula for resource allocation devised by the Resource Allocation Working Party (‘RAWP’) was intended to procure an equitable geographical distribution of health care resources; its application in a period of financial restraint necessarily .entailed a redistribution from some health authorities to others. (For a detailed account see Jones and Prowle, 1984, pp. 93-99.) Secondly, it was a period of increased militancy amongst trade unionists in the NHS; industrial action became relatively commonplace (Barnard and Harrison, 1986, p. 1220). Thirdly, between 1974 and 1976 the Government and medical profession were involved in what Klein (1983, p. 117) describes as ‘the most bitter political struggle since the inception of the NHS’: the battle over an attempt to remove private beds from NHS hospitals. (For a detailed account, see Klein, 1980 and the memoirs of the then Secretary of State, Mrs Barbara Castle [Castle, 1980].) Against this background the Royal Commission on the National Health Service was established in 1976 under the Chairmanship of Sir Alec Merrison.
By the publication of the Commission’s Report in July 1979, a new Conservative government had been elected; the Conservative Party remained in office throughout the 1980s. Like Guillebaud (see above), the Royal Commission was broadly satisfied with the performance of the NHS, though it made a large number of somewhat piecemeal recommendations. Major proposals included the abolition of the Area or District tier (unspecified) of organisation (Royal Commission, 1979, p. 331), the abolition of FPCs (p. 331), and a strengthening of CHCs (p. 157). It also recommended the introduction of a limited list of drugs available for prescription on the NHS (p. 89) though this was soon rejected by the new Secretary of State, Mr Patrick Jenkin (DHSS, 1979).
A good deal of the Government response to the Report was contained in Patients First, a consultative document published in December 1979; this document proposed the abolition of the Area tier and its replacement by statutory District Health Authorities (DHAs) (DHSS and Welsh Office, 1979, p. 9), the retention of FPCs (p. 14), and (somewhat tentatively) the abolition of CHCs (p. 14). The proposals were therefore more than a little different from those of the Royal Commission. Other proposals in Patients First were the simplification of the planning system (p. 18) and greater delegation of authority to ‘units’ (levels of organisation such as hospitals, below the District) which would be managed by an administrator, and a nurse ‘of appropriate seniority to discharge an individual responsibility in conjunction with the medical staff (p. 7); the administrator at hospital level, rather than a District specialist, was to be responsible for functions such as catering and domestic work. The desirability of a ‘chief executive’ was explicitly rejected (p. 7). Experimentation with ‘management advisory services’ within Regions was also announced (pp. 18-19). A later announcement accepted the Royal Commission’s critique of NHS information provision and established an investigation under Mrs Edith Korner (DHSS, 1980a).
Most of the proposed changes were subsequently brought into operation, and are summarised in Figure 2.3. With effect from April 1982 DHAs were created, often, though not invariably, on the basis of the former Districts; as a result, FPCs often covered more than one new DHA. At District level consensus DMTs were retained, whilst the Unit level administrator and nurse were to manage in conjunction with a representative of medical staff (DHSS, 1980b, para 26) in a triumvirate along the lines originally legitimised in the Bradbeer Report (see above). Special emphasis was placed on the coordinating role of the administrator (DHSS, 1980b, para 25). CHCs were retained.
In the meantime (from 1981 onwards) the NHS had been expected by the government to make ‘efficiency savings’; this practice consisted of assuming that health authorities’ outturn expenditure would be less than their nominal budget by a specified percentage, and hence providing an actual budget to match only the assumed outturn. Since such an arrangement provides no controls over where the savings are made, it is no more than a convenient assumption that they result from improved efficiency (Harrison and Gretton, 1984, p. 97). The required figures were 0.2% in 1981-2, 0.3% in 1982-3 and 0.5% in 1983-4 (Ham, 1985, p. 48).
1948-82: behind the formalities
It is evident from the preceding account that a good deal of concern with the management arrangements for the NHS was exhibited by governments throughout the whole period under review. Despite superficial appearances, the underlying view of what constituted good management and how to obtain it was a very particular one. It had two elements: the belief that it was neither appropriate nor practicable to seek managerial control over doctors, and the belief that better management would result from improving the inputs into the management process. Each of these elements is discussed in some detail.
That between 1948 and 1982 there were few aspirations for managerial control of doctors can be illustrated in two ways. Firstly, the position of doctors throughout the various formal changes can be examined. The position of GPs has not merely remained constant since the inception of the NHS in 1948, but since the introduction of ‘panel doctors’ in 1912; their insistence upon remaining as independent contractors and upon precluding even a salary option led to the substitution of Executive Councils for the old Local Insurance Committees. As Willcocks (1967, p. 74) expressed it ‘this old compromise was to be the new compromise’. The compromise was again maintained (in England and Wales) through FPCs in 1974 and 1982 reorganisations, with apparently little attempt to propose alternatives (see, for instance, Medical Services Review Committee, 1962, pp. 56, 88-92; DHSS, 1970, p. 19), except in the case of the Royal Commission discussed above. In short, there was little management involvement with general practice; perhaps the significant exception was the system of prescribing review by which GPs with exceptionally expensive prescribing habits were identified and asked to modify their practice (Johnson, 1962).
In summary, it is hardly surprising that both the Porritt Report and academic commentators noted the lack of friction between managers and GPs (Medical Services Review Committee, 1962, p. 112; Lindsey, 1962, pp. 83-85). Although the 1974 reorganisation affected the position of MOsH as effectively chief executives of local authority health departments, their status was ostensibly preserved (and in the case of some of their former subordinates, enhanced) by the creation of the specialty of Community Medicine.
In hospital medicine too, doctors were not challenged by the formal organisation, which, despite the recommendations of Farquharson-Lang and the (then) Institute of Hospital Administrators (IHA) (see above) remained collegial in character throughout the period under examination. The clearest manifestation of this was the creation in 1974 of consensus teams: a means of providing the formal right of veto to a group which possessed it in practice anyway (Harrison, 1982, pp. 379-380). Although the post-1974 Health Authorities had a smaller medical membership than their predecessors, this was more than compensated by the formal involvement of doctors elsewhere in the management structure. It is significant that consultant contracts of employment remained at RHA level, (except in the case of Authorities responsible for undergraduate medical education), and that no attempt to introduce American models of hospital management by clinical ‘chiefs of service’ was made. (This was considered and rejected by the Bradbeer Report: Central Health Services Council, 1954, pp. 27-30). Indeed, hospital beds were allocated to individual hospital consultants in a form of quasi-ownership, giving the individual virtually unilateral control over their use and utilisation. Moreover, the right to engage in private practice, a major source of uncertainty for managers, was retained, and indeed was enhanced in 1980 (British Medical Journal, 15 September, 1979, p. 685).
A second way of illustrating the adherence of successive governments to the notion of clinical freedom is to examine the content of official policy documents; at all periods in the history of the NHS such documents have made explicit references either to the notion itself, or to a model of management which, it is made clear, centres upon providing facilities for professionals. Such references indeed predate the creation of the Service; the 1944 Coalition government White Paper on a National Health Service stated that ‘whatever the organisation, the doctors taking part must remain free to direct their clinical knowledge and personal skill for the benefit of their patients in the way in which they feel to be best’ (Ministry of Health, 1944, p. 26). These sentiments were on several occasions echoed by Aneurin Bevan, Minister of Health from 1945 to 1951: (see quotations in Allsop, 1984, p. 17 and Watkin, 1975, p. 139). If such a view underpinned the creation of the NHS, it also underpinned its first reorganisation; the Crossman Green Paper (see above) set out a fundamental principle that ‘the Service should provide full clinical freedom to the doctors working in it’ (DHSS, 1970, p. 1; see also Allsop, 1984, p. 29). The Secretary of State’s foreword to the Conservative White Paper which set out the firm plans for Reorganisation assured the reader that
The organisational changes will not affect the professional relationship between individual patients and individual professional workers on which the complex of health services is so largely built. The professional workers will retain their clinical freedom -governed as it is by the bounds of professional knowledge and ethics and by the resources that are available – to do as they think best for their patients. This freedom is cherished by the professions and accepted by the Government. It is a safeguard for patients today and an insurance for future improvements (DHSS, 1972a, p. vii).
The subsequent Grey Book (see above) went further in linking management to medicine:
…. the objective in reorganising the NHS is to enable health care to be improved. Success in achieving this objective depends primarily on the people in the health care professions who prevent, diagnose and treat disease. Management plays only a subsidiary part, but the way in which the Service is organised and the processes used in directing resources can help or hinder the people who play the primary part (DHSS, 1972b, p. 9).
Nor had the philosophy for what was to become the 1982 reorganisation changed much; Patients First had the following to say:
It is doctors, dentists and nurses and their colleagues in the other health professions who provide the care and cure of patients and promote the health of the people. It is the purpose of management to support them in giving that service (DHSS and Welsh Office, 1979, pp. 1-2).
Such quotations are, of course, selective. The same documents also make references to such matters as the need for efficiency, but what is striking is that they are careful never to imply that doctors might need to become more efficient; the inference is rather that it is other, unspecified, groups which need to be controlled in order to maximise resources for medical care. Thus the above quotation from Patients First continues: ‘The efficient management of the Service is therefore of the highest importance, not least when resources are tight. The more economical it can be, the more resources there will be for patient care’ (DHSS and Welsh Office, 1979, p. 3). It is also true that some of the above documents acknowledge that resources are limited and that priorities need to be established. But here again, there is no challenge to medical autonomy; rather, it is assumed that agreed priorities will somehow emerge from discussions. Thus the Grey Book speaks of mechanisms by which doctors can ‘contribute more effectively to … decision making’ (DHSS, 1972b, p. 10), whilst Patients First refers to machinery to ensure that the doctor’s voice is fully heard’ (DHSS and Welsh Office, 1979, p. 17).
A third way of demonstrating the lack of a managerial challenge to doctors is to look at management practice as revealed in the extensive contemporary empirical research literature. It is clear from this that policymakers and managers were not the most influential actors within health authorities. A number of case studies have instanced the influence of hospital Consultants on specific decisions. Kogan’s research for the Royal Commission on the NHS documented the case of a decision to transfer the responsibility for biomedical engineering to the Works Officer, twice overturned as a result of medical objections (Kogan et al, 1978, p. 129 ff). This ability to veto change was capable of persisting over long periods; Rathwell has shown how, in one health authority, attempts to settle the number and distribution of hospital beds for the elderly remained unsuccessful, as a result of medical disagreements, over a period of four years. Even a severe winter, and consequent admissions crisis did not aid resolution, which had still not been achieved at the conclusion of the research (1987, Chap 4). In another study, Linstead has shown how Consultant physicians, on this occasion in alliance with another professional group, were able to veto proposed changes in training arrangements for hospital technicians (1984, p. 11). A further example of the obstructive ability of the medical profession is provided in Forte’s (1986, p. 43) case study of one district; clinicians were able to delay the implementation of the whole operational plan by withdrawing their earlier agreement to acute service ‘rationalisations’. The ability of doctors to impose their definition of a particular situation upon others has been well illustrated by Ham’s example of proposed alterations to bed allocations between hospitals being seen as a lack of suitable case material for medical teaching rather than as a need to provide a good service for the elderly (Ham, 1981, pp. 147-149).
Perhaps more important than such single instances are findings which show the influence of the medical profession on the strategic shape of services delivered by the NHS. Haywood and Alaszewski (1980, pp. 104-106) have examined the pattern of inputs to, and outputs from, the NHS during the 1970s, showing that whilst real resources available (staff, money) rose considerably, output in terms of the number of cases treated (as inpatients or outpatients) rose much more modestly. Although this discrepancy is to some extent due to improvements in staff conditions of employment, the major explanation is increased intensity of diagnosis and treatment, a conclusion confirmed by increases in the workload of pathology, radiology and physiotherapy departments, and by the rising ratio of total attendances to new outpatients. This can be seen as implying a decision, not taken by politicians or managers but by individual clinicians, to devote the majority of additional resources to greater intensity of care rather than to treating larger numbers of patients. That is, the decisions which underlie these aggregates are individual clinicians’ decisions about admission, diagnosis, therapy, and discharge. (It should be appreciated, of course, that these conclusions involve no judgement about the value or otherwise of such trends.) These observations, together with an analysis of failures to implement national priorities, also led the authors to comment that ‘the power of [central government] to effect change is limited, even when only a modest change in emphasis is envisaged’ (p. 61), a conclusion supported in Stocking’s study of the pattern of introduction of day case surgery (1985, pp. 223-228).
This strategic influence of the medical profession can also be discerned in the arrangements for the education and supply of professional manpower, a crucial resource for the NHS. Harrison’s study of this area concluded that the arrangements were to varying degrees dominated by professional organisations rather than by managers or even by DHSS. Underneath a complex surface pattern of many official and professional bodies was, however, a dominant medical influence; ‘the whole mechanism is not nearly as pluralistic as the mere listing of the bodies involved may convey; not only is the medical profession dominant within most of them, but the same sections of the profession … are represented within many’ (Harrison, 1981, p. 94). Kogan et al (1978, p. 174) have pointed out that decisions by bodies such as the Royal Colleges can result in the non-recognition of hospital training posts which in turn can result in hospital closure.
Conclusions about strategic medical influence are also supported by research into the management and policy process in specific NHS Regions. Elcock and Haywood (1980, pp. 77, 97) note that ‘in both Regions, the medical profession fought vigorously against changes in priorities intended to favour the [official priority groups of patients] at the expense of the acute sector.’ Nor do such conclusions relate solely to the post-reorganisation period. Ham’s historical study concluded that legal and financial controls were not an effective means of securing change; ‘the capacity of the central [government] department to ensure that its policies were implemented was limited’ even though ‘its style became more promotional and interventionist as the 1960s progressed’ (Ham, 1981, pp. 191-192). Stocking’s 1985 study of such longstanding central priorities as Regional Secure Units and the revision of waking times for hospital inpatients confirms this conclusion.
How far are such conclusions supported by evidence about the perceptions of NHS managers? In an interview study of eighteen management teams, Schulz and Harrison found that
on twelve…teams…there was overwhelming agreement that consultants had the primary influence on the pattern of health care delivery in the area. Only two teams ascribed the primary influence to themselves, with the remaining four … either divided on the issue or ascribing equal influence’ (Schulz and Harrison, 1983, p. 33).
The same respondents reported that RHAs and DHSS were relatively uninfluential (pp. 30-33). These perceptions were replicated in another interview study of administrators, medical and nursing officers, who were ‘particularly aware of the power consultants had to cause and prevent change. They saw the individual professional largely in control’ (Glennerster et al, 1983, p. 260).
The chairpersons and members of health authorities were no more influential, either individually or collectively, than the managers they employed. For instance Brown et al (1975, pp. 11-14) found that managers gave the authority members very little information about ongoing issues about which there were disagreements. Haywood’s initial study of six DHAs concluded that ‘in general, there were few decisions influenced by members’ (Haywood, 1983, p. 44), a finding confirmed in a follow-up study which also indicated that, within HA membership, chairpersons were relatively influential (Haywood and Ranade, 1985). These findings have been confirmed by Ham; the general lack of member influence on policy was partly the result of medical influence manifest through ‘creeping development in acute specialties’ (1986, pp. 123-126). Scottish members similarly lacked influence on resource allocation (Hunter, 1980, p. 198); one respondent perhaps summed it all up when he said ‘as far as I can see, the health board is a rubber stamp’ (Hunter, 1984, p. 50). Managers interviewed by Glennerster et al (1983, p. 261) and Schulz and Harrison (1983, p. 30) confirmed these assessments of member weakness.
If managers were not pre-eminently powerful, they were not predominantly proactive either. The process of planning is where, perhaps, one might most expect to find proactive behaviour; studies of NHS planning show that this was rarely possible. For instance, Barnard et al (1979, Vol 3, p. 16) document the way in which a London health authority’s attempts to assess the health care needs of its population were rapidly abandoned in order to produce ‘defensive’ information to demonstrate the perceived unfairness to the authority of the RAWP formula. The northern health district studied by Forte (1986, pp. 24-25) experienced similar difficulty in sustaining proactive behaviour. In Scotland, Hunter found ‘… plans thwarted by the flare-up of a crisis, such as occurred in both [health boards where fieldwork was conducted] over nursing staff establishments’ (1980, p. 151), whilst even within the Scottish Home and Health Department planning was reactive and ad hoc (Wiseman, 1979, pp. 106-107).
It might also be expected that proactive behaviour would be found in the activities of chief officers of health authorities, and the management teams of which they were members. In their study of District Administrators, Stewart et al (1980, p. 76) note, however, that few were able to play the more proactive roles of shaping plans, innovating new practices or of managing the total organisation; rather the evidence (pp. 149-171) of how the research subjects spent their days shows little sign of interest in strategic issues but a preoccupation with ad hoc referrals of issues. Nor was the content of management team agendas any different; Schulz and Harrison (1983, p. 37) note that a major item of team work was ‘tackling of issues which in some way presented themselves as problems to the team or its members’. Hay wood’s systematic classification of the agenda items of several management teams shows the prevalence of non-strategic items (Haywood, 1979, pp. 54, 57); 90% of items consist of information exchange, deciding to whom issues should be referred (‘process’), or routine decision-making. Yet the teams were created in order to take ‘decisions for the totality of health care’ (DHSS, 1972b, p. 15). Haywood summarises by describing chief officers as ‘directors of process…. reactors rather than initiators ….’ (1979, p. 59).
If top managers were reactive, it is hardly surprising that their subordinates perceived their own jobs in the same way. Harrison, Haywood and Fussell took a population of upper-middle NHS managers all attending university continuing education courses (and perhaps therefore to be expected to be more textbook-oriented than the average) and gave them a free choice of how to make a written characterisation of their own job roles. The respondents overwhelmingly chose to typify their jobs as tackling problems referred to them by other actors who had expressed some dissatisfaction; the main consideration was to satisfy the complaint without creating further dissatisfaction elsewhere (Harrison, Haywood and Fussell, 1984, p. 186).
It is not surprising, therefore, that managers and doctors were rarely in conflict (Green, 1975). Moreover, studies of managers’ behaviour indicate that their problem-solving efforts were strongly focused within the organisation rather than outwards. Stewart et al (1980, pp. 172-7) traced all the issues with which District Administrators dealt over a three-day period, almost none of which did not originate within the health authority. Similarly, all the examples of decisions quoted in Hay wood’s study (1979, pp. 57-8) are internal in origin. The Howe Report into the scandal at Ely Hospital had shown a closed community with no awareness of standards elsewhere and an inbuilt resistance to complaints (Committee of Enquiry, 1969, p. 115 ff) (and this was not the first or last such scandal), so that Thompson’s comment from a study conducted in the early 1980s is apposite:
One of the more sobering features of the study was an apparent lack of interest in consumer responses, even the relevance and significance of patients’ complaints (Thompson, 1986, p. 57).
The same kind of introversion is evident in the responses to the study by Harrison, Haywood and Fussell; administrators’ agendas were largely defined by other actors within the health authority, whilst the nurses’ agendas seemed dominated by problems of organisational formalities. The authors concluded that:
the…study suggests…that the typical dissatisfactions which NHS managers perceive as problems are related not to formal organisational objectives as set out in statute, nor…to the kind… (such as quality, access, acceptability and equality) suggested by the Royal Commission on the National Health Service, but to organisational process and internal relationships… The material counsels against any expectations of logical or causal links between formal organisational objectives, managers’ perceptions, and managerial action (Harrison, Haywood and Fussell, 1984, p. 1987).
The preceding few pages have shown NHS management in the 1950s, 1960s and 1970s as it both was and was supposed to be. Managers were, and rightly so, ‘diplomats’ (Harrison, 1988a, p. 51). Rather than being responsible for shaping and controlling the service, they were engaged in
… a process concerned to conciliate, in as coordinated a fashion as possible, all the sub-groups within an organisation (Harrison and Hallas, 1979a, p. I486)… In the context of diplomacy there is rarely a meaningful overall objective; more often there is a set of partially, or sometimes completely, contradictory objectives held by groups or individuals (1979b, p. 1523).
The other dominant assumption about management in the period, it will be recalled, was that improvements would come from changes in inputs to the management process, particularly changes in organisational structure and in training provision; this view was not, of course, peculiar to the NHS and, for instance, underpins the Fulton Report (Committee on the Civil Service, 1968). Better management career structures were seen as the answer to the problem, almost irrespective of what the problem was. Indeed, in the extreme case the absence of managerial careers was seen as the problem; the Salmon Report took it as axiomatic that nurses’ status was too low, and all its proposals flowed from this (Ministry of Health and Scottish Home and Health Department, 1966, p. 7). Increasing managerial specialisation (see above) was another manifestation of the same assumption, as was the increased attention paid to training and education of managers (see, for instance, King’s Fund Working Party, 1977).
Claims for managerial roles and equality of status with administrators therefore became the strategy by which the health professions other than medicine sought to advance themselves;
each professional group – which was of course heavily represented on the working party concerned with its particular specialty – was naturally ready to welcome a form of organisation which provided more numerous and more lucrative opportunities of promotion for its members (Watkin, 1975, p. 349).
Both the Royal Commission (1979, p. 29) and, more critically, Brown (1979, p. 31) agreed that consensus management teams were both a reflection and a cause of such professional aspirations to managerial autonomy.
Of course, these claims did not go entirely without challenge; the content of the Farquharson-Lang and Institute of Hospital Administrators Reports has already been discussed. But as the 1974 reorganisation approached, such formal opposition became more muted and disappeared. Its last vestige may be found in Naylor’s influential study of the possible forms of new organisation; having dismissed the possibility of management control over clinicians, he continues:
….could the remainder of the health professions and all the other groups of workers be subordinated to one director? ….the answer is probably in the affirmative [though]….as the strength of the other health professions grows nearer to the doctors, there may be pressure for equality of status (Naylor, 1971, p. 33).
This concern with managerial inputs coincided with the aspirations of various occupational groups; the professions other than medicine can in particular be seen to have derived considerable benefits. The corollary of concern with inputs is a lack of concern with outputs, that is, a lack of evaluation. Such a lack of evaluation is very much evident in the empirical studies of NHS management to which reference has already been made. For instance, studies of planning show a strong emphasis on hospital beds; thus Rathwell (1987, Chapter 4) has shown how planning for the elderly in one authority was largely confined to beds, notwithstanding the existence of official priority for community care. (In the same study, planning for the mentally handicapped, where no beds existed, was not so constrained.) Similarly Ham (1981, p. 147) has shown how in another city the problem of the elderly were perceived as a problem of ‘bed blocking’, and Glennerster et al (1983, p. 261) have shown the importance with which national norms were treated. Planning options also showed a strong emphasis on what Brown et al termed ‘shopping lists of deficiencies’ in existing services:
When the…. district teams submitted their…. priorities for long-term development… .over half concerned the development of primary care ….[but] when it came to concrete proposals….’community’ projects did not fare quite so well…. They received….their pre-organisation share of-the share-out (Brown et al, 1975, pp. 103-104).
According to Thompson (1986, p. 20), things had not changed by the 1980s. Such ad hoc planning was also to be found in Scotland (Wiseman, 1979), though planning documents sometimes sought to conceal this by the inclusion of large quantities of symbolic information unrelated to actual proposals for change (Schulz and Harrison, 1983, p. 38). Glennerster et al (1983, p. 264) note that most of the respondents in their study ‘still thought of planning as what to do with the increment’ and also provide an insight into why this should be so; ‘in theory, people favoured a change in priorities but only on the basis of “you can do it so long as you don’t touch me” ‘ (p. 260).
A further characteristic of planning options follows closely from this. Hunter (1980, pp. 145, 184) notes that development funds were not merely regarded as important, but for many actors were the answer to planning problems; the tendency was always to seek more resources rather than to question the value of existing resource use, most developments were the result of building schemes, and most also meant ‘more of the same’. He goes on to explain:
At best, allocations of [development funds] reflected a compromise between…. simply plugging gaps in existing services and…. initiating new services…. Often there was no choice…. Pressures from existing services presented officers with little or no alternative but to plough more funds into them to relieve the pressures (Hunter, 1980, p. 184, emphasis added).
The same absence of evaluation or review was prevalent in managerial behaviour more generally. The management teams in Schulz and Harrison’s study allocated resources incrementally; when asked individually about their objectives, respondents overwhelmingly replied that they were concerned, firstly, to keep existing services intact, and, secondly, to respond if possible to internal demands for expansion. Movement towards national priorities came only in third place (Schulz and Harrison, 1983, p. 37). Nor surprisingly, therefore, Barnard et al (1979, Vol 3, p. 32) found that ‘little attention was paid to collecting information on resource use…. or on outcomes’. To some extent, however, the illusion of scrutiny was maintained by such devices as frequent visits to institutions by senior officers, though these were in practice quite un-critical in approach (Schulz and Harrison, 1983, p. 37). In a more recent study Thompson (1986, p. 57) was surprised to observe ‘the noticeable absence of any systematic monitoring…. of policy formulation and implementation’.
The same approach to management was manifested in Harrison, Haywood and Fussell’s study of upper middle managers; respondents were given the opportunity to choose a problem related to their work, and to state how they would tackle it and what would be a satisfactory solution. The tendency was for responses to ignore the last section of the brief, that is to treat the action taken to attack the problem as being a solution in itself, rather than to suggest criteria by which the results of that action might be judged (1984, p. 186). In the light of this varied evidence, it is difficult to disagree with the conclusion that the managerial changes of the 1970s failed to make NHS decisionmaking less incremental (Brown, 1979, p. 205; Lee and Mills, 1982, p. 179).
It is now possible to summarise the character of NHS management before 1987, that is, before Griffiths. Firstly, rather than conforming to textbook models of authoritative, proactive management (Stewart, 1979, pp. 66-7), the NHS manager was for the most part a diplomat acting to smooth out conflicts and procure resources with which professionals could perform their tasks. It follows that there was relatively little medical-managerial conflict (Green, 1975) and that authors such as Heller (1979, pp. 1, 45) and Petchey (1986, p. 100) are mistaken in asserting that such conflict was a major determinant of the shape of the service. And whilst Klein (1985) is no doubt correct in asserting that doctors and managers had different value systems, there was also considerable overlap and homogeneity (Schulz and Harrison, 1983, p. 44; Brown, 1979, p. 191).
Secondly, despite a certain amount of discontent and frustration amongst managers (Klein, 1984, p. 1708; Stewart et al, 1980, pp. 30, 66, 113; Haywood et al, 1979, pp. 26, 35, 39; Schulz and Harrison, 1983, p. 17; Fairey et al, 1975, pp. 25-6), it was widely understood that the prevailing situation was pragmatically desirable (Naylor, 1971, p. 33; Jaques, 1978, p. 141; Kogan et al, 1978, p. 45 ff). There seems to be little evidence for the inference made by Haywood and Alaszewski (1980, p. 87) that managers suffered from the delusion that they had, or ought to have, decisive control of the service. It is true that there were managers who displayed exceptional behaviour; some were proactive (Stewart et al, 1980, p. 78 ff; Schulz and Harrison, 1983, pp. 40-3; Rathwell, 1987, ch. 4). But these were minority examples.
Overview: 1982 and after
General management was not the first management initiative to mark a radical departure from the preceding management arrangements. On 22 January 1982, about nine months before the Griffiths Inquiry was commissioned, the Secretary of State for Social Services, Mr Norman Fowler, announced arrangements to ‘improve accountability’ in the NHS. There were two elements to these arrangements: a review process and a set of performance indicators (PIs).
The review process was intended to secure greater adherence to national policies and priorities than had previously been the case;
… each year Ministers will lead a Departmental review of the long-term plans, objectives and effectiveness of each Region with the Chairmen of the Regional Authorities and Chief Regional Officers. The aims of the new system will be to ensure that each Region is using the resources allocated to it in accordance with the Government’s policies – for example giving priority to services for the elderly, the handicapped and the mentally ill – and also to establish agreement … on the progress and development which the Regions will aim to achieve in the ensuing year (DHSS, 1982a, pp. 1-2).
A similar process was to take place between regional authorities and DHAs within the region. The new process commenced immediately, in January 1982, with a review of the Mersey Region.
Performance Indicators were to be developed on a pilot basis in the Northern Region. To be employed in conjunction with the review process, they would
….enable comparison to be made between districts and so help Ministers and the Regional Chairmen…. to assess the performance of their constituent…. authorities in using manpower and other resources efficiently (DHSS, 1982a, p.2).
Unlike earlier attempts to use comparative data (see, for instance, Yates, 1983), the new indicators were therefore to be compulsory. The first national (English) package of indicators (DHSS, 1983a) was issued on 22 September 1983, in a form which allowed any health authority to be compared with all others in terms both of absolute values of the indicators used and of rankings within the region and the country. The package contained some seventy indicators relating to clinical work, finance, manpower (sic), support services and estate management, all constructed from already available data. The clinical indicators related mainly to the use of clinical facilities within broad specialty groups, rather than to the outcomes of treatment, consisting of such efficiency measures as average length of hospital stay, throughput of patients per bed per annum, turnover interval between cases occupying a bed, and the ratio of return outpatient visits to new outpatients. They were, however, all measures which are largely determined by the aggregate of doctors’ behaviour rather than by managers’ decisions.
Less than two months after the original review process/ performance indicator announcement, Mr Fowler announced two further initiatives (DHSS, 1982b). Firstly, a national enquiry was established with the aim of ‘identify[ing] underused and surplus land and property, and, where appropriate dispos[ing] of it’ (p.l). The subsequent Ceri Davies Report (DHSS, 1983b) recommended a system of notional rents for NHS property as the basis of a performance measure of estate utilisation and the disposal of unused and underused assets; it was accepted by the Government in November 1983 (DHSS, 1983c). The other initiative was the experimental use of private firms of accountants to audit the accounts of health authorities (DHSS, 1982b).
Only three weeks from this announcement, on 1 April 1982, came the announcement of yet another initiative: the extension of ‘Rayner Scrutinies’ from the Civil Services to the NHS. Named after Sir Derek Rayner, Managing Director of Messrs Marks and Spencer and part-time efficiency adviser to Government, such scrutinies involved intensive study of a particular area of expenditure by an officer seconded from normal duties (DHSS, 1982c). The chosen topics were later announced as vacancy advertising, the storage of supplies, catering costs, the cost-effectiveness of meetings, NHS residential property, the recovery of aids loaned to patients, ambulance service control systems, collection of income due to health authorities, and the administration of project briefs for hospital building schemes (DHSS, 1982d).
Further initiatives followed. On 27 August a Review of NHS Audit arrangements was announced; the results, promulgated a year later, emphasised the need for greater attention to be given to ‘value for money’ rather than to narrow financial propriety (DHSS, 1982e; 1983d). On 7 October 1982 it was announced that a firm of chartered accountants were to study the possibility of cash-limiting Family Practitioner Committee budgets (DHSS, 1982 f). On 19 January 1983 central control of NHS manpower numbers was announced (DHSS, 1983e) and on 4 February came the first public suggestion that the Government was seriously considering restrictions on doctors’ rights to prescribe (DHSS, 1983 f); in November 1984 the withdrawal occurred from NHS prescriptions of a range of proprietary drugs which had been previously freely available (DHSS, 1984a). On 8 September 1983, health authorities were instructed to engage in competitive tendering for laundry, domestic, and catering services (DHSS, 1983g), and on 19 December the Minister for Health announced proposals to place restrictions on the use of deputising services by off-duty GPs (DHSS, 1983h).
On 3 February 1983, towards the conclusion of the spate of initiatives outlined above, a development occurred which was to crystallise and symbolise the post-1982 policy for managing the NHS. The Secretary of State announced that
Four leading businessmen are to conduct an independent management Inquiry into the effective use and management of manpower and related resources in the National Health Service…. we are setting the Inquiry two main tasks; to examine the way in which resources are used and controlled inside the health service, so as to secure the best value for money and the best possible services for the patient [and] to identify what further management issues need pursuing for these important purposes…. Mr Griffiths has not been asked to prepare a report…. we could simply have set up another Royal Commission and then sat back for several years to await its lengthy report, but on past experience that would not lead to effective action. Instead, we have gone straight for management action, with the minimum of fuss or formality (DHSS, 19831).
Mr Roy Griffiths was Deputy Chairman and Managing Director of Messrs J Sainsbury, and his colleagues the Personnel Director of British Telecommunications (Michael Bett), Group Finance Director of United Biscuits (Jim Blyth) and Chairman of Television South West (Sir Brian Bailey, a former NALGO official). The Team’s final report, in the form of a twenty-four page letter (NHS Management Inquiry, 1983), was sent to the Secretary of State on 6 October 1983, the full text being made public on 25 October.
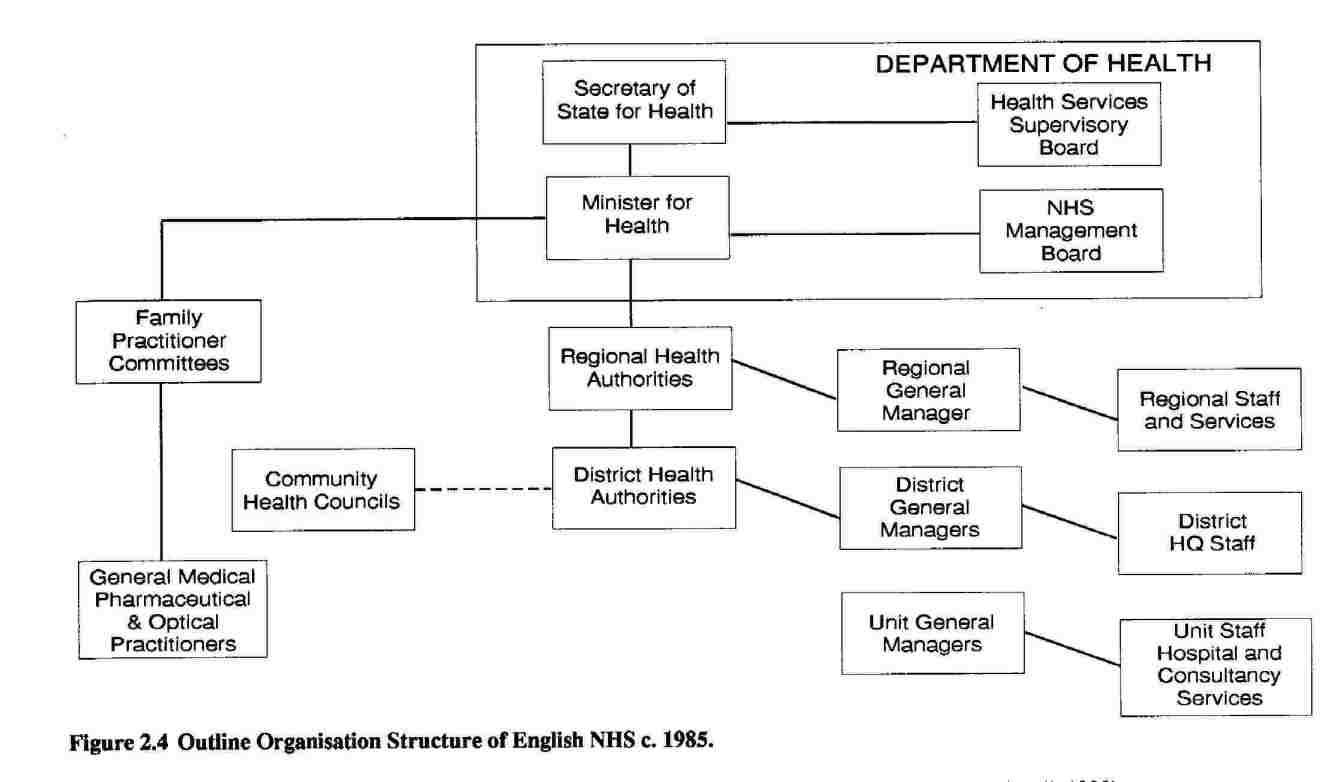
The Team’s recommendations were baldly stated in eight pages. Firstly, changes within DHSS were proposed: the creation of a Health Services Supervisory Board (chaired by the Secretary of State, and including the Minister for Health, the Permanent Secretary, the Chief Medical Officer, the Chairman [sic] of the NHS Management Board [see below], and two or three non-executive members with general management skills and experience) with strategic responsibility for the objectives and resources of the NHS, and, responsible to it, a full-time, multiprofessional NHS Management Board to oversee implementation of the strategy (NHS Management Inquiry, 1983, p.3). Hence the Management Board would assume all pre-existing NHS management responsibilities located in DHSS, and its members would include some from outside the Civil and Health Services (p.4). Incentives and sanctions in management were held to require attention, and accordingly great stress was placed on the role of a personnel director as a Board member (pp. 4, 7).
Secondly, general managers were proposed for RHA, DHA and Unit levels of organisation; regardless of discipline, such persons were to carry overall management responsibility for achieving the relevant health authority’s objectives, and were to have substantial freedom to design local organisational structures. Functionally-based management structures were to be minimised and day-to-day decisions taken at Unit level rather than higher up the organisation (pp. 4-5).
Thirdly, the review process (see above) was to be extended to unit level, and efficiency savings (see above) replaced by ‘cost-improvement programmes’, aimed at reducing costs without impairing services (pp. 4-5).
Fourthly, clinical doctors were to become more involved in local management. The prime vehicle for this was a proposed system of ‘management budgets’: the allocation of workload-related budgets to consultants (pp. 6-7). The locus of consultant contracts was, however, to remain unchanged (p. 19). Finally, the Report urged that more attention be paid to patients’ and community opinion, expressed through both Community Health Councils and market research methods (p. 9). The Report also spoke approvingly of some of the earlier initiatives such as performance indicators, the disposal of surplus property, Rayner Scrutinies, and annual reviews (pp. 1, 8, 13).
On the same day as the release of the Report, the Secretary of State for Social Services told the House of Commons that the Government welcomed the thrust of the recommendations and accepted those applicable within the DHSS; the remainder were to be the subject of a short period of consultation (DHSS, 1983J). In the event, this period included an investigation by the House of Commons Social Services Committee, whose conclusions were by no means wholly supportive (Social Services Committee, 1984). In general, the comments of medical, nursing and ancillary staff representative organisation were unfavourable (see Harrison, 1988b) whilst those of administrators’ and treasurers’ organisations were favourable. Unsurprisingly, most comment was directed at the proposal to appoint general managers.
On 4 June 1984, the Secretary of State promulgated the Government’s decisions on the Griffiths Report (DHSS, 1984b). Some changes, including those within DHSS and pilot schemes for management budgets, were confirmed as in progress already (p.l), and the principle of individual general managers in place of consensus teams accepted:
….The Management Inquiry Team recommended that the general management function should be clearly vested in one person (at each level) who would take personal responsibility for securing action. We accept this view; and believe that the establishment of a personal and visible responsibility…. is essential to obtain a guaranteed commitment…. for improvement in services…. In reaching this conclusion, we do not undervalue the importance of consensus in a multi-professional organisation like the NHS. But we share the Report’s view that consensus, as a management style, will not alone secure effective and timely management action, nor does it necessarily initiate the kind of dynamic approach needed in the health service to ensure the best quality of care and value for money for patients (p.2).
General managers were therefore to be appointed at Regional, District and Unit levels of organisation by the end of 1985; the posts were to be open to NHS managers of all disciplines, to doctors, and to persons from outside the Service. Appointments were to be on the basis of fixed-term contracts of three to five years with renewal for further fixed terms by mutual agreement and, by implication, dependent upon an assessment of the incumbent’s performance. Any costs incurred by appointments were to be offset by savings on other management costs (Appendix C).
The Health Services Supervisory Board and the NHS Management Board took a slightly different form from that envisaged in the Griffiths Report. Pressure from the nursing profession led to the early addition of the DHSS Chief Nursing Officer to the Supervisory Board (DHSS, 1984c), and only one non-executive outsider, Mr Griffiths himself, was appointed (Chaplin, 1987, p.2). Mr Victor Paige, formerly Chairman of the Port of London Authority was appointed as Chairman of the NHS Management Board in December 1984 (DHSS, 1984d), but resigned in June 1986 (DHSS, 1986a; Davies, 1986a). A revised arrangement resulted, with Mr Tony Newton, the Minister for Health as Chairman of the Management Board, (by then Sir) Roy Griffiths as Deputy Chairman (with direct access to the Prime Minister), and Mr Len Peach (Personnel Director of Messrs IBM [UK] as Chief Executive (DHSS, 1986b). The composition of the Management Board varied during 1984 to 1987, with roughly one-third of its members from commercial backgrounds, one quarter from the NHS, and the remainder from the Civil Service (Chaplin, 1987, p.2; Health Service Journal, 29 January 1987). The Management and Supervisory Boards remained a part of DHSS rather than separate tiers of management. (For an outline of the then internal organisation of DHSS, see Health Trends, 1986, Vol 18, pp. 32-36.)
General Managers were appointed by RHAs and DHAs and at Units, though subsequent general manager appointments were on rolling, rather than fixed-term contracts, and a system of individual performance review (IPR) and performance-related pay (PRP) were introduced (DHSS, 1986c, 1986d). The Review Process operated at all levels of the service, and was modified to consist at regional level of a management meeting between the NHS Management Board and Officers of each RHA at which progress on plans and cost-improvement programmes is reviewed; this was followed by a ministerial meeting with chairpersons of individual RHAs at which more strategic and long-term issues are discussed, along with major issues arising from the management meeting (Mills, 1987).
Management budgets were not introduced on a widespread basis. Four health districts were chosen as ‘demonstration sites’ even before the publication of the Griffiths Report, but despite the involvement of management consultants not all of these were successful at the technical level of establishing the necessary information systems. Moreover, they did not gain the widespread support of clinicians (see, for instance, Arthur Young, 1986a; 1986b). A second generation of demonstrations began in 1985; it was intended that this would pay more attention to the behavioural aspects of such systems (DHSS, 1985a). Nevertheless, there remained problems in convincing doctors of the value of the innovation and a further set of pilots proved to be necessary; these were launched in November 1986 under the new rubric of ‘resource management’ (DHSS, 1986e). (For a review of the various pilots, see Pollitt et al, 1988; Buxton et al, 1989). Figure 2.4 summarises the post-Griffiths structure.
It may be noted that the general context of developments in information technology during the early 1980s met a necessary, though not sufficient, condition of several of these managerial developments. It is hard to imagine, for instance, a system of dispersed management budgets without computerised information (Arthur Young, 1986a, p. 1), whilst the second, computerised, package of performance indicators was much more ‘user-friendly’ (and hence, likely to be used) than the original manual of typescript tables (Fairey, 1985). The role of such technology in public sector management has been neatly summarised by Pollitt:
Finally, computers: they have played a significant permissive role in the introduction of performance assessment systems. The advent of dispersed, multi-access systems with cheap desk-top VDUs has permitted the storage, rapid retrieval and display of the vast quantities of data that most performance assessment schemes appear to need. Computers obviously didn’t produce the wave [of such schemes in the public sector] but they have allowed it to flow more swiftly and to deposit less paper (Pollitt, 1986, p. 160).
Conclusion: radical but not novel
General management was radical in two senses. Firstly, it reversed a strong trend towards multidisciplinary management by groups of equals. Multidisciplinary management at hospital level had been introduced in 1948 and subsequently endorsed by Bradbeer. The advocacy of Salmon for such an arrangement to be extended to ‘group’ level was successful, and the consensus teams introduced in 1974 represented the apotheosis of such a view. The fortunes of the occupations other than administration, nursing and medicine were more variable over time, initially prospering through reports such as Noel Hall and Halsbury (see above), and through the 1974 Reorganisation, but later losing a little ground as a result of the 1982 Reorganisation’s suspicion of District-level ‘functional’ management.
Moreover, the reversal was a sudden one. Patients First, the policy document which underpinned the 1982 Reorganisation was unequivocal about the desirability of team management:
The Government has rejected the proposition that each authority should appoint a chief executive responsible for all the authority’s staff. It believes that such an appointment would not be compatible with the professional independence required by the wide range of staff employed in the Service. Instead, each authority should appoint a team…. (DHSS and Welsh Office, 1979, p. 7).
And despite Griffiths’ truism that a general manager would need ‘to harness the best of the consensus management approach and avoid the worst …’ (NHS Management Inquiry, 1983, p. 17), the reversal was real. It was the general manager with whom the buck (whatever one of those is!) was intended to stop. Early decisions were taken to place them on limited-term contracts and to open the posts to persons of any occupational background. Subsequently, management development schemes (NHS Training Authority, 1986, p. 2) and career structures (Owens and Glennerster, 1990, p. 103) were built in such a way as to institutionalise a new and virtually exclusive route to the top: through general management rather than through a profession.
In particular, the introduction of general management constituted the first major and systematic threat to clinical freedom, a doctrine which, as has been shown, pervaded the NHS from even before its inception. The abolition of consensus decision-making teams entailed the abolition of a formal medical veto. Clinical performance indicators reflect the way in which hospital consultants manage their beds and their workload and therefore allows this limited aspect of their performance to be visible to others (Shortell et al, 1976). Direct management access to consumer and community opinion (through market surveys, for instance) represents a challenge to the widespread assumption that only doctors may legitimately speak on behalf of patients or be aware of their needs. Systems of management budgets could, if managers chose and if measures of casemix severity were introduced, be used as a vehicle for imposing management priorities on clinicians and for controlling the costs of each type of case (Harrison, 1986, pp. 8-9).
In these ways, the potential for greater managerial control over doctors was created: the potential
to move from a system that is based on the mobilisation of consent to one based on the management of conflict – from one that has conceded the right of groups to veto change to one that gives the managers the right to override objections (Day and Klein, 1983, p. 1813).
Thus the Griffiths and related reforms set out to challenge forty years of professional domination of the NHS (Petchey, 1986, p. 100), though it was not to be expected that members of the government would put it in such blunt terms. In opening the House of Commons debate on the Griffiths Report, the Secretary of State said
Of course doctors and nurses will continue to make their own decisions about how they treat their patients. But equally it would be foolish to deny that there are practical constraints imposed on consultants in a world of necessarily limited resources (House of Commons Debates, 4 May 1984, Col. 649).
The truism that clinical freedom cannot be absolute serves to obscure the fact that it may have degrees.
The medical profession itself certainly saw general management as a threat. The immediate response of the British Medical Association (BMA) to the publication of the Griffiths Report was to complain at the perceived lack of time for consultation, to challenge the concept of a non-medical general manager, to demand the retention of District Management Teams, and to seek the provision of an appeals mechanism against managers’ decisions (British Medical Journal, Vol. 287, 1983, pp. 1321-1322, 1643, 1811). It also sought, in place of the general manager proposed by Griffiths, the election from within existing teams of a Chairman [sic], and a trial period for any changes adopted (Social Services Committee, 1984, pp. 1-13; British Medical Journal, Vol. 288, 1984, p. 84). It was further argued that management at the unit level of organisation was best left to doctors, and that the proposed Supervisory and Management Boards should include clinicians. (The results of these protestations will be examined in Chapter 3.)
The second sense in which general management was radical was that it definitively broke the old assumption (which had been under some strain since 1979: Webb and Wistow, 1985, pp. 210-15; Klein, 1985, p. 197) that better inputs to management produced better management. The introduction of short-term managerial contracts, together with the paraphernalia of review and incentives constituted a new focus on results, rather than inputs.
General management, then, was radical in that it represented a major break with past practice. But it was not a novel idea in relation to the NHS. It had been practised to some extent between 1948 and 1974 in the office of the local authority MOH, though without the use of the title of general manager or chief executive. But the creation of the NHS had already eroded it, and further erosion took place as a result of the Mayston Report (the local government equivalent of the Salmon Report) even before the role was abolished in 1974.
The hospitals had never had a chief executive officer or general manager since the creation of the NHS, despite the existence of the Group Secretary (see above) and the persistence for some years in some places of the role of hospital Medical Superintendent. But, as has been noted above, the proposal was made seriously on two occasions: once from official sources and once from the Administrators’ pressure group (the then IHA) in conjunction with an academic foundation. The official source, the Farquharson-Lang Report suffered the suppression in England of its references to the desirability of a chief executive officer. That such ideas were out of kilter with the times was recognised by two of the architects of the 1974 Reorganisation:
It is not possible to have a ‘managing director’ … clinical doctors could not be made subordinate … (Naylor, 1971, p. 33).
No such solution is realistically available (Jaques, 1978, p. 141).
The authors of the IHA Report recognised this too, but were more optimistic that the climate of opinion might change:
We also understand that it will take some time for the medical profession to consider our suggestion … Nevertheless we think that the logic of our argument … will prevail in the end (Joint Working Party, 1967a, p. 42).
3 General management: Its arrival as policy
This chapter presents, as far as possible without interpretation, data related to the formal adoption of general management as government policy in June 1984. As noted in Chapter 1, the policy’s immediate origins were in the Government’s decision in October 1982 to establish what subsequently became the Griffiths Inquiry into NHS management. This earlier decision needs to be examined in its wider context, and for this reason the organisation of the first several sections of this chapter are thematic: demand for health care resources, the economic (i.e. supply) context, and the political context. Obviously these are not wholly discrete.
From October 1982 onwards, the account is more closely concerned with specific events close to the NHS, and is therefore presented chronologically.
Context: demand for health care resources
The two main contextual variables which are held to imply increasing demand for health care resources in the U.K. are demographic change, and developments in health care (in practice, medical) technology. The term ‘imply’ is used advisedly; in order to form part of any plausible explanation for government policy, such variables would have to be shown to have been recognised by policymakers. In the case of each variable, relevant trend data are presented, followed by evidence of their political recognition at the appropriate time.
Although the U.K. population has now grown continuously for almost two centuries, growth has been relatively slow in recent years as a result of what appears to be a long term decline in the birth rate. Coupled with increased life expectancy, this has produced a population in which increasing proportions are in the older age groups (Central Statistical Office, 1983; DHSS, 1987).
The point was readily conceded by NHS policy makers (see also Fowler, 1991, pp. 165-6):
- the rising numbers of the very old in our community daily present us with new problems on a scale that we have only begun dimly to comprehend (Mr Patrick Jenkin; DHSS 1979b).
- the demand for health care is in effect unlimited, and that is very much accentuated by demographic factors … (Sir Patrick Nairne, Permanent Secretary, DHSS; Committee of Public Accounts, 1981, p. 10).
- these population changes led to extra need for hospital and community health services if the NHS had failed to deliver extra services of at least that amount standards would have dropped (DHSS, 1983k, p. 11).
- you know better than I do about the increasing pressures arising from demographic factors (Sir Kenneth Stowe, Permanent Secretary, DHSS; Stowe, 1986, p. 741).
In fact the 1980 public expenditure white paper, the first produced by the new Conservative government contained a table of estimated current NHS expenditure per capita by age group , and a statement implying that a calculation of the cost of demographic change had been made (HM Treasury, 1980, p. 105) though without stating an explicit figure. Nevertheless, a table of the increasing numbers of the elderly through to 1984 was included. It is clear from this that in 1980 the government knew that it faced a rapidly increasing resource demand from this source.
Table 3.3
|
Persons Aged 75 years and Over UK (Millions)
|
||
| Year | Total UK Population | Persons Aged 75 years and Over |
| 1981 | 56.4 | 3.3 |
| 1991 | 57.5 | 4.0 |
| 2001 | 59.4 | 4.4 |
| 2011 | 59.4 | 4.4 |
Source: Social Trends no 18 (1988) Table 1.2
This situation has changed little since the early 1980s. Table 3.3 shows that it will be the turn of the century before demand abates. Little change has occurred in relative per capita expenditure between age groups (H.M. Treasury, 1991), though the disaggregation of the 85 year and above age group means that the apparent 21st century plateau of Table 3.3 continues to imply increasing demand. Table 3.4 shows the official cost estimates throughout the 1980s and into the 1990s.
Table 3.4
| Demographic Change: Required Increase in Total NHS Funding over Previous Year | |
| Year | Percentage |
| 1980/1 | 1.1 |
| 1981/2 | 0.4 |
| 1982/3 | 0.4 |
| 1983/4 | 0.5 |
| 1984/5 | 0.6 |
| 1985/6 | 1.3 |
| 1986/7 | 0.9 |
| 1987/8 | 1.4 |
| 1988/9 | 1.0 |
| 1990/1 (est) | 0.8 |
| 1991/2 (est) | 0.6 |
Source: Public Expenditure White Papers for relevant years
The second source of implied demand for additional health care resources is technological development. This includes not just equipment and drugs, but techniques of diagnosis, therapy and care more generally (Stocking, 1985, p. 5). The pressures for the utilisation of whatever new technologies are developed is very much an international phenomenon (Aaron and Schwartz, 1984) and not easy for governments to control:
innovations may have diffused readily because there was no need to define explicitly the uses to which staff and equipment were being put. For example, neural tube defect screening [that is, for spina bifida] with its various components of blood tests, amniocentesis, counselling, and abortion is costly. However, it seems to have been able to diffuse relatively rapidly because in its initial stages in any particular locality, no new equipment or funds needed to be requested. It is only as the service builds up that it becomes necessary to ask for additional laboratory equipment, etc (Stocking, 1985, pp. 67-68).
Indeed, the working party responsible for producing the booklet Expensive Medical Techniques was able to go so far as to develop a typology of strategies by which such technological ‘cuckoos’ turned up in the health authority ‘nest’ (Council for Science and Society, 1982, pp. 18-21). Moreover, the expectations of the public can generate quite high expectations of technological availability (Stocking, 1985, p. 48).
Such technology tends to be both expensive in itself and rarely labour-saving, so that its diffusion places considerable pressure on government. It includes new developments in care (including social care) just as much as it includes high technology (Klein, 1989, p. 182). At the same time, however, UK governments have often seemed to wish to take a degree of political credit for keeping up with new developments (see, for instance, DHSS, 1979c; 1983k) and have therefore had to acknowledge them as a legitimate source of demand:
[if unit costs rise] it is in fact a product of advancing medical technology and advancing systems of care which enables that to happen (Mr Patrick Jenkin; Social Services Committee, 1980, p. 105).
The cost implications of both the ageing population and of technological developments were comprehensively recognised in the DHSS publication Health Care and its Costs in 1983 (DHSS, 1983k), since when the government has continued to accept both as pressures which must be accommodated within spending plans. (Demography costs are shown in Table 3.4; technology costs are assumed to be a convenient one-half percent of revenue in real terms per annum.)
Context: macroeconomic policy and the supply of NHS finance
The Conservatives entered office in May 1979 with a commitment to honour the awards made by the (Clegg) Standing Commission on Pay Comparability, two of whose reports related to NHS staff. These reports were not completed until after the election (Standing Commission on Pay Comparability, 1979; 1980). Even after a contribution by health authorities (which an incoming Labour government would also have required) the cost was some £360 million in cash (Social Services Committee, 1980, p. 20).
Yet the Conservatives had also come to office with a commitment to control inflation as the prime item in their manifesto, as well as with a commitment to achieve such control by control of the money supply. In addition, and linked in an obscure and uncertain way to the control of inflation (Allsopp and Mayes, 1985, pp. 424, 433-5), public expenditure was to be controlled:
To master inflation, proper monetary discipline is essential, with publicly stated targets for the rate of growth of the money supply. At the same time, a gradual reduction in the size of the Government’s borrowing requirement is also vital. ( …).
The State takes too much of the nation’s income; its share must be steadily reduced. When it spends and borrows too much, taxes, interest rates, prices and unemployment rise so that in the long run there is less wealth with which to improve our standard of living and our social services (Conservative Party, 1979, p. 8).
This mixture of monetarist and supply-side economics was to take precedence over welfare state expenditure: as the first Secretary of State for Social Services under the new government put it
a sound and thriving economy must be the foundation of all welfare provisions (Mr Patrick Jenkin; DHSS, 1979b).
no-one stands to gain more from a strengthening of the economy and the resumption of growth than the people whom my programmes are intended to serve; because it is only in that way that we will get the increasing resources which are necessary to pay for the services which we provide (Mr Patrick Jenkin; Social Services Committee, 1980, p. 85).
The operational policy for this macroeconomic stance, the Medium Term Financial Strategy (MTFS), launched on 26 March 1980 (Smith, 1987, p. 91). As envisaged in the Manifesto (see above), the MTFS had two elements, the first of which, control of the money supply (Sterling M3) is outside the scope of this study. The second element was a fiscal strategy of restricting the public sector borrowing requirement (PSBR) to a reducing proportion of gross domestic product (GDP) (Jackson, 1985, pp. 51-5).
Table 3.5 (not reproduced) summarises the government’s intentions and the eventual outcomes.
It is evident from the Table that the Government experienced difficulty in making forecasts (hence the difference between columns 2 and 3); this was largely due to inaccurate forecasting of unemployment, and hence of benefits payments (Jackson 1985, p. 53). Hence the progress planned in the 1980 budget was not made (cf columns 2 and 6). The greatest difficulty was experienced, as it transpired, over the period 1980 to 1981, when (see column 5) the absolute GDP was falling. In spite of all this, fiscal policy was extremely tight and the objective of reducing PSBR as a percentage of GDP was eventually met (column 6), even though the original targets were not. Given that the 1981-82 improved figures (columns 5 and 6) would not have been evident before quite late in 1982, the situation in late 1981 and early 1982 would have looked unpromising to policymakers (Thain, 1985, p. 275; Holmes, 1985, p. 108). (The fiscal strategy of the MTFS was subsequently weakened to aim for a constant ratio of Public Expenditure to GDP and, after 1990 further weakened to the achievement of stability over the medium term. By the late 1980s the PSBR no longer existed and public expenditure was at its lowest as a proportion of GDP [Thain and Wright 1992, pp. 198-9]; by 1990 the PSBR had reappeared and by 1992 was regarded once again as a serious problem.)
Table 3.6
| Shares of UK Government Expenditure 1979/1992 – % of General Government Expenditure | |||||
| 1979/80 | 1984/5 | 1989/90 | 1990/1 | 1991/2(est) | |
| Social Security | 25.9 | 30.2 | 29.7 | 30.1 | 31.7 |
| Health | 12.1 | 12.7 | 13.8 | 14.2 | 14.4 |
| Education and Science | 14.5 | 13.3 | 14.6 | 14.5 | 14.2 |
| Defence | 11.9 | 13.0 | 11.7 | 11.2 | 10.5 |
| Law & Order | 4.1 | 4.7 | 5.6 | 5.8 | 5.9 |
| Housing | 7.3 | 3.5 | 2.9 | 2.5 | 2.7 |
Source: derived from The Guardian 12 March 1992
In principle, of course, none of this need necessarily affect the allocation of financial resources to the NHS; expenditure could be curtailed elsewhere in the public sector. Indeed, this has to some extent occurred, as Table 3.6 makes clear. However, the predominance of social security expenditure (most of which is not cash limited) in accounting for one-quarter to one-third of all public expenditure, and the presence of health as the next largest programme (Guardian, 12 March 1992) made it difficult for health ministers to hold out indefinitely against the Treasury:
the Government is determined to stand by its economic policy. This means that health authorities’ cash limits will not be increased this year for the effect of excess price inflation (Mr Patrick Jenkin, 1979, emphasis original).
every nation must adjust to the economic realities of the time the National Health Service is not immune from these realities …. That is why the NHS had to make its contribution to the exercise which the Government undertook [the ‘Lawson’ cuts] to bring public expenditure as a whole back to the course which we had planned for it (Mr Norman Fowler, 1983).
Indeed by the end of the 1981/82 financial year, the health programme was the only one of the largest four government programmes that had suffered only minor cuts in planned expenditure (see Thain and Wright, 1991, p. 19).
The political context
This section considers, in separate subsections, public opinion, parliamentary activity, pressure group activity, and executive (government) activity in the years up to 1982.
Public opinion
In considering the impact of public opinion upon government behaviour towards the NHS, it is convenient to separate opinions about the NHS in general from those about specific places: doctors, bureaucrats, and trade unionists. The evidence cited in this section is derived entirely from opinion polls (and is therefore subject to all the criticisms of polling as a technique: see Taylor-Gooby, 1985a, p. 74 ff), but does not attempt to give a complete review of relevant findings. Moreover, it has not been possible to show that ministers were aware of these specific findings, though they were certainly aware of the general trends indicated. (The Conservative Party conducts private polls, but the results of these remain confidential for some fifteen years after collection of the data.) For these reasons, this evidence is strongly suggestive rather than wholly conclusive. However, there is no shortage of evidence that Secretaries of State for Health in general (Guardian, 20 February 1989, p. 19; 5 July 1989, p. 24) or Mr Norman Fowler in particular (Fowler, 1991, p. 145) habitually concern themselves with opinion poll findings. (The latter point was confirmed by several respondents to the present study.)
Very general poll questions about the popularity or importance of the NHS tend to produce evidence of massive public support; for instance, Taylor-Gooby (1985b, p. 76) cites a 1984 poll in which 93 percent of respondents considered the continuation of the Service to be ‘very important’. Such general evidence can be objected to, on the grounds both that it takes no account of public opinion about taxation, and that it merely taps attitudes concerning the broad notion of a health service, rather than respondents’ concrete experiences with the NHS.
Nevertheless, poll questions concerning NHS finances have also produced responses strongly in favour of additional financial resources for the Service. The British Election Surveys for 1974 and 1979 show, respectively, 84 percent and 87 percent of respondents saying it to be ‘very important’ or ‘fairly important’ that more money be provided to the NHS (Sarlvik and Crewe, 1983). Similarly, MORI polls throughout the two decades up to show increasing proportions of respondents (70 percent by 1980) considering ‘too little’ to be spent on the NHS (New Society, 4 December 1980, pp. 464-465), a finding confirmed in Gallup Polls (Webb and Wybrow, 1981, p. 50).The trend continued after 1980 (Economist, 8 October 1983, pp. 18-21), and more recent Marplan polls confirm the implication (unsurprising in respect of health services free at the point of delivery) that extra funds should be derived from additional taxation or from adjustments in government priorities rather than from increased charges (Davies, 1987, p. 382; Elmore, 1989, p. 122). Finally, Taylor-Gooby’s survey of the Medway area seems to confirm the universalistic principle of the NHS, with 66 percent of respondents saying that services should not be restricted on grounds of income (Taylor-Gooby, 1985b, pp. 30-31).
Predictably, poll questions which focus on the public’s actual experiences of the NHS do show some dissatisfactions and specific complaints. Nevertheless, a survey conducted on behalf of the Royal Commission on the National Health Service showed that over 80 percent of inpatients thought the service ‘good’ or ‘very good’ (Royal Commission, 1979, p. 13), findings subsequently confirmed in a series of polls conducted on behalf of the National Association of Health Authorities (Halpern, 1985a; 1986; Davies 1987a). Reviewing the decade’s opinion polls subsequently, Solomon concluded that ‘Feelings of dissatisfaction with the running of the NHS itself as a political institution are far more widespread than discontent with specific services’ (Solomon, 1992, p. 76).
In comparison with other occupations, health professionals (doctors and nurses) are held in high public esteem; Table 3.7 summarises the findings of three relevant MORI polls. In the earliest (1980), doctors are easily the most highly rated (in terms of ethics) of a list of occupations, whilst in the second (1987) they are only narrowly beaten as a result of the addition of the clergy to the list of occupations. In the third (1987), it is the addition of nurses which once more leaves the medical profession narrowly in second place. Since these polls do not ask identical questions or provide identical lists of occupations (no such comparable data are available), they cannot be interpreted as a trend, but they do serve to illustrate the high level of public popularity enjoyed by doctors and nurses. Despite this high level of relative popularity, however, there are some suggestions that public confidence in the medical profession has weakened slightly since the 1960s as a result of greater public exposures to the reports of ‘scandals’ (Pollitt, 1984), or simply as part of more critical public attitudes towards authority (Harrison, Haywood and Fussell, 1984).
Table 3.7 Public Opinion and Health Professionals
| February 1980: How would you rate the honesty and ethical standards of the people in these different jobs? Would you say they were high, average or low? (%) | ||||
| High | Average | Low | Don’t Know | |
| Doctors | 73 | 21 | 3 | 3 |
| Members of Parliament | 17 | 49 | 25 | 10 |
| Police Officers | 51 | 38 | 7 | 4 |
| Trade Union leaders | 10 | 33 | 46 | 11 |
| Business Executives | 17 | 49 | 19 | 15 |
| Local Councillors | 16 | 50 | 54 | 10 |
| Solicitors | 49 | 33 | 7 | 11 |
Source: MORI, Commissioned by Sunday Times
| December 1983: For each (of the following types of people) would you tell me whether you generally trust them to tell the truth or not? (%) | |||
| Tell Truth | Do Not | Don’t Know | |
| Business Leaders | 25 | 65 | 10 |
| Clergymen/priests | 85 | 11 | 4 |
| Civil Servants | 25 | 63 | 12 |
| Doctors | 82 | 14 | 4 |
| Government Ministers | 16 | 74 | 10 |
| Journalists | 19 | 73 | 8 |
| Judges | 77 | 18 | 5 |
| Ordinary man/woman on the street | 57 | 27 | 16 |
| Politicians generally | 18 | 75 | 7 |
| Police | 61 | 32 | 8 |
| Teachers | 79 | 14 | 7 |
| Television newsreaders | 63 | 25 | 11 |
| Trade Union Officials | 18 | 71 | 11 |
Source: MORI, Commissioned by Sunday Times
| May 1987: Which two or three groups of people on this list do you yourself have most respect for (%) | |
| Civil Servants | 3 |
| Company Directors | 3 |
| Doctors | 70 |
| Journalists | 1 |
| Members of Parliament | 4 |
| Nurses | 75 |
| Policemen | 50 |
| Scientists | 12 |
| Social Workers | 14 |
| Teachers | 20 |
| Trade Union Leaders | 3 |
| None of these | 1 |
| Don’t know | 2 |
Source: MORI
Public attitudes towards the NHS and to health professionals are, however, unlikely to extend to health service managers and administrators, at least if attitudes to public sector bureaucrats in general are any guide. Thus a MORI poll amongst Southwark residents revealed that 69 percent of respondents felt that the local authority ‘wasted’ a lot of money, 42 percent that it spent money on the ‘wrong things’, whilst seven percent objected more generally to ‘bureaucracy’ (New Society, 4 December 1980, p. 465). According to the same source, Conservative Party private polls in 1979 revealed similar attitudes nationally.
The same attitude can, of course, be discerned amongst politicians. The constant concern of the House of Commons Select Committees with administrative manpower in the NHS (see below, and, for instance, Committee of Public Accounts 1981, pp. 6-7) is one manifestation of this, whilst others may be found in ministerial speeches:
if we can slim the management structure of the service, we can switch tens of millions of pounds out of administration and directly into the care and cure of patients (Mr Patrick Jenkin: DHSS 1979b).
Mr Fowler, too, was noted for his slighting references to the NHS’s ‘administrative tail’ (Halpern, 1987), a view which is all of a piece with what Fry (1984, p. 325) somewhat euphemistically terms Mrs Thatcher’s ‘irreverent’ attitude towards public servants. Such anti-statism is, however, not a wholly distinctive Conservative view, for politicians of the left (such as Barbara Castle, Richard Crossman and Tony Benn) have also often felt their efforts to have been thwarted by the bureaucracy (Hennessy, 1987).
If bureaucrats are unpopular, so were trade unions, at least over the period with which this study is concerned. The public distrust of union officials is evident in Table 3.7, whilst other polls show dislike both of unions as organisations and of their activities. Thus, between 1979 and 1980 the proportion of respondents who felt that unions were ‘a bad thing’ rose from 29 percent to 43 percent (Webb and Wybrow, 1981, p. 65), whilst contemporary Gallup polls showed increasing public hostility towards what was perceived as trade union ‘political’ activity (pp. 67-71). In a 1980 poll, 78 percent of respondents considered that British trade unions had ‘too much power’ and showed ‘too little responsibility’ (Times, 21 January 1980). Such data, of course, refer to trade unions in general, but there seems no reason to conclude that they do not apply equally to those unions organising within the NHS.
Parliamentary activity
In the early 1980s, the House of Commons began to display an unprecedented level of interest in the management of the NHS, and, in particular, the size of its workforce. Some of this interest was from individual Members, especially backbenchers on the right of the party. Young and Sloman (1982, p. 32) quote the following example, describing it as atypical only in being ‘calm, civilised and well-briefed’:
I divide this into two parts: first of all, the total number of civil servants, the ones who work in our ministries up and down the country, and then there are the other civil servants, who are workers in the National Health Service and under our education authorities. And it is the latter, let us say the workers in the field, who have expanded so enormously during the last twenty years. Let me give you one example of the scale of movement: between 1960 and 1978 a million people moved out of the private sector and one and a half million people moved into public-sector employment. Now that is a vast change by any standards; it makes a demographic revolution in some senses (Mr Peter Hordern, Conservative MP for Horsham and Crawley, speaking in 1981).
Another example, said to have the ear of Mrs Thatcher, is Mr Ralph Howell, Conservative MP for North Norfolk; on his own account he asked
hundreds of parliamentary questions …. aimed at proving there is no proper management in the NHS (personal communication 1987; see also Howell, 1982).
Indeed, Mr Howells asked nine such questions between May and July 1982 (Hansard, Written Answers, 6 May 1982, Col. 118; 19 May 1982, Cols. 126-7; 10 June 1982, Col. 154; 21 June 1982, Col. 12; 22 June 1982, Cols. 67-8; 22 July 1982; Col. 285; 29 July 1982; Col. 674; 30 July; Cols. 850- 1).
However, it was House of Commons Select Committees which were most prominent in castigating the management of the NHS: the Social Services Committee and the Public Accounts Committee.
In its Third Report for the Session 1979-1980 the Committee made its first examination of DHSS expenditure plans. As part of a general critique of what it saw as a failure by the Department to maintain strategic control of the NHS (Nairne, 1983, pp. 250-252), the Report endorsed the need and scope for greater efficiency in the NHS, but went on to comment on the Secretary of State’s claims that the expenditure cuts of the preceding year had been partly offset by increasing efficiency:
We must, however, express forcibly our disquiet that the Department, whilst embracing the rhetoric of greater efficiency, does not appear to be in a position to measure its actual achievement ….we accordingly recommend that the DHSS should give high priority to developing a comprehensive information system which would permit this Committee and the public to assess the effects of changes in expenditure levels or patterns on the quality and scope of services provided (Social Services Committee, 1980, p. x).
Though the Committee made no cross reference, and did not use the term, it was, in fact reviewing a proposal which its predecessor, the pre-1979 Expenditure Committee, for the development of ‘indicators of performance’ of local health authorities (Klein, 1982, p. 399).
The Government’s immediate reply to the Committee forcibly rejected the general critique, and indeed seemed to miss the point that was being made:
Perhaps the most disturbing aspect of this Report is its assumption that everything should be managed at Whitehall level and that Ministers should preside over every detailed decision. I reject that view. It is the Government’s firm policy that detailed planning and management of resources are best left to those on the spot who know local needs and priorities (Mr Patrick Jenkin; DHSS, 1980c).
(The formal Government reply simply repeated the point at greater length [DHSS, 1980d].) The Social Services Committee returned to the attack in the following year; drawing attention to the dangers of assuming that falling costs per acute case implied increasing efficiency, and went on:
if the health authorities do not succeed in squeezing out waste, then they may economise by cutting either the scale or quality of the services we recommend that as a matter of urgency, every effort should be made to find a way to measure the savings flowing from improved efficiency (Social Services Committee, 1981, p. xiii).
Again, in 1982, the Committee remarked that ‘there is some suspicion that “efficiency savings” are becoming a regular euphemism for “expenditure cuts'” (Social Services Committee, 1982, p. xiii), and still in 1986 it remained sceptical:
Whilst endorsing the Government’s determination to improve efficiency and management in the NHS, we recommend that the Government monitor closely the effect on health services of cost-improvement programmes, to ensure that such programmes do not lead to a reduction in overall health care (Social Services Committee, 1986, p. xix).
The Social Services Committee had not been alone in showing interest in the management of the National Health Service. In his annual report on the appropriation accounts for 1979-80 the Comptroller and Auditor-General noted wide discrepancies in staffing levels and other variables as between health authorities, commenting that his observations raised
…. the question of the right balance, in the interests of economy and efficiency, between the necessary central direction and oversight of the NHS and a system of delegation and discretion appropriate to a locally-based and managed service (quoted in Committee of Public Account, 1981, p. 1).
The Committee of Public Accounts (PAC) took up this matter in a series of hearings in the spring of 1981. Throughout these, members of the Committee stressed the NHS’s accountability to Parliament and emphasised their perceptions of a lack of DHSS control over health authorities. As one member (Mr Michael Morris) put it to the DHSS Permanent Secretary, Sir Patrick Nairne:
…. you have made it clear to the Committee that Ministers settle the national policies, but it does seem to me …. that the Department has got a very relaxed approach to monitoring and implementation of these policies …. [Y]ou are relying, it seems to me, almost entirely on cash limits as the control from the centre. I am still not clear why it is that the Department is against issuing firm instructions (Committee of Public Accounts, 1981, p. 56).
In response, the DHSS witnesses maintained that detailed central control was not necessary, though they referred on several occasions (Committee of Public Accounts, 1981, pp. 5, 53-54, 58) to the Korner working group (see above, Chapter 2), implying that this would in due course provide comparative performance data. (The Korner Group’s terms of reference make no reference whatever to the development of information for central monitoring purposes: Steering Group on Health Services Information, 1982, P- 1).
However, the Committee were apparently finally persuaded of the undesirability of detailed DHSS control, and contented themselves, with a call for greater upward flow of information as a means of monitoring the comparative performance of different health authorities. Their Report concluded that the mere existence of cash limits was not, as DHSS witnesses had argued, sufficient discipline upon health authorities:
arrangements will be satisfactory in practice only if accountability upwards is matched by a flow of information about the activities of the districts, which will enable the regions, and in turn DHSS, to monitor performance effectively and to take necessary action to remedy any serious deficiencies, or inefficiency, which may develop (Committee of Public Accounts, 1981, p. xvii).
By the time the PAC came to review matters again, in the Spring of 1982, the Review Process, Performance Indicator, surplus land, and private audit initiatives had already been announced (see above, Chapter 2), marking something of a departure from past government reluctance to be drawn into such complexities (Graham, 1984, p. 182). In his announcement of them, the Secretary of State acknowledged that the first two were a response to the Committee’s criticisms (DHSS, 1982a, p.3). Welcoming the developments, the PAC concluded that much remained to be done and that it would continue to observe progress (Committee of Public Accounts, 1982, pp. vii-viii). Both the PAC and the National Audit Office (NAO) continued to monitor the NHS closely; in its sixteenth Report for the session 1983-84 the PAC welcomed the management changes of 1982 (see Chapter 2, above) but continued to criticise NHS manpower levels (Committee of Public Accounts, 1984, p. xi).
In 1986, the NAO produced a report questioning whether cost-improvements in the NHS had really been achieved without damage to patient services (NAO, 1986, p. 9), a matter which was subsequently taken up by the PAC in its forty-second Report for 1985-86 (Committee of Public Accounts, 1986). A good deal of adverse publicity, including the naming by an MP of the District Health Authorities where such cuts had occurred, resulted (Davies, 1986b, p. 850). The Committee concluded
We cannot emphasise strongly enough that both the NHS and the Department should keep fully to their policy that [Cost-Improvement Programmes] should not include savings from cuts in services And we note that, despite their increasingly robust scrutiny of CIPs, DHSS could not give an absolute assurance that service cuts had not been included (Committee of Public Accounts, 1986, p. x).
By 1988, the Social Services Committee had begun to make its own calculations, rather than simply relying on Departmental assurances. The following quotation serves as a summary of the stance adopted by the Committee in several of its reports at this time:
DHSS has recently sought to dissuade us from calculating the extent to which growth in expenditure on HCHS [Hospital and Community Health Services] has been sufficient to meet increased demand. The Department does not accept that to achieve its objective of an approximate two per cent increase in services, to meet demographic, technological and service pressures, a concomitant growth in resources of two per cent per annum is needed. According to DHSS, other efficiency gains between 1983-84 and 1986-87 can be quantified. If unit costs had remained at their 1983-84 levels (apart from the effect of inflation), it would have cost nearly £900 million more to maintain 1987-88 service levels than was actually the case. About two-thirds of this figure was attributable to specific cash-releasing cost improvement programmes, so the Department’s figure for the other efficiency gains achieved is of the order of £300 million.
Between 1980-81 and 1987-88 resources for HCHS have grown by 10.3 per cent (taking into account cash-releasing cost improvement programmes) – that is, by about 1.5 per cent per year. To the extent that this is less than two per cent per annum we believe that this represents underfunding although we appreciate that DHSS disputes the Committee’s description of such underfunding as ‘cumulative’. Even after taking account of the extra efficiency gains identified by DHSS, which the Department acknowledges to be “a less precise and certain figure than for cash-releasing cost improvements”, and of cash-releasing cost improvements, in our view the underfunding of the Hospital and Community Health Services between 1980-81 and 1987-88 has been in the region of £1.5 billion at 1987-88 prices (Social Services Committee, 1988, p. viii).
Pressure group activity
A number of groups saw in the election of a Conservative government in 1979 the opportunity to press their various interests in relation to the NHS. Thus, the decision in 1982 to experiment with private audit of the NHS (see Chapter 2 above) was a response to pressure from the Institute of Chartered Accountants (DHSS, 1982b). Similarly, the then Minister of Health, Dr Gerard Vaughan, was lobbied by the Association of British Launderers and Cleaners and the British Textile Rental Association in the autumn of 1979 (Ascher, 1987, p. 26). When it subsequently became evident that NHS managers remained hostile to the Associations’ proposals for NHS laundry and linen services to be subcontracted, further lobbying took place in 1981 through the health service press, and involved a wider range of trade associations who stood to benefit from such subcontracting (p. 27). Such industry representatives continued to argue that they are being unfairly treated even in the system of compulsory competitive tendering subsequently introduced (Public Service Review, No. 4, 1985, pp. 2, 4).
However, this subsection concentrates on pressure group activity from three sources. Firstly, the Confederation of British Industry (CBI) (the major national employers’ organisation) had been criticising government policy on public expenditure. It believed that restrictions beyond those contemplated at the beginning of the Conservative period of office were required in order to provide resources for greater business tax cuts and increased infrastructural capital spending. A systematic statement of this view was set out in a document of 1981 (CBI Working Party, 1981) in which it was argued, inter alia, that NHS staff numbers were excessive and geographically inconsistent (p. 2). It recommended freezing a large proportion of non-direct care posts as they became vacant, the extension of competitive tendering, and the extension of Rayner Scrutinies (pp. 26 ff). The CBI’s working party (which included Mr L.S. Payne, Distribution Director of Messrs. Sainsbury and a close colleague of Mr Roy Griffiths) remained in existence for a further four years, monitoring public expenditure trends (see, for instance, CBI Working Party 1985) during what was in general a period of difficult relationships between the Confederation and the Government (Holmes, 1985, pp. 154-61). CBI opinions on the subject of the NHS workforce were well known to Ministers.
By contrast, a second group, the BMA, was actively concerned to secure additional resources for the NHS. Its 1980 Annual Representative Meeting passed the motion
that this meeting expresses its grave concern at the financial problems facing the NHS and urges the Secretary of State to establish additional sources of capital and revenue with which to maintain and develop the standard of patient care (British Medical Journal, Vol. 281, p. 323).
Council of the BMA also agreed to report on alternative methods of financing, but this seems not to have been done, despite a ‘reminder’ motion at the 1981 Annual Representation Meeting (British Medical Journal, Vol. 283, p. 157). In 1982, the BMA seemed content with a ‘serious warning’ issued to government by Chairman of Council to ‘consider carefully the claim of the NHS for a fairer share of the nation’s wealth’ (British Medical Journal, Vol. 285, p. 240).
A third group was also placing pressure on the government, albeit in a rather different way. 1982 saw the most co-ordinated attempt by the NHS trades unions, representing both ancillary and non-medical professional staff, to secure substantial increases in pay. Industrial action persisted from April until December, when ancillary staff finally accepted an offer made six months before; nurses and a number of other professions had received a larger increase, and subsequently a review body (analogous to that already existing for doctors) to make recommendations on future pay (Barnard and Harrison 1986; Fowler 1991, pp. 168-77; Seifert 1992, pp. 271-9). According to the then Secretary of State, the dispute increased NHS waiting lists by some 65,000 people (Fowler, 1991, p. 171).
The Executive
Prior to the election of the Conservatives to government in 1979, Mr Patrick Jenkin had been Shadow Secretary of State for Social Services. He was aware of the high level of discontent with the results of the 1974 reorganisation of the NHS (see Chapter 2), and had established a small group of NHS administrators (by no means all of whom were Conservative voters) to give informal advice on future policy. The consensus amongst this group was that there was currently a surplus tier of administration and that Jenkin’s proposal for full-time health authority chairman (sic) was unworkable. Despite the once-held view of the then Institute of Health Service Administrators that a chief executive was desirable (see Chapter 2), the group did not propose the abolition of consensus teams. Following the Conservative general election victory on 3 May Jenkin became Secretary of State for Social Services, with Dr Gerard Vaughan (a former NHS consultant psychiatrist) as Minister of State for Health. (Sir Patrick Nairne was Permanent Secretary at DHSS.)
Not long after the election, Jenkin addressed a meeting of the October Club, an association of former NHS administrative trainees saying that he ‘could not imagine’ the government agreeing to any such thing as a chief executive role in the NHS.
As noted in Chapter 2 above, the Royal Commission on the NHS reported in July 1979 (Royal Commission, 1979), shortly after the Conservatives had come to power. Once its more radical options of devolving detailed ministerial accountability for the NHS to RHAs or to local government had been rejected, many of its organisation-related recommendations could easily be reconciled with Ministers’ views that it was necessary to ‘shorten lines of command’ and ‘restore the authority of managers’ as well as contain administrative costs.
Having been persuaded by the civil service that the retention of RHAs was a necessary condition for the survival of the RAWP mechanism, the main thrust of Jenkin’s policy document Patients First (DHSS et al 1979) was simplification and decentralisation: the abolition of Area Health Authorities and consequent establishment of Districts (DHAs) as the lowest level of statutory authority, and the creation of a semi-formal management team at Unit level. The further development of functional management was inhibited (Jenkin had even received proposals for the creation of a post of Regional Head Porter), but consensus teams were retained at regional and district levels:
The Government has rejected the proposition that each authority should appoint a chief executive responsible for all the authority’s staff. It believes that such an appointment would not be compatible with the professional independence required by the wide range of staff employed in the Service. Instead, each authority should appoint a team to co-ordinate all the health service activities of the district, including in particular the implementation of decisions taken by the authority, and to advise on the planning and provision of services. The district team should have the same composition as existing area management teams. Membership of such a team should not be allowed to derogate from the responsibility of individual managers on the team to manage the services for which they are responsible, while working together as a strong and cohesive group (DHSS et al, 1979, p. 7).
After a period of formal consultation, which revealed, inter alia, substantial support within the NHS for the retention of consensus teams (DHSS, 1980c, p. 8), a decision was made to further restructure the NHS (the term ‘reorganise’ was avoided) along the lines proposed with effect from 1 April 1982. Although the creation of new statutory Districts, and the necessity to advertise and appoint to large numbers of new and revised posts made the period 1980 to 1982 one of considerable upheaval within the NHS, the organisational changes cannot themselves be regarded as radical.
Indeed, at this time the NHS was somewhat detached from contemporary managerial developments elsewhere in the public services. Thus, although it was subject (as noted in Chapter 2) to the Treasury’s ‘efficiency savings’ provisions from 1981, it remained outside the scope of Rayner ‘scrutinies’ (Hennessy 1989) until April 1982 (though more than one such scrutiny was concerned with the social security side of DHSS: Warner 1984), and of compulsory competitive tendering until 1986. Despite ministerial hopes that the private sector would grow to carry out a quarter of all hospital work by 1985 (Wintour and Wheen, 1982, p. 10), radical change to the NHS’s finances was, however, considered and rejected on two occasions.
The first of these two episodes concerned possible alternative finance mechanisms for the NHS. The Secretary of State announced on 30 July 1981 that:
My Department is in the process of completing its studies of health care financing in other Western countries, which form the groundwork for consideration of what options there may be to improve health care financing and delivery in this country. In view of the advanced state of this work, I am now able to announce the formation of an inter-departmental working party which will consider, on the basis of these findings, a range of possible proposals for improvement. When this second stage of the review is completed, which I expect to be by the beginning of 1982, I and my colleagues will be in a better position to establish which if any of many possible approaches is likely to be of value here, and to select options for more detailed examination (DHSS, 1981).
The working party seems to have been partly a response to what one inside described as ‘difficult relations with No. 10 over [NHS] manpower’ and partly as a result of the urgings of Dr Vaughan (British Medical Journal, Vol. 283, 1981, pp. 244, 447). With the assistance of policy consultants from the private health care sector and of reports from civil servants of field trips to the continent and elsewhere, the working party explored a range of alternatives to tax-based funding, ‘including national insurance, private insurance, and charges for services.’ (See also Klein 1984, p. 91; Godt 1987, p. 472.) In December 1981 the Guardian newspaper claimed that radical proposals were imminent and that
At the moment all four Health Ministers – Mr Norman Fowler…., Dr Gerard Vaughan, Lord Elton and Mr Geoffrey Finsberg -are united in wanting to examine these options (The Guardian, 2 December 1981, p. 1).
This was by no means the case. Mr Jenkin had been much less enthusiastic than Dr Vaughan, and neither senior civil servants at DHSS or the Treasury had been keen on the lack of central financial control in the alternative systems studied. Even the Prime Minister, it was believed, was extremely cautious. Mr Fowler, who had succeeded Mr Jenkin as Secretary of State for Social Services in September 1981, did not take much persuading that the alternatives had insufficient merit; he announced on 30 July 1982 that
The government have no plans to change the present system of financing the NHS largely from taxation, and will continue to review the scope, for more cost consciousness …. and for increasing private provision (DHSS, 1982g).
As Fowler subsequently noted in his autobiography
Every country in Europe was facing an explosion in demand for health care; every country in Europe was spending substantial public resources upon health; and in many ways our centrally run, centrally financed system was the most effective in controlling costs. There was no inherent cost advantage in moving over to an entirely new financing system and it was also clear that whatever system was chosen, taxation would still have to finance a giant share of the service. The unemployed, the poor, the chronically sick and disabled and of course children would need to be covered by public money (Fowler, 1991, p. 184).
By this time Mr Kenneth Clarke had succeeded Dr Vaughan as Minister for Health.
In addition, a number of steps had been taken which represented a centralisation of NHS decisionmaking; as a response to the criticisms of the PAC (see above) concerning alleged lack of Departmental control over the NHS the development of performance indicators and the introduction of the review process has been announced (see above, Chapter 2). The latter had been the idea of the new Permanent Secretary, Sir Kenneth Stowe, who had arrived at the DHSS in August 1981 a few weeks before Mr Fowler; the former had been devised by one of Stowe’s staff.
Having set out along this course of further managerialism rather than changes to the funding arrangements, Fowler was less than enthusiastic about the second episode of proposed radical change, coming, as it did only five weeks after his announcement that there was no intention of changing the funding basis of the NHS (Fowler, 1991, p. 184). During the Public Expenditure Survey of summer 1982, Treasury ministers had asked the Central Policy Review Staff (CPRS) to indicate as quickly as possible some options:
Nothing was to be considered too radical in principle: the objective was to show Ministers the kind of ways by which they might cut public spending by £1 billion by 1990 (Blackstone and Plowden, 1988, p. 95).
There were only a few days available for the work, and the resulting ‘quick and dirty’ paper was circulated to members of the Cabinet on 7 September 1982, in advance of its scheduled discussion on 9 September (Economist, 9 October, 1982, p. 22). The radical options included replacement of the NHS with private insurance, but the CPRS had added the comment that this was not worth pursuing since privatised systems were more expensive (Blackstone and Plowden, 1988, p. 96). According to the Economist there was a considerable majority in Cabinet against the paper as a whole, so that despite the Prime Minister’s wishes it was not discussed in detail (Economist, 9 October, 1982, p. 22). It was only after the CPRS paper had been pieced together from a variety of ‘leaks’ and publicised in the Economist on 17 September that it was felt necessary to comprehensively dissociate the Government from it. (This incident is frequently cited as a major cause of the eventual abolition of the CPRS in 1983: see, for instance, Blackstone and Plowden, 1988, p. 95).
Establishing the Griffiths inquiry
The Conservative Party Conference was to take place in the first week of October 1982. So far as the NHS was concerned, it was felt to be politically imperative to provide public reassurance in the wake of the CPRS leak, and in the probability that a general election would occur before the next such Conference. The Prime Minister provided this reassurance in her closing speech: ‘the NHS is safe with us’, she said (Sherman, 1982, p. 10).
t the previous day’s conference proceedings, Mr Fowler had closed the health debate with an attack on the health unions and the then current industrial action but added the statement that
we want manpower directed at serving the patient, not at building new empires of paper and bureaucracy. Over the last twelve months I have set in hand …. a series of measures to ensure that we make better use of manpower. I want to make even faster progress, and with this in mind I intend to establish a small team, headed by people from private industry, to achieve it. Their job will not be to produce a lengthy report – there is no shortage of lengthy reports in the Health Service – but to help us produce results, not in years but in months (Fowler, 1982, p. 12).
The decision to employ an informal inquiry rather than a Royal Commission or other formal arrangement was wholly in keeping with the previous (and subsequent) practice of Thatcher governments. The specific proposal had, however, been made by Sir Kenneth Stowe, the DHSS Permanent Secretary, during the preceding August (so that it preceded the CPRS incident). The decision to use businesspersons was simply ‘good form’ at the time. The focus of the new inquiry was to be on ‘manpower’ the aspect of the NHS which, as has been noted above, had been most subject to political criticism: it was a response simultaneously to Mr Howells’, the CBI’s and ‘no. 10’s’ concerns.
The ‘manpower’ inquiry having been announced, and the Secretary of State being much occupied with the NHS industrial action, it was left to the civil servants at DHSS to get on with setting it up; no urgency was displayed, though Mr Fowler did make a reference to the inquiry in his speech in the House of Commons on an Opposition motion deploring the Government’s failure to settle the NHS industrial dispute:
We must therefore make the best use of manpower [sic] and seek the highest possible efficiency in the Health Service itself. During the past few months the Government have set in hand a whole range of initiatives. They include setting up a small team to help us carry through our manpower initiatives, drawing on the experience of people in outside industry (Mr Norman Fowler, Hansard, 20 October 1982, Col. 384).
An early decision was, however, made that the support to the inquiry would be handled by Mr Cliff Graham, an Assistant Secretary at DHSS. One potential Chairman of the inquiry was approached in November or December 1982, but declined the offer on grounds of a potential conflict of interest. The Trades Union Congress were consulted as to possible members of the inquiry team and Mr Len Murray, its General Secretary, proposed Mr Michael Bett, Board Member for Personnel of British Telecom. Bett was visited at home by a civil servant in December 1982, and accepted the invitation, without at that time knowing who was to chair the inquiry.
A second member of the team was Sir Brian Bailey, already involved in the NHS as Chairman of South-Western RHA, a former official of the trade union NALGO with business interests in television. Suggested by Sir Kenneth Stowe, Bailey was in some ways a natural choice, having been an author of the ‘Three Chairmen’s Report’ (see above, Chapter 2), and having just completed a two-year term as Chairman of RHA Chairmen (sic).
The two remaining members of the inquiry team were both linked with close confidants of Mrs Thatcher. Sir Hector Laing, Chairman of Messrs United Biscuits, drew attention to Mr Jim Blyth, his company’s Group Finance Director; the latter accepted membership. Sir John (later Lord) Sainsbury, Chairman of the eponymous supermarket chain, suggested his deputy, Mr Roy Griffiths, who had recently volunteered his services to the Public Appointments Unit. Informal soundings effected by Sir Derek Rayner confirmed that Griffiths was perceived as a major architect of Sainbury’s current commercial success. When offered the chair of the NHS ‘manpower’ inquiry by Stowe in December 1982, Griffiths was initially extremely reluctant.
Griffiths’ objections, which were to the terms of reference proposed, were twofold. Firstly, being aware of the political saliency of the NHS ‘manpower’ issue, he did not wish to be cast in the role of ‘hatchet man’, cutting NHS staff, especially in what was almost certain to be an election year. Secondly, he took the view that the terms of reference were too restricted; logically enough, his perspective was that to inquire into the ‘manpower’ of an overstaffed organisation was to confine inquiry to a second order problem. Rather, the first order problem was ‘a management problem, or general problem’. Hence, only if the proposed terms of reference for the inquiry were modified to include this wider concern would Mr Griffiths accept. Though ‘taken aback’ by the response, Stowe organised a meeting between Griffiths and ministers – Fowler, Clarke and Finsberg – at which broader terms of reference were agreed. The way in which team members had been approached meant that Griffiths had been unable to influence its composition, however.
The establishment of the inquiry was announced on 3 February 1983 in response to a written Parliamentary Question from the Conservative Mrs Jill Knight; despite the change in terms of reference (and despite NHS ‘manpower’ controls by the DHSS having been announced less than two weeks before: see Chapter 2), the ‘manpower’ issue was still given prominence. The Question asked the Secretary of State if he would make a statement ‘on what plans he has to control manpower in the NHS’ (DHSS, 1983i, p. 1).
Although Fowler’s reply began ‘I have today established an independent NHS Management Inquiry into these matters’ (DHSS, 19831, p. 1, emphasis added), it went on to place the inquiry firmly in the context of earlier management changes, before summarising the terms of reference:
Over the last four years this Government has devoted extra resources to the NHS. Next year we will be spending nearly £13 billion on the NHS in England. That represents a real increase in services of 7J/2% and an increase of 17% against the Retail Price Index. But what matters most is the actual services the patients are getting for this money and the way in which the delivery of these services is managed by the NHS.
In 1979 we therefore embarked on the essential task of strengthening the management of the NHS and improving its efficiency and effectiveness in the interests of the patients. First, we slimmed down the structure of administration to cut out unnecessary bureaucracy. Second, we developed a new framework of public accountability and review, to clarify and make more effective the management chain from the District to the Secretary of State. Third, we launched a whole series of initiatives, aimed at improving the management efficiency of the NHS; including NHS manpower targets, the development of NHS performance indicators and the introduction of financial targets for efficiency savings.
What we need to be sure of is that in practice this whole management process is working properly and that it produces, for both patients and public alike, the best possible service from the very large resources allocated to the NHS.
We are therefore now setting the Inquiry Team two main tasks:
- to examine the ways in which resources are used and controlled inside the health service, so as to secure the best value for money and the best possible services for the patient;
- to identify what further management issues need pursuing for these important purposes.
We could simply have set up another Royal Commission and then sat back for several years to await its lengthy report, but on past experience that would not lead to effective action. Instead, we have gone straight for management action, with the minimum of fuss and formality. I am grateful to Mr Griffiths and his colleagues for agreeing to carry out this task (DHSS, 1983i, pp. 2-3).
The inquiry team (Bailey had by this time become Chairman of the Health Education Council) was to be supported by Mr Graham; in addition, Stowe ‘loaned’ his Private Secretary Ms Kay Barton. (Later, Mr Tim Stevens was added to the support team.) The team was to report on progress by June 1983. Uniquely, the final output was not to be a formal report but advice to the Secretary of State on ‘Management action’.
Fowler’s speech had, in fact, misquoted the terms of reference by omitting the word ‘manpower’, which remained in them: as the eventual report put it:
We were asked to give advice on the effective use and management of manpower and related resources in the National Health Service (NHS Management Inquiry, 1983, p. 1).
Not surprisingly, the significance of the Griffiths inquiry was not recognised (indeed it was arguably not recognisable) until later. Under the title ‘Manpower checkout’, the (then) Health and Social Service Journal, the most widely read NHS management journal, could not understand what was happening:
NHS managers are bemused as to why yet another inquiry is being set up to study those areas of manpower which are constantly under scrutiny through the procedures of ministerial and regional reviews while many administrators admit there are areas where manpower levels are inconsistent, they believe this can only really be teased out at a local level, and a central inquiry is both unnecessary and ineffectual (Health and Social Service Journal, 17 February 1983, p. 196).
Yet, save for its alleged exclusion of medical staff, at which administrators were said to be ‘annoyed’, the expanded account of Griffiths’ remit quoted by the Journal was nearer to the reality of the task upon which the inquiry team was about to embark:
- To review present management incentives
- To examine ways in which NHS resources are used and controlled including the internal management of hospitals
- To advise if any further action is needed by the Secretary of State.
The team will question whether better use can be made of manpower resources, if there is any scope in the health service to improve efficiency, and if the patient is getting value for money. The team will examine all non-medical staff covering administrative and clerical, nursing and midwifery, professional and technical and ancillary staff groups (ibid, p. 196).
The British Medical Journal, presumably not at that time as interested in the topic, confined itself to a bare statement of the (correct) terms of reference and membership of the inquiry (British Medical Journal, Vol. 286, 1983, p.659).
Only the NHS administrators’ professional journal (perhaps with the time for reflection enforced by a less frequent publication schedule) was able to put the inquiry into any kind of perspective (though it did not make the connection back to the Conservative Party conference of four months earlier):
It looks as though the inquiry is part of the price the NHS has to pay for Ministers’ success in fending off some rather wild ideas for dismantling it (Hospital and Health Services Review, March, 1983, p. 52).
The process of the inquiry
The first meeting of the inquiry team was over dinner at Sainsbury’s. Early in the discussion, one member of the team described his view of the task before them simply as ‘gauleiter versus consensus’. Asked if a gauleiter model would mean that doctors had to be in charge, another member replied ‘If so then we should all go home now’. On Graham’s suggestion a decision had been taken to use the style ‘NHS Management Inquiry’ and the team was subsequently provided with its own letterhead to this effect.
The team undertook no primary reading of NHS literature in general, nor of relevant research literature (see Chapter 2). However, Graham produced a report distilling some 150 relevant official documents including the Farqharson Lang Report (in connection with which Graham had written the Ministry’s English circular in the mid 1960s: see Chapter 2). One such document by which some team members were said to be impressed (though others could not recall it at all) was the Bradbeer Report of 1954 (Central Health Services Council 1954) which, as was noted in Chapter 2 above, demanded the (then) retention of a single chief officer at the level of the statutory authority but accepted a multidisciplinary triumvirate at hospital level. The team did not perceive themselves to have been given any kind of political ‘steer’ towards a chief executive or any other particular solution; indeed some senior DHSS civil servants regarded it as a matter of some concern that they could not foresee the outcome. The inquiry proceeded along three main lines.
Firstly, the team members were involved in a programme of visits within the NHS. These were often performed by individuals (usually Griffiths, Bett and Blyth) and followed by relatively infrequent meetings at which ideas were pooled and Bailey’s NHS experience used as a sounding board. The approach was later summed up by one of the team’s support staff thus:
Time was short. The team decided they could not invite evidence formally. Instead they would be open to all advice, invitations and written evidence. They did accept many invitations to meet groups and individuals, in the NHS and from other interested bodies. As time went on, they had to be more selective; for example, turning down invitations from local branches of national organisations. Otherwise we should have taken nine years, rather than nine months (sic) (Barton, 1984, p. 41).
The approach adopted on visits was to listen to opinions offered rather than to ask specific questions. Early in the course of the inquiry the rumour had spread within the NHS that full-time DHA chairpersons and chief executives were a likely outcome (see, for instance, Sherman, 1983, p. 426), and many witnesses volunteered their opposition to the notion. A few witnesses, especially RHA and DHA chairpersons, were more supportive. In general, the impression left upon team members by these visits was an absence of management and an excess of professional domination; this was variously described as ‘a polo style of management’ (i.e. with a hole in it like the well-known confection), ‘people banding together [in professions] in search of leadership’, and ‘top-level trade unionism in action rather than selfless devotion’.
Shortly after the Conservatives’ election victory on 11 June 1983, Griffiths had a meeting with Regional Administrators (later described by one of the participants as ‘disastrous’) at which the general manager notion was floated. The proposal met a hostile response, though it was later privately explained that much of the hostility had sprung from a feeling that the idea had long ago been killed off (by Jenkin: see above). One consequence was a degree of public coyness on the topic by team members. In an interview given to the Health and Social Service Journal in July 1983, Griffiths was paraphrased as saying:
The Griffiths inquiry is not about instituting a tier of chief executives throughout the NHS or general managers or full time chairmen. It is about tracking down responsibility. While the NHS management inquiry set up earlier this year could end up recommending any of the numerous solutions already suggested by previous reports, it is at the moment still at the stage of asking questions rather than supplying answers (Halpern, 1983, p. 832).
Yet the team had already made its mind up about general management, albeit subconsciously. Given the business backgrounds of three of them ‘we took this conclusion in with us’. The fourth member of the team ‘came to acquiesce’ on the basis of the visits: ‘we drifted into the general manager assumption’. And as another said ‘I was only rarely influenced by what witnesses thought’. As Ms Barton subsequently put it
The team had been asked to advise from their own expert knowledge, so there was no need to try to justify their conclusions by claiming depths of knowledge (Barton, 1984, pp. 41-2).
The second line of inquiry pursued by the team was to commission the Management Advisory Service (see Chapter 2) to conduct studies of the relationship between doctors and the management process at five NHS general hospitals: Guy’s and St. Thomas’s in London, the John Radcliffe in Oxford, the Freeman in Newcastle upon Tyne, and Farnborough Hospital at Bromley. These ‘unit studies’ were effected between May and July 1983. By its own account, the report of these studies ‘set out generally negative observations on the management process’. In particular:
Clinicians may view management as a service provided to them by someone else There is no obligation placed on the clinician to become engaged in any activity which might, however loosely, be described as management. The clinician’s influence on the management process is, however, profound. He (sic) commits huge resources [and] influences management decisions over priorities for development or reallocation of funds and other resources, by forming a heavily influential lobby. The clinician exhibits all the characteristics of good management when wishing to advance the state of knowledge in his (sic) own clinical field [but] the vitality which clinicians can supply for their own clinical issues is not available to the organisation as a whole.
The inquiry team concluded that the findings reinforced a number of the opinions that they had already formed: that hospitals contained a number of complex organisational processes without anyone in charge of them: that doctors were essentially unmanaged: that no mechanism existed to link clinical workloads to financial resources.
The third line of inquiry pursued by the team related to this last point. Blyth (the team member with a background in finance) was concerned to develop a system of workload-related budgets, which were given the title ‘management budgets’. Although sporadic work on this topic had been in progress in the NHS for some years (Wickings, 1983; Wickings et al, 1983), the decision was made, with encouragement from senior civil servants, to commission management consultants to produce more rapid results in four ‘demonstration’ districts. Messrs Arthur Young McClelland Moores were contracted at DHSS expense to work in North Tees and Southmead DHAs, and Messrs Cooper and Lybrand in Haling and Basingstoke. Work commenced in September 1983 (before the team had reported) with a target implementation date of 1 April 1984. The terms of reference were
To develop management budgets at unit level with the emphasis on management not accountancy. The aim is to produce an unsophisticated system in which workload related budgets covering financial and manpower allocations and full overhead costs are closely related to workable service objectives, against which performance and progress can be compared.
The team also set out the principles upon which management budgets were to be based. Some of these provide a clear insight into the reasoning behind the notion, and how it was linked with the conclusions drawn from other lines of inquiry:
- The unit is the focal point for management delegation and as such will be provided by the district with an allocation in total terms of the annual money expected to be available.
- Budget holders by definition must be given the responsibility for preparing their budgets.
- Since the principle of clinicians as the main users of resources at Unit level is established, they, individually or in groups, will be classed as ‘User Budget Holders’ and as such will have charged to their budgets:- Direct Costs – A charge from other functional cost centres for the use made of those resources.
- Functional budget holders will also be responsible for preparing their budgets on the basis of agreed/ estimated/anticipated usage but it is intended that their total costs be ‘recovered’ from the ‘user’ budget holders.
- The co-ordination of budgets within the Unit will be the responsibility of:-The Unit management team and/or one nominated member of that team as overall unit ‘supremo’.
- -The management accounting arm of the District Treasury function.
The required progress report from the team, a document of only three pages, vhich was never made public, was considered by Cabinet in June 1983. The text of the main report was written, largely by Griffiths and Graham during September. There had been no substantial dissent amongst the team, though some of its members would have liked to see more radical proposals, including the ‘floating off of the NHS from detailed ministerial accountability, a suggestion, it will be recalled, made by both the 1976 ‘Three Chairmen’s’ report (of which Bailey had been a co-author), and the Royal Commission on the NHS and rejected by Jenkin. (The notion of the NHS Management Board, which was proposed by the inquiry team, is in a sense the ‘rump’ of this idea.) Other more radical ideas held by team members included RHA chairpersons operating as a national collective, HAs as employers of consultant medical staff, and tougher disciplinary procedures for doctors.
What remained in the report was very much associated with Griffiths personally (‘Griffiths processed everything’) though there was a view from sne team member that the Permanent Secretary had helped to ‘domesticate’ some of the proposals. The team members fully expected their conclusions to be made public, but did not expect to be in any way responsible for implementing them. (Indeed, apart from a few presentational meetings, only Griffiths and Graham had any subsequent involvement.) Rather, they saw their task as to stake their opinions: as one member put it
They [ministers] could take it or leave it.
Although they recognised that general management was not likely to be immediately well-received by doctors, it had been the possible delegation of consultant contracts to DHA level that had been presented as the main area BMA concern, in respect of which a major dispute had been predicted. )n the topic of general managers, the BMA had been ‘dispassionate’ during lie inquiry (in contrast to afterwards: see below). They had been reassured t>y Ministers that the proposals would not interfere with clinical freedom. The model of the existing relationship between DHSS Permanent Secretary Chief Medical Officer was used to justify this: the former was accounting officer and head of the department, but the latter had direct access to Ministers.
Moreover, during the team’s visits to hospitals ‘Griffiths had the doctors eating out of his hand’ by sympathising with their views about poor management. It was not surprising, therefore, that the inquiry team were not overly apprehensive about the eventual medical reaction. And at least one member had mixed feelings; for him, the prospect of a battle with the doctors served as ‘both a deterrent and an incentive’.
The team’s report which had been the subject of oral briefing, but not written draft, within the Department was sent to the Secretary of State on 6 October 1983. It took the form of a twenty-four page letter signed by Griffiths. It began by emphasising that it was not (presumably in the formal sense) a report but rather a set of recommendations for action (as indeed had been the principle set out in Fowler’s original speech almost a year before). The report was in two parts. The first (occupying seven pages) set out the recommendations for action (see Chapter 2 above).
The second part of the report (some fifteen pages) contained background and some of the reasoning behind the recommendations. Although not very tightly structured, this section contained what can be seen as the four key elements of the inquiry team’s diagnosis of NHS management.
Firstly, the team were concerned that individual overall management accountability could not be located:
it appears to us that consensus management can lead to ‘lowest common denominator decisions’ and to long delays in the management process the absolute need to get agreement overshadows the substance of the decision required In short, if Florence Nightingale were carrying her lamp through the corridors of the NHS today, she would almost certainly be searching for the people in charge (NHS Management Inquiry, 1983, pp. 17, 22).
The character of this analysis as a critique of NHS professionalism is largely veiled by the text itself, though reference is made to the need to ensure that professional functions are ‘geared into the overall objectives of the general management process’ (p. 14).
The second aspect of the team’s diagnosis was that ‘the machinery of implementation is generally weak’ (p. 14).
there is no driving force seeking and accepting direct and personal responsibility for developing management plans, securing their implementation and monitoring actual achievements …. certain major initiatives are difficult to implement [and] above all lack of a general management process means that it is extremely difficult to achieve change [A] more thrusting and committed style of management is implicit in all our recommendations (pp.12, 19).
Thirdly, the inquiry team drew attention to lack of an orientation towards performance in the Service.
it lacks any real continuous evaluation of its performance rarely are precise management objectives set; there is little measurement of health output; clinical evaluation of particular practices is by no means common and economic evaluation of these practices is extremely rare (p. 10).
Finally, the team identified a lack of concern with the views of consumers of health services:
Nor can the NHS display a ready assessment of the effectiveness with which it is meeting the needs and expectations of the people it serves Whether the NHS is meeting the needs of the patient, and the community, and can prove that it is doing so, is open to question (p. 10).
Publication and decisionmaking
In his speech to the Conservative Party Conference on 13 October 1983, Mr Fowler made no reference to the Griffiths Report, though it was already publicly known that he had received it (Health and Social Service Journal, 13 October 1983, p. 1215). Rumours about its content were incorrect, especially the assumption that the fourteen RHA chairpersons would form a national tier of management (ibid, p. 1216). Much of the health debate at the Conference was occupied with attacks on NHS bureaucracy, in which Fowler joined: ‘I should like to see savings directed (sic) at the administrative tail’ (Health and Social Service Journal, 20 October 1983, p. 1243). Yet he did provide some clues about Griffiths: ‘too much administration and too little management’: ‘how can you talk of local devolution of responsibility if locally no-one knows who is in charge?’ (ibid, p. 1244).
In her closing speech, the Prime Minister elaborated on her comment of the preceding year:
At this conference last year I said ‘The NHS is safe with us’. I will go further. The NHS is safe only with us because this government will see that it is prudently managed and financed, that care is concentrated on the patient rather than the bureaucrat. That is the true, the genuine care (Mrs Margaret Thatcher, quoted in Small, 1989, p. 104).
The Griffiths report, in fact, had the support of the Secretary of State and the Permanent Secretary, and had been approved at ‘No. 10’. Two weeks later, as predicted by the Health and Social Service Journal, the report was made public (Health and Social Service Journal, 20 October 1983, p. 1244). This was effected through a statement by Mr Fowler in the House of Commons:
The Inquiry Team endorses the main initiatives that the Government has already taken to make health authorities accountable for the performance of the services they provide. However, they say an enormous programme of management action is still needed. The Inquiry Team found that at all levels in the National Health Service there is a lack of a clearly defined general management function. Responsibility is too rarely placed on one person. Although they would like to harness the best of the consensus management approach, they found that at present consensus management can lead to lowest common denominator decisions, and long delays in the management process. Another effect is that the process of devolution of responsibility is ineffective (Fowler, 1983a, p. 1).
Later in his statement, Fowler accepted the inquiry’s proposals for a Health Services Supervisory Board and for an NHS Management Board. In respect of the other proposals, he announced a period of consultation, after which, it was hoped ‘the general management function’ could be implemented by April 1984.
The text of the report was sent for information to the NHS on the same day (DHSS, 1983i). Appended to this were a set of ‘Accompanying Notes’, inserted at the insistence of senior civil servants, elucidating various parts of the text proper. In general, these notes set out to allay possible concerns of persons working in the DHSS and NHS, and in particular concerns about general management; a number of observers were particularly amused by the obvious addition – in a different typeface – of the final sentence of paragraph 6:
5. The General Manager (recommendations 6.2 and 8.3): The appointment of general managers would not imply the end of the good features of the consensus management approach. Paragraph 15 makes this clear, and should be read with care. In the words of that paragraph, ‘the identification of a general manager [would] harness the best of the consensus management approach [ie the attempt to reach inter-disciplinary agreement on points that cross professional boundaries] and avoid the worst of the problems it can present [ie ‘lowest common denominator decisions’ and ‘long delays in the management process’].
6.Equally, it is clear from paragraph 15 that the proposal (in recommendation 6.6) that the primary relationship of functional managers should be to the general manager would not ‘weaken the professional responsibilities of …. chief officers, especially in relation to decision taking on matters within their own spheres of responsibility.’ For instance, nurses will still lead nursing.
7.Recommendations 6.2 and 8.3 speak of identifying a general manager regardless of discipline. This should be taken for what it means: ie that the general manager could just as well be, say, a treasurer, a nurse, or a doctor (whether clinician or community physician) as an administrator. The only criterion is who is ‘the best person for the job’ (paragraph 21).
A further paragraph of the accompanying notes reflected a particular concern of Mr Kenneth Clarke: though the Griffiths text had spoken only generally of incentives and sanctions, the notes employed a remarkable non sequitur to arrive at the conclusion that general managers should be subject to the fixed term contracts which Clarke had believed to be the norm in private industry:
8. It is implicit in the report that the general manager – like other staff – would be assessed against performance. He or she would need to be appointed for a fixed term and re-appointment should not be regarded as automatic.
Within a few days it was announced that Mr Graham, who had headed the support staff to the inquiry team, had been promoted to Under-Secretary at DHSS and would head the Regional Liaison Division, which would have the prime responsibility for implementing the government’s eventual decisions on the report; he was later described as ‘Mr Griffiths’ main apostle to the NHS’ (Halpern, 1984, p. 429).
On 18 November, the formal period of consultation began; in a letter to chairpersons of health authorities, the Secretary of State sought views by 9 January 1984 on the general management function, and on the involvement of clinicians in the management process (Fowler, 1983b). The elliptical wording was reassuring in tone:
I have it in mind to issue guidance early next year requiring (sic) Authorities to clarify the general management function by identifying a general manager at region, district and unit level, along the lines of paragraphs 14-16 of the Report. We particularly share the Griffiths view that this should not add to existing management structures but should provide a much needed refinement of them. Our guidance would (as at present proposed) require Authorities to designate (on the recommendations of the Chairmen) the general managers who would be drawn in most cases from amongst existing staff, to undertake the general management function for a defined period of 3-5 years (Fowler, 1983b, pp. 1-2).
Those working in the NHS, however, were not reassured at the possible demise of consensus teams, but each profession took the view that if there had to be a general manager he or she should come from that group:
If it were a matter of Hobson’s Choice, the doctor should be top dog.
It must be taken for granted that at unit level, the general manager must be a nurse. (BMA and Health Visitors Association spokespersons, respectively: paraphrased in Hyde and Wilson, 1983, pp. 1309-10).
(For synopses of organisational responses to Griffiths, see Hospital and Health Services Review, March 1984, pp. 94-7; Health and Social Service Journal, 12 January 1984, p. 37.)
In the event, a decision was taken by Mr Fowler to extend the consultation period. The Social Services Committee had been re-constituted following the general election and decided in December 1983 to make the Griffiths Report its first topic of enquiry. Four oral hearings were held between 18 January and 8 February 1984 and a final report published on 15 March 1984 (Social Services Committee, 1984).
The BMA’s view of the general manager proposals had hardened since the inquiry and since its Council meeting on 4 January 1984; the Chairmen of Council, Mr Anthony Grabham, had written to the Secretary of State in the following terms, which were also put in evidence to the Social Services Committee:
Of all the many points raised in the Council debate there was most concern over the concept of the ‘executive’ manager. It could be interpreted from the report that a somewhat autocratic ‘executive’ manager would be appointed with significant delegated powers, who would – in the interests of ‘good management’ – be able to make major decisions against the advice of the profession. The council hopes and believes that this is not intended. But it should be clearly understood that the profession would neither accept nor cooperate with any such arrangement – particularly where the interests of patients are concerned. While such appointments may be necessary and desirable in trade and commerce they can have no place in the health service which depends upon a number of caring professions working together as a team in the interests of patients …. The council strongly endorses the view expressed in the report that the best of consensus management should be maintained, and strongly recommends that this is achieved through the existing structure of the district management team (quoted in British Medical Journal, Vol. 288, 14 January 1984, p. 165).
This virtual declaration of independence was amplified in the oral hearing on 18 January 1984:
(Mrs Short) If [the Griffiths proposals] are implemented, Mr Grabham, how do we interpret your remark that the profession would neither accept nor cooperate with the general manager concept?
(Mr Grabham.) The other phrase is ‘in issues which are affecting patient care’. I think one, without being too long-winded, has to say that the way in which we carry out our work at the moment is that a group of professions will examine a problem. They will all put their different views about how the problem should be addressed, and they normally come to a common agreement. They then feel bound in honour to carry through that agreement. They are part of that agreement. If the situation changed, and if there were to be an executive manager, who took decisions in isolation, if he [sic] took decisions which were harmful to our patients then we would not feel bound to co-operate with him in carrying out that decision.
(…..) (Mr Winterton) But you will know that there are chief executives in local government and that professional people do in fact answer to him (sic) and he is in overall control. Are you saying that no professional person would be prepared to act on the instructions, whatever they may be, of a chief executive who does not have that qualification?
(Mr Grabham.) My assessment of my profession and the nursing profession is they would not be prepared to accept an instruction from a lay administrator if they thought it was going to damage the interests of their patients. ( )
(Mrs Short) That would mean that the general manager idea would be torpedoed presumably?
(Mr Grabham.) I honestly do not understand precisely what they mean by a ‘general manager’. If it is to say that one individual should be responsible for seeing that certain matters were carried out with expedition, matters outside the field of clinical care, one could accept that entirely. If one is to say that some lay administrator might make decisions in the face of advice to the contrary from medical or nursing professions then he would not, could not, expect the support of those professions (Social Services Committee, 1984, p. 4).
Other demands made by the BMA included the provision of an appeals mechanism against the decisions of a general manager. It also sought, in place of the general manager proposed by Griffiths, the election from within existing management teams of a chairperson, and a trial period for any changes which were adopted. It was also argued that management at the Unit level of organisation was best left to doctors and that the Management and Supervisory Boards should include clinicians (See British Medical Journal, Vol. 287, 1983, pp. 1321-2, 1643, 1811; Vol. 288, 1984, p. 84).
The nurses’ organisations did not take such a different view, though it was not so defiantly expressed: the Royal College of Nursing’s evidence concerning general management noted that
These recommendations, at the core of the Inquiry, have provoked the strongest reaction among RCN members. In general, members have expressed the view that while they can, to varying extents, sympathise with the analysis of NHS management inadequacies, they do not accept that the introduction of the general manager at region, district and unit can or will solve the problems (Social Services Committee, 1984, p. 16).
Similar views were expressed by the Royal College of Midwives, the Association of Nurse Administrators, and the Health Visitors Association (Social Services Committee, 1984, pp. 44-8). Not surprisingly, at least in the view of one of the Committee members, the NHS Administrators organisations (the Institute of Health Service Administrators, and the Association of Health Service Treasurers) were in favour of general management:
the Institute expects that many Administrators will be appointed as general managers because they possess the necessary skills based on experience, training, and their current responsibilities for coordination (Social Services Committee, 1984, p. 70).
(Mr Winterton) But are you not, as it were in favour of this probable change because you are very much in the riding seat and it is likely that most of your members will end up as the new chief executives and general managers, and you yourself have just referred to the drawing up of a job description and the additional remuneration. Is it not inevitable, therefore, that there is going to be conflict between you and other groups because you are the group that is going to benefit most from this change? (p. 73).
(By July 1984 the Institute had decided to re-name itself the Institute of Health Service Management: Hospital and Health Service Review, November 1984, pp. 301-4.)
Yet in his own evidence to the Committee, Mr Fowler was diffident; for example
(Mr Meadowcroft) If you have a district or a unit where the evidence to you from them on consensus or unanimity is that they are happy with the way they are working, decisions to them appear to be reached quite adequately and effectively, are you going to insist that they conform to a uniform pattern and have to appoint a general manager?
(Mr Fowler.) That is precisely the point Mr Winterton put to me. It is precisely the point we will have to consider as a result of the consultation. I cannot come to you and actually say we have made a decision on that point when we quite clearly have not. (Social Services Committee, 1984, p. 174.)
Mr Fowler’s apparent change of view about general management did not pass without comment at the time: interviewed in February 1984 by Peter Merry, Editor of Health and Social Service Journal, Fowler made a virtue of his position, presenting it as open-mindedness, though still managing to sound diffident:
PM You did indicate to the Select Committee that you had gone a little cold on the whole idea of the general manager. What are your views on the alternative models that have been put forward during recent debates, the idea of a rotating chairman, or introducing a general management function?
NF No, I think that’s a slight misconception. I didn’t say that I had gone ‘cold’ on the idea. What I said to the Select Committee was basically this: that we’re in the middle of considering the results of the many representations that have been made. It would be foolish from my point of view to actually say at this stage we have come to absolute firm and definite conclusions. If that was the position, there would actually be no point in asking for representation.
PM Comparing your stance on that with your initial response to the report, there’s quite a difference in the strength of your endorsements.
NF I don’t think there’s a tremendous difference. What we said at the time of the publication of Griffiths was that we accepted the broad thrust of Griffiths. As far as I can see, there were many things inside Griffiths most people inside the health service would accept
I think it’s also agreed that the general management function of the health service can be improved. There are few people, it would seem to me, who would argue that no improvements are possible at all. We have come to a particular debate because it is in a sense the easiest thing to home in on, and that is the position of the general manager himself [sic].
The only thing I would want to say at this stage about the general manager is that we would see the way forward there not in terms of experiments what we have been told is that there is general agreement about improving the process. There is considerable debate about precisely how that should take place and obviously at this stage we will have to be in the position of leaving our options open. But I wouldn’t want it to be thought that in any way we have stepped back from many of the improvements that Griffiths has put forward (Health and Social Service Journal, 23 February 1984, p. 221).
In its Report, published on 15 March 1984, the Social Services Committee welcomed the spirit of the Griffiths Report, but expressed the view, albeit obliquely, that the general management process did not require general managers:
The reaction to the Report has not been very enthusiastic. It has been interpreted as an attack on NHS staff, as a threat to clinical freedom, a blow to nurse management the Report does not always seem to appreciate the peculiar nature of the NHS the major difference is that the organisation of the NHS in management terms does not coincide with its professional organisation great caution has to be exercised in making assumptions about the possibility of creating mechanistic management hierarchies we are persuaded that there is room for improvement in management within the present limits of the system, in particular through Team Chairmen [sic] taking a more commanding role (Social Services Committee, 1984, pp. vii-ix; xxiii-xxiv).
In his immediate response to the Committee’s Report, Mr Fowler was still diffident:
I welcome this report and would like to thank the Committee for working so quickly. The report has many helpful suggestions and I am pleased to see the support it gives to the general thrust of the Griffiths Report. The Social Services Committee has made a most useful contribution to the current debate on the management of the NHS.
I was pleased to see that the Committee accepted the broad Griffiths message that we need to improve the management in the NHS and that this cannot be done fully within the existing management system. I am sure that the Committee are right when they reject proposals for experiments or pilot projects in NHS management as a suitable response to the Griffiths Report.
I will study the report with great interest and make a formal response in the usual way (DHSS, 1984e).
At the press launch of the Report, however, the Committee were less oblique than their text had been:
We don’t go along with Griffiths, we don’t go along with general managers (Mr Nicholas Winterton, quoted in Health and Social Service Journal, 22 March 1984, p. 338).
The Journal went on to comment that
What was more interesting was the almost incredible lengths Conservative members appeared to go in order to distance Norman Fowler from Griffiths. Mr Fowler’s initial enthusiasm for Griffiths has, of course, progressively waned as he has had to face the political pressures that would result from full blooded implementation (ibid., p. 338).
In the month following the Social Services Committee’s Report, DHSS spokespersons continued to leave the general manager question open. Mr Graham addressed a conference of the Institute of Health Service Administrators in April, but concentrated his remarks on the Griffiths prescription for changes within the Department. The Health and Social Service Journal commented that:
This exhibited the kind of tact one expects from the Department as Mr Fowler appears to be having cold feet on most of the other major bits of Griffiths (Health and Social Service Journal, 12 April 1984, p. 429).
The Social Services Committee’s Report was the subject of a poorly attended adjournment debate in the Commons on 4 May 1984. Opening the debate, Mr Fowler said that he wished to listen to views expressed before reaching final conclusions on the Griffiths Report; he hoped to publish such conclusions later in the month (Hansard, 4 May 1984, Col. 642). But it soon became evident that a decision about general managers had been made, even if there was to be some flexibility about details:
Though I have views about the basic Griffiths concept of the establishment of a personal and visible responsibility for general management at all levels of the Health Service, there is room for discussion about how it should be implemented. The purpose of the consultation in which we are engaged – and I hope that it will be the purpose of some of the speeches today – is to seek the advice of all those with an interest in how we can best introduce individual general managers into the Health Service. The many comments that we have received so far have helped greatly in clarifying areas where people feel that there will be problems and where they would welcome a lead from the centre (ibid, Col. 649, emphasis added).
Fowler was immediately questioned by a Liberal member of the Social Services Committee, but evaded further questioning:
(Mr Michael Meadowcroft) When telling us that health authorities will be given some flexibility in the timing of what they must implement, is it implicit in what the Secretary of State is telling us that they will have to implement some change? Is he now moving away from the extent of flexibility that he implied in reply to questions asked by the Select Committee?
(Mr Fowler) No. I have already made it clear that I support the general thrust of the report. There should be some flexibility, and timing is simply one of the areas in which we shall allow it. Timing is one of the central points that has emerged from the consultations and it is at unit level that flexibility with timing is most required. I am glad to have the Select Committee’s approval and support for my belief that local authorities should not go ahead with general managers on a pilot basis while others wait and see (ibid., Col. 650).
Towards the end of the debate, a Conservative member of the Social Services began to sound as if he repudiated the Report
(Mr James Couchman) The Select Committee, to avoid a split which would probably have been down party lines, produced a report that welcomed the general spirit of the Griffiths report, and then damned the report with faint praise with a set of slightly wishy-washy recommendations. I wish that the Select Committee had given my right hon. Friend the Secretary of State a firm lead to implement the Griffiths’ recommendations (ibid., Col. 690).
On 4 June 1984, in answer to a parliamentary question, Mr Fowler announced his decision:
The guidance I am giving health authorities today requires them to start work straightaway to establish the general management function and to identify individual general managers at authority and unit levels It requires regional authorities to make their proposals to me by the end of September, but allows district authorities until the end of 1985 to complete action at unit level (DHSS, 1986, p. 1).
The guidance to which the Secretary of State referred was issued to the NHS on the same day. As well as the usual circular (DHSS, 1984, f) setting out the action which health authorities were to take in creating and filling general manager posts, there was a letter from Mr Graham to chairpersons of authorities, seeking their co-operation in putting ‘all staff in the picture within 2-3 weeks.’ To this end, the letter enclosed a video of interviews with Messrs Fowler and Bett, a list of approved speakers on the topic of Griffiths, a question-and-answer brief for other speakers, and a professionally produced eight page, full colour printed leaflet for distribution to all staff. The comprehensiveness of these materials (a commonplace in subsequent government marketing of its policies) would have been difficult to achieve in the month between the Commons debate and the announcement of the government’s decision.
The question and answer brief sought to play down staff fears about general managers:
7.Will consultants be responsible to the general manager?
Consultants are clinically autonomous, in the sense that they take personal responsibility for the diagnosis, treatment and prognosis of their patients. They are not responsible to any ‘top doctor’, manager or even the health authority for their clinical decisions. The changes now being made will in no way alter this position. Authorities are, however, responsible for allocating resources to enable consultants to practice and for ensuring that their resources are used effectively and efficiently. An authority will therefore expect its general managers to be in regular discussion with consultants about the use of resources and to report to the authority as necessary.
8.What happens if doctors/nurses/professional officers disagree with the general manager?
f the disagreement is over a management decision, the general manager must fulfil his [sic] responsibility to see that a decision is taken, even if that means referring it to the authority itself. That is the job the authority has given him. If the disagreement is over a professional matter such as, for example, the level of pathology services necessary to support clinical work, the doctor or other professional will be able to refer the matter to the authority.
9.Does this mean the end of consensus?
It certainly means the end of management by consensus teams, but not the end of consensus in management. For in a multi-disciplinary organisation like the Health Service objectives can only be achieved when all parties are basically in agreement. The role of the general manager will not be to take decisions autocratically. It will be to build on the present consensus team approach, by ensuring that the team is led, and by resolving disputes. In the present situation no one has the responsibility to bring things to a head, and matters therefore float around unresolved for far too long. Worse still, because every team member has a veto, some proposals are never aired because the proponents feel it will not be possible to get a consensus (DHSS, 1984g, p. 4).
Not surprisingly, Mrs Renee Short, who had chaired the Social Services Committee, was less than pleased with the Secretary of State:
He has just ignored what we recommended. He has gone ahead and acted against the united medical, nursing and trade union opinion. It is rather extraordinary – he has accepted Griffiths hook, line and sinker I think it is a real cock-up. Typical Norman. He is a bit out of favour at the moment, as you may have gathered (quoted in Russell, 1984, p. 1843).
The members of the Griffiths team, though disappointed at the length of time taken by Mr Fowler to reach a decision, finally had their way. The whole incident has contributed towards securing a reputation for indecision on his part; according to one official such indecision was ‘a major problem’ (quoted in Davies, 1987b, p. 724), a view also expressed by several respondents to the present study.
On the other hand, it is likely that a reaction like that of the BMA to the general manager proposal would have given any Minister pause for thought: a powerful reaction from a powerful interest group. In the end, according to ‘insiders’ responding to the present study, Mr Fowler’s hand was strengthened (or ‘forced’ according to some) by the Prime Minister during the late spring of 1984; the alternative perspectives on this evidence are also held by professional DHSS-watchers:
Another of the things he’s [Fowler’s] done right is to keep David Willett [sic] her social policy adviser at No. 10 informed of everything he’s doing … (Observer, 5 May 1985).
Downing Street was pulling strings whenever the DHSS attempted any innovation such as general management (Davies, 1987b, p. 724).
In retrospect, it can be seen that the BMA’s posture could not easily have been sustained. Enough rank-and-file clinicians had expressed the view to the Griffiths team that they would welcome having one person in charge. (Though ‘in charge’ in this context may well have meant having someone more easily available to provide resources and solve problems for doctors.) And at one point in the Spring of 1984 Mr Fowler had lost his temper (by no means an unknown occurrence, by his own admission: Fowler, 1991, pp. 190, 206, 214, 219, 276) with the profession’s representatives, pointing out that, as an elected politician he occupied the high ground of legitimacy. In terms of the formalities of the Griffiths changes, then, the profession had suffered a major defeat. The BMA had complained at the perceived lack of time for consultation, challenged the concept of a non-medical chief executive, and demanded the retention of District Management Teams and the provision of an appeals mechanism against the decisions of a general manager. It also sought, in place of the general manager proposed by Griffiths, the election from within existing DMTs of a chairman, and a trial period for any changes which were adopted. It was also argued that management at the Unit level of organisation was best left to doctors and that the Management and Supervisory Boards should include clinicians (British Medical Journal, Vol. 287, 1983, pp. 1321-2, 1643, 1811; Vol. 288, 1984, p. 84). With the exception of the consultation period, extended because of the Social Services Committee’s enquiry, none of these preferences prevailed, and by July 1984 the BMA’s Annual Representatives Meeting was told by one of its officials that ‘management by managers’ was here to stay (British Medical Journal, Vol. 289, 1984). Ironically, later in the same year, official sources were still assuring the profession that policy towards DMTs remained unchanged (British Medical Journal, Vol. 289, 1984, p. 1470)!
For the nursing profession, the introduction of general managers entailed the loss of the right to be managed only by another member of the profession, and the concomitant loss of guaranteed promotion opportunities. In this sense, it overturned the victory won by nurses in the 1974 reorganisation. The initial reaction of representatives of the nursing profession was just as hostile towards the form of the Griffiths proposals than had been that of the medical profession. The views of the Royal College of Nursing, the Royal College of Midwives, the Association of Nurse Administrators, the Confederation of Health Service Employees, and the National Union of Public Employees were highly consistent. There was concern at the short consultation period, at the absence of the DHSS Chief Nursing Officer from the proposed Management Board, and at the absence of a trial period for the new management arrangements. There was a general desire to retain consensus decisionmaking (though the RCN was prepared to give up the veto power of each team member), and to retain a line relationship between District Nursing Officer and Directors of Nursing Services within Units. (See, for instance, Nursing Times, 4 July 1984, pp. 189; 8 August 1984, p. 19; 6 February 1985, p. 15.) There was resistance to the idea of nursing budgets being held by non-nurses and to the potential for a general manager to compel a nurse to ‘act unprofessionally’ (Social Services Committee, 1984, pp. 13-48). In general, then, there was a feeling that Griffiths had paid scant regard to the status or professionalism of nurses, a notion subsequently carried by the RCN into an anti-Griffiths national advertising campaign (Small, 1989, p. 55).
These concerns about the Griffiths proposals produced, on the face of it, a number of concessions on the part of the Government. The DHSS Chief Nursing Officer was included in the NHS Management Board (DHSS, 1984c), and although English Districts were not required to retain District Nursing Officers (as the profession’s representatives had hoped), they were required by the Secretary of State to provide for a senior officer to give nursing advice to the Authority (Nursing Times, 29 May, 1985, p. 16; 24 July, 1985, p. 19). On the remainder of the Griffiths changes, a degree of acceptance on the part of the nursing profession developed; like in the medical profession there were always some nurses who found it difficult to disagree with the generality of the Griffiths analysis, and some have criticised the profession for ‘creating a poor impression’ by its reaction to the report (Nursing Times, 13 March 1985, p. 19). Less than two years after the publication of the Griffiths Report, one RCN officer, whilst still unhappy at the absence of compulsory posts of District Nursing Officer, was generally reassured about the form of the changes (Rowden, 1985, p. 20).
Postscript: further changes on the policy agenda
As was noted in Chapter 1 further organisational changes followed the Griffiths reforms. These changes were the outcome of a year-long prime-ministerial review of the NHS. This review was the product of widespread concern about the level of NHS funding.
In part, this concern reflected the disappointment of health authorities at budget allocations for 1987-88, and at the readiness of the new Secretary of State, Mr John Moore, to concede to Treasury pressure in the public expenditure round of that year (see Health Service Journal, 1987, passim). In addition there were decisions by several major interest groups (the King’s Fund Institute, the National Association of Health Authorities, and a combination of the BMA, Royal College of Nursing and Institute of Health Services Management) to commence their own enquiries into NHS funding. Not surprisingly, the same concerns came to be reflected in Parliament (see, for instance, Health Service Journal, 12 November 1987, p. 1316), and by the end of the year the Social Services (Select) Committee had decided to conduct its own enquiry (Health Service Journal, 17 December, 1987, p. 1458), and even prominent Conservative MPs such as Mr Barney Heyhoe (a former Minister of State at DHSS) and Mr Nicholas Winterton (a member of the Social Services Committee) joined the public call for additional funds. Finally, substantial media coverage had been given to reports of delays in urgently needed treatment of some children’s cardiac conditions (see, for instance, Health Service Journal, 26 November 1987, p. 1369). The predominant mood was crystallised in December in a statement by the presidents of the Royal Colleges of Physicians, Surgeons, and Obstetricians and Gynaecologists, calling in the strongest language for more funds (Leathard, 1990, p. 129).
Despite occasional calls for radical change from the political right (see for instance, Health Service Journal, 29 October 1987, p. 1249; 14 January 1988, p. 46), the position of Mr Moore was that no major changes were required. As one respondent to the present study put it, the government was prepared to ‘tough it out’, even to the point of a media battle with the BMA. In early January 1988 Mr Moore stated publicly that the government had no plans for a formal review of the NHS (Health Service Journal, 14 January 1988, p. 29). On 14 January, two right-wing think-tanks published proposals for (rather different) radical changes in the NHS (Adam Smith Institute, 1989; Centre for Policy Studies, 1989).
On 25 January the Prime Minister, (without having previously informed Parliament), announced on the television programme Panorama that just such a review would in fact take place (Health Service Journal, 28 January 1988, p. 103). It subsequently emerged that the review was to be conducted by politicians rather than being treated as a formal Committee of Inquiry: the reviewers were initially the Prime Minister, Mr Moore and Mr Tony Newton (DHSS), Messrs Nigel Lawson and John Major (Treasury) and after some dispute Messrs Malcolm Rifkind and Peter Walker (Scottish and Welsh Offices, respectively) (Brown and Timmins, 1988, p. 5; Paton, 1992, p. 42). The aim was to allow radical ideas to be considered without the risk of a repetition of the CPRS leak of 1982 (see above) (Willetts, quoted in Brown, 1988).
Although the review had been established in response to issues about the amount of NHS funding, media analysts were quick to assume that funding methods would be the prime focus (Timmins, 1988, p. 19). It was also assumed that the work of the working party on alternative finance (see above) which Mr Fowler had shelved would be disinterred (Healthcare Parliamentary Monitor, 22 February 1988, p. 1). In May it was confirmed that the review would include primary care, rather than, as originally believed, only hospital care (Health Service Journal, 19 May 1988, p. 549).
The reviewers worked throughout 1988, during which time the DHSS was split into separate components of Social Security and Health, the latter new department (DoH) being headed by Mr Kenneth Clarke, with appropriate modifications to the review team membership. The assiduously maintained private status of the review (Cook, personal communication 1988) meant that little is yet known about the process by which it reached its conclusion, though indirect evidence is provided by the pamphlets submitted by a number of right-wing policy organisations such as the Institute for Economic Affairs (for a review of these, see Paton, 1992, ch. 3; Kendall and Moon, 1990, pp. 108-12), and by press ‘leaks’. The general picture is one of the relatively early abandonment of more radical policy options, such as restructuring the NHS along the lines of American health maintenance organisations (Times, 26 February 1988, p. 5), or allowing citizens to opt out of paying for, and receiving, NHS services (Times, 16 May 1988). Just as in 1982, the evident problems of other countries’ health systems, in particular the U.S.A., had served to highlight the degree of control which central funding gives to government, and the degree of comprehensiveness of the service (Healthcare Parliamentary Monitor, 25 April 1988, p. 2; Times, 20 January 1988, p. 10).
According to Paton (1992, p. 44), the inquiry then went through a brief phrase in which reform seemed likely to take the form of a strengthening of management, resource management and clinical audit, rather than major structural change. By the summer of 1988, however, the probability of some kind of purchaser/provider split and ‘internal market’ (with intellectual origins in the work of the American economist Enthoven: 1985) had become stronger. Paton (1992, p. 45) states that this was very much at the Prime Minister’s insistence, though (and contrary to Paton’s assertions about ministerial preferences) circumstantial evidence from press reports is that the shift had occurred even before the split of the DHSS in July 1988 and the arrival of Mr Clarke as Secretary of State (Health Service Journal, 1 July 1988, p. 747; Guardian, 27 July, 1988, p. 1; Times, 14 October 1988, p. 6; Health Service Journal, 24 November 1988, p. 1374).
The logical appeal of such an approach as a potential vehicle for competition and solution to the ‘efficiency trap’ did not make the detailed design of new policies any easier, and neither the white paper Working for Patients (DoH et al, 1989) published in January exactly one year after the establishment of the review, nor its subsequent working papers were very specific; the Health Service Journal judged that, even after a year, health ministers were ‘devising policy on the hoof (Health Service Journal, 23 February 1989, p. 221). On 23 February 1989, the government published controversial proposals for radical changes in the contracts of GPs (Department of Health and Welsh Office, 1989; Times, 24 February 1989, p. 1).
As with the Griffiths reforms, much attention was given to ‘marketing’ the new policies. Senior NHS managers were confidentially briefed by the Secretary of State via a video link (McVerry and Beavers, 1992), other managers received briefing packs and staff and the public received glossy booklets. Nevertheless, the government faced a good deal of opposition in the form of a critical Social Services Committee Report in July 1989 (Social Services Committee, 1989), a legal challenge (Health and Social Service Journal, 8 February 1990, p. 181), and opposition from the BMA:
[BMA Council] does not believe … that the changes proposed would achieve [the government’s stated] aims. Indeed, it is convinced that many of the proposals would cause serious damage to NHS patient care, lead to a fragmented service and destroy the comprehensive nature of the existing service. The Government’s main proposals would appear to be to contain and reduce the level of public expenditure devoted to health care. The proposals would undoubtedly increase substantially the administrative and accountancy costs of the service, and they ignore the rising costs of providing services for the elderly and of medical advances. In the absence of any additional funding the proposals would inevitably reduce the standards of NHS patient care (British Medical Association, 1989, p. 2).
By mid 1989 there was a widespread perception that the government was losing political ground on the issue (Timmins, 1989, p. 25), circumstantial evidence of which continued to be apparent in opinion polls throughout 1990 and 1991 (see, for instance, Independent, 25 October 1991, p. 5).
Nevertheless, the new GP contract was imposed by the government with effect from April 1990, and the necessary legislation for the other reforms (The National Health Service and Community Care Act, 1990) became law in June 1990, effective for the most part from April 1991. At its Annual Representatives Meeting in June 1992, the BMA formally ended its campaign against the changes.
4 The impact of general management
In attempting to assess the impact of general management in the NHS from its introduction until 1988, this chapter is divided into four main sections. The first provides a pre-Griffiths ‘baseline’ against which the study’s findings can be compared. The second assesses the impact of general management at national level, both in the sense of the Griffiths changes within the DHSS, and in the sense of the appointment of general managers across the English NHS.
The third section reports largely interview data from two DHAs (see Chapter 1 above), with some material from RHAs and CHCs. The fourth section provides both a summary and a comparison of the findings of the present study with those of other contemporary research. As in the two preceding chapters, there is a postscript relating to the Working for Patients changes, in this case reviewing such little evidence as is currently available concerning their early impact.
Establishing a baseline
Chapter 2 provided a brief summary of the findings of some 25 empirical research projects, concerned with NHS management, and carried out between 1966 and 1982. These were summarised, at that stage, by applying to the typical pre-Griffiths NHS manager the label ‘diplomat’. (A more extensive review may be found in Harrison 1988a, ch.3.) It is not necessary to repeat the literature summary here, but rather to structure it into four basic propositions about pre-Griffiths management. These can then be used as a baseline against which to view the findings of the present study. The four propositions are as follows.
Firstly, managers were not the most influential players in the service, an observation which extends to managers in the DHSS. Influence was to some extent distributed around the various occupational groups in the service, but amongst these the doctors were pre-eminently powerful. Some of this influence was channelled through organised groups, such as the BMA and Royal Colleges, and incorporated into central government decisionmaking processes. (See Harrison, Hunter and Pollitt, 1990, ch. 4; Haywood and Hunter, 1982). However, as Chapter 2 made clear, much influence was local in character, and exercised as much through ordinary doctors’ use of ‘clinical freedom’ to determine the pattern of local health services as through micropolitical manoeuvrings. One effect was ‘lowest common denominator’ decisionmaking (Harrison, 1982).
Secondly, the behaviour of NHS managers was largely reactive, rather than goal-seeking (or proactive), in character. This is, of course, a matter of degree rather than of absolutes; Larson et al (1986, p. 338) have pointed out how difficult it can be to apply these labels to actual managerial behaviour. Suffice it to say that the pre-Griffiths NHS manager was not generally responsible for setting his or her own work agenda. Rather than setting objectives, he or she reacted to problems.
Thirdly, the most important sources of agenda-determining problems for NHS managers were inside the organisation. Managers responded to problems raised by professional groups, especially doctors, and trade unions, rather than to problems raised by patients, relatives, citizens or CHCs. NHS management, one might say, was producer oriented.
Finally, change in the NHS was largely incremental in character. ‘Incremental’ here means that it occurred by accretion to the status quo, rather than by dismantling it. This usage corresponds to Lindblom’s notion of ‘incremental analysis’ rather than ‘incremental polities’:
Simplification is systematically achieved in two principal ways …. it is achieved through limitation of policy comparisons to those which differ in relatively small degree from policies presently in effect …. [and] it is necessary only to study those respects in which the proposed alternative and its consequences differ from the status quo (Lindblom, 1959, p. 84).
In other words, the organisational status quo was taken for granted as good, and not subject to any review or evaluation.
Three features of this summary are striking. Firstly, all four elements of the ‘diplomat’ manager are inversions of classical textbook stereotypes. In this literature the entire notion of organisational hierarchy assumes managers to be authoritative (Weber, 1947); the manager’s first task (in logical terms) is to set objectives (Stewart, 1979, p. 66); successful organisations should be customer-responsive (Drucker, 1955, Ch. 5); and the manager should evaluate organisational activity (Stewart, 1979, p. 67).
Secondly, each of the four elements of research findings corresponds to an element of the Griffiths diagnosis as summarised in the preceding chapter. Thus, the Griffiths report sees no single person in charge, whereas the research identifies the diffuse, localised power of doctors. Griffiths complained of weak implementation of plans: what managers failed to do. The research identifies what managers did do: tackle ongoing problems instead. Griffiths identified a lack of management concern with consumer views, whereas the research shows management concern with producer views. And Griffiths’ lack of performance orientation corresponds to the research finding concerning incremental change. These correspondences are summarised in Table 4.1.
Table 4.1
| Correspondence of Research Findings 1966-82 with the Griffiths Reports Diagnosis | |
| Research Findings | Griffiths Diagnosis |
| Collective influence of doctors rather than individual influence of managers | Lowest common denominator decisions, no-one in charge |
| Reactive, problem solving behaviour dominant | Lack of concern with implementation |
| Priority to servicing internal, organisational demands | Lack of attention to consumers |
| Incremental change to status quo | Lack of performance orientation |
See text for explanations.
It should be noted, however, that the Griffiths Report adds a value judgement to the agreed set of ‘facts’. The term ‘diagnosis’ clearly implies a situation which is unsatisfactory, a perception not necessarily shared by the various researchers, and, as noted in Chapter 2 above, not the received wisdom of the 1970s and early 1980s. As a result, there was little conflict between doctors and managers. No doubt doctors sometimes felt that managers did not fully understand their needs (Medical Services Review Committee, 1962, pp. 110-111) but Heller (1979, pp. 1, 45) and Petchey (1986, p. 100) are mistaken in arguing that managers have long striven to rationalise the Service and consequently that its shape is a product of their conflicts with the medical profession. Nor is Klein (1985, p. 60) necessarily correct in arguing that doctors and managers have conflicting value systems. On the contrary, and in contrast to local authority social service departments (Kakabadse, 1982, p. 109), there has been a remarkable homogeneity of culture in the NHS. Doctors and managers have shared common values (Brown, 1979, p. 191), and common hierarchies in terms of the status attached to particular medical specialties and to acute, teaching hospitals (Schulz and Harrison, 1983, p. 44). (The major conflicts which occurred prior to 1982 were in the field of industrial relations; Barnard and Harrison, 1986; Seifert, 1992.)
The third striking feature of the four elements of pre-Griffiths management is that one of them may well explain the others. To put it rather crudely, if managers were not die most influential players in the organisation, then it would not be surprising if much of their energy was expended in providing facilities and solving other problems for doctors, rather than in reviewing the performance of medically-led services. The influence of the doctors can, therefore, very much be seen as a key to the practice of pre-Griffiths ‘diplomat’ management. By the same token, it is a key to the evaluation of the impact of the subsequent Griffiths changes.
The impact at national level
It was noted in Chapter 3 above that the government had decided immediately upon the publication of the Griffiths Report to implement its recommendations concerning the internal organisation of the DHSS. Despite departmental pressure for the Chairman (sic) of the NHS Management Board (in effect, the General Manager for the NHS in England) to be placed in a line responsibility to the Permanent Secretary, an early decision was made that the Office holder should be of second Permanent Secretary rank, responsible to the Secretary of State, and acting as accounting officer for most NHS expenditure (Social Services Committee, 1984, p. 167). It proved impossible to recruit Mr Griffiths to the post, and it was not until December 1984 that, as noted in Chapter 2, Mr Victor Paige’s three year appointment was announced.
The first eighteen months of Paige’s incumbency gave rise to a good deal of criticism from various quarters. It took more than six months to fill all the posts on the Board (Paige, 1985, p. 205), during which time the Board and its Chairman were largely unseen within the Service (Health and Social Service Journal, 24 April 1986, p. 361), having apparently been sucked into civil service inertia (Coad, 1986, p. 755):
Mr Paige in the next office along from his fellow second permanent secretary, the chief medical officer, surrounded by the same pot plants and the same civil servants (Halpern, quoted in Small, 1989, p. 31).
In June 1986, Paige resigned in circumstances which suggested, as some commentators on the original Griffiths proposals had feared, that there had been difficulties in reconciling political and managerial considerations (DHSS, 1986a; Barnard and Harrison, 1984) on such issues as efficiency savings and the closure of nurses’ homes (Davies, 1986a; Petchey, 1986, p. 101; Small, 1989, pp. 47,56). His letter of resignation approached the point elliptically:
The Management of the NHS is complex. Ministers and the Chairman of the Management Board can approach the same issue with different perspectives, priorities, objectives and restraints. The conclusions are not always compatible. Also there are always others in the action – or trying to be! Within my remit that makes for difficulties in working to the management standards and style to which I am committed. I have brought this to your notice on several occasions. You are aware that it is not working out as I believe it should. After much careful thought and with great sadness I have therefore decided to resign as the Chairman of the Management Board (DHSS, 1986a, p. 1).
In his subsequent autobiography, Mr Fowler conceded ‘I have to admit that he had a point’ (Fowler, 1991, p. 196). In fact, rather than having been (as the health service press had implied) too weak, Mr Paige seems to have been too assertive; the following quotations are from ‘insider’ respondents to the present study:
He went for ministers head-on, and lacked subtlety in his dealings with civil servants.
He tried to fight ministers but was poor at it.
He expected management considerations to trump political ones.
The revised arrangements for the Management Board, set out in Chapter 2 above, represented a formal reassertion of political control (there had been the inevitable speculation that Griffiths might succeed Paige: Health Service Journal, 24 July 1986, pp. 971-2) and a rejection (though it transpired not to be a permanent one) of Griffiths’ formula for the separation of politics and management. To the Health Service Journal, with its generally managerial perspective, this made little sense:
It is hard to resist the observation that if Florence Nightingale came across the new look NHS management board she might have some difficulty in working out who was in charge. The structure announced by Social Services Secretary Norman Fowler last week ( ………) looks as if it was agreed by a very large committee. But then Mr Fowler is capable of behaving like a very large committee all on his own. In many ways the new structure will be seen as a step backwards. It is a retreat from the notion that once the government has decided on policy, it will be left to professional management to carry it out. Despite protestations by Mr Fowler and even by Sir Roy Griffiths himself that the original principles of general management are not being diluted, not everyone in the NHS will be totally convinced. The manner in which the boundaries between policy and implementation have been drawn might raise a few suspicions. For instance, the decision to install Health Minister Tony Newton as chairman of the management board means that boundary becomes blurred at board level. Yet elsewhere in the DHSS the policy groups still sidestep the management board and theoretically report to the supervisory board. If the minister is on the management board there is no reason why the policy groups cannot report to it. Someone, somewhere seems to be having his/her cake and eating it (Health and Social Service Journal, 9 October 1986, p. 1307).
The Management Board had also endured a second, highly if briefly publicised, problem. Mr Cliff Graham, who had led the Griffiths inquiry support staff, and subsequently led much of the implementation effort (see Chapter 3 above), had, along with his immediate superior Mr Graham Hart, been appointed to the Management Board in April 1985 (DHSS, 1985c, p. 1). Graham suddenly left his post on 31 July 1985 for a University sabbatical (Health and Social Service Journal, 1 August 1985, p. 944). One journalist who had been particularly close to the Griffiths inquiry explained the event thus:
The reasons for his departure are less than straightforward. As with all these events there was no doubt an element of soap opera that is of little value except as gossip. But there was a great deal of tension within the Department and there is a certain significance for thehealth service in why some of the friction existed ( ) But the almost messianic zeal which Cliff Graham generated for general management had to be tempered to fit into the bureaucracy of the management board …. In simplistic terms Mr Graham is said to have wanted to go on tilting at windmills while the mandarins in the Department wanted to proceed with the bureaucratic task (Halpern, 1985b, p. 975).
In other words, Graham did not subscribe to what has subsequently been referred to as Whitehall’s ‘disbelief system’ (Metcalfe and Richards, 1990, pp. 18-9). No doubt this was a fair assessment. But in the context of the present study it is worth being more specific about one particular issue which contributed to his departure: the retention of parallel medical and administrative hierarchies within DHSS was the very antithesis of Griffiths’ notion of general management.
Overall, the impact of the Griffiths changes within DHSS was not great. There were some achievements; for instance, respondents to the present study were clear that the introduction of Performance-Related Pay to the NHS over a period of eighteen months in 1985-86 could not have been achieved by the civil service at anything like a comparable pace. But this was seen very much as a personal achievement of Mr Peach, with little or no evidence of corporate working on the part of the Management Board. It is also probable that the expectations of the Board’s being able to keep the NHS out of politics were unrealistic (Barnard and Harrison, 1984) given its importance in terms of both public expenditure and public opinion (see Chapter 3). Nevertheless, the subsequent removal of the Management Board’s successor to Leeds in 1992 indicates that there is some ministerial, as well as managerial desire, for such separation.
It is difficult to find very much at all to say about the Supervisory Board. According to ‘insider’ respondents to the present study:
Its initial purpose was to cover the Management Board from political fallout, but later it had no purpose.
It was a muddle throughout. And after the changes following Paige’s resignation it virtually never met.
Given the ministerial role in policy, and its support from DHSS ‘policy divisions’, and given the Griffiths team’s and the government’s own rejection of the possibility of creating some sort of agency status for the NHS, the rationale for the Supervisory Board (and its successor) is not easy to understand.
Griffiths’ own subsequent verdict on the Departmental changes was that
The Supervisory Board and the Management Board were absolutely correct in concept but half-hearted in their implementation. Major policy issues were left uncovered. There was no attempt to establish objectives at the centre and no concentration on outcomes (Griffiths, 1992, p. 65).
A different aspect of the national level impact of the Griffiths changes is the process and pattern of general manager appointments across England. Despite the assurances given in Fowler’s letter of June 1984 to chairpersons of health authorities that general managers would normally be appointed from existing officers, by October of the same year a member of the Management Board informed the conference of the newly renamed Institute of Health Service Management that
Ministers are hoping and expecting to see general managers being drawn from a variety of backgrounds inside and outside the health service (Mr Graham Hart, quoted in Health and Social Service Journal, 25 October, 1984, p. 1258).
Indeed, the determination of Mr Clarke to ensure that the exercise was ‘not simply a walkover for existing Administrators’ led to the much-publicised veto of a number of proposed appointments of such persons (Timmins, 1985; Small, 1989, p. 50), sometimes, allegedly on grounds of mistaken identity. There seems to be no evidence, however, that Ministers or the Department tried to secure particular appointments.
Table 4.2 summarises the situation at the end of the appointment process. It is immediately apparent that, despite the highly-publicised vetoes, the penetration by persons from outside the NHS had been low. More than 60 percent of posts had gone to Administrators or Treasurers, overwhelmingly in the Authorities within which they already worked (Alleway, 1985, p.1121). Many of the doctors appointed at Unit level of the organisation were clinicians who continued to undertake some clinical duties (Sherman, 1985, p. 152; Manpower Policy and Practice, Winter, 1986, pp. 14-5). Despite remarks by Lady Trumpington (the government health spokeswoman in the Lords) to the RCN Conference that nurses should not be discouraged from applying for general manager posts (DHSS, 1985d, p. 1), the profession fared relatively poorly, obtaining less than ten percent of posts, largely concentrated in lower-paid community unit roles.
Table 4.2 The Background of NHS General Managers
|
Regional General Manager
|
District General Manager
|
Unit General Manager
|
% OF ALL
|
|||||
| Former occupation | 1986 | 1987 | 1986 | 1987 | 1986 | 1987 | 1986 | 1987 |
| NHS admin. and finance | 9 | 9 | 132 | 132 | 364 | 355 | 62% | 61% |
| NHS medicine | 1 | 1 | 15 | 16 | 110 | 110 | 15% | 16% |
| NHS nursing | 1 | 1 | 15 | 16 | 110 | 110 | 15% | 16% |
| NHS other | – | – | – | – | – | 14 | – | 2% |
| Outside NHS | 3 | 3 | 38 | 36 | 54 | 57 | 12% | 12% |
| Vacancies | – | – | 2 | 2 | 13 | 4 | 2% | 1% |
| Total | – | – | 2 | 2 | 13 | 4 | 2% | 1% |
Sources: (October 1986), M. Syrett, ‘NHS Management: Here to Stay?’, Manpower Policy and Practice, Winter 1986, pp. 10-11. (December 1987), A. Leathard, Health Care Provision: Past, Present and Future, London, Chapman and Hall, 1990, p. 89.
Percentages do not necessarily sum to 100 due to rounding.
Of the twelve percent or so from outside the NHS, some one-third were retiring officers from H.M. Forces (Alleway, 1985). It is possible to calculate that, up to mid-1987, the attrition rate amongst (all) ‘outsiders’ was some ten times that of those appointed from within the NHS: 22 percent compared with 2.5 percent. Although the then Chief Executive of the NHS argued that thiese figures were not unreasonable (Peach, 1987, p. 4), many of the departures were highly publicised, and it is therefore possible to attempt some analysis of the circumstances, based on the acceptance of press reports at face value. The following is based on twelve reported cases between March 1986 and July 1988 (Health Service Journal, 21 March 1986, p. 408; 8 May 1986, p. 610; 22 May 1986, p. 680; 14 August 1986, p. 1066; 16 April 1987, p. 434; 7 May 1987, p. 516; 23 July 1987, p. 834; 26 November 1987, p. 1367; 4 February 1988, p. 136; 2 June 1988, p. 606; 11 September 1986, p. 1176). All the reported cases contain some suggestion of disagreement between an ‘outsider’ general manager and the health authority, sometimes directly, sometimes indirectly through disagreements with consultant medical staff. In a large majority of cases, there is a reference to differences of preferred management style, and a fairly clear implication that the general manager wished to change things faster than others wished; for example
‘he tried to scythe through customs and traditions’ said one source (Health Service Journal, 16 April 1987, p. 434).
The remaining small minority of cases illustrates the reverse; general managers resigning in protest at being required to make financial savings.
The impact of general management in two districts
This section sets out the findings of die present study in respect of the two districts in which fieldwork was conducted; details of these districts were set out in Chapter 1 above. The findings were not, as it transpired, very different between the two districts, so that it has not been necessary to structure their presentation into separate subsections. Instead, the findings are structured along the lines of the four elements employed earlier in this chapter to summarise the baseline of pre-Griffiths research findings; it should be noted, of course, that these elements are not exclusive of each other, so that some points could have been made under more than one heading.
The extent of managerial influence
Few of the respondents in either district held the view that, in general terms, the introduction of general management had led to any substantial shift in the balance of influence between managers and doctors. This view was consistent both across disciplines and up and down the hierarchy. Sometimes, the key problem was seen in contractual terms:
Griffiths has made no difference to the management/doctor relationship because DHAs don’t employ doctors (Consultant Pathologist, London DHA).
We wanted to put a clause into Consultant contracts requiring them to be involved in [management] budgeting arrangements, but this was opposed by both the profession and the RHA (Director of Personnel, London DHA).
The location of consultant contracts, abandoned as an issue by the Griffiths inquiry team, was thus symbolically important for many respondents: almost an indication of ‘bad faith’ (Pollitt et al, 1990). This feeling that doctors were to be barely touched by general management was also prevalent amongst doctors themselves:
[General management] is something that they get on with up there [at District HQ]; it doesn’t affect us (GP member of District Management Board, Northern DHA).
Management stops at the consulting room door (Consultant Obstetrician, Northern DHA).
Management has nothing to do with what I do (Consultant Physician, London DHA).
Although a younger generation of consultants was in general more approachable and informal than its predecessor, other professions were frequently able to point to instances of unchanged, and unacceptable, medical behaviour:
One particular consultant regularly swears at my [sic] nurses, but the Unit General Manager won’t do anything about it; no matter what happens, they [doctors] will do what they want (Senior Nurse Manager, London DHA).
Management have not got the real power to act against the few clinicians who don’t give two hoots (Consultant Geriatrician, London DHA).
Managers in both Districts were aware of poor timekeeping by doctors in outpatient departments and in operating theatres, with consequent extensive queuing and overrunning lists respectively:
[Surgeons] come and go as they please (Consultant Anaesthetist, Northern DHA).
In both cases, management action had been confined to circular memoranda asking all clinicians to bear the problem in mind. In one district a particular consultant’s lack of interest in a certain surgical procedure meant an ever-lengthening waiting list. The solution was to spend some £100,000 to pay for operations elsewhere until the offender’s retirement three years thence:
No-one will grasp the nettle (GP member of District Management Board, London).
Medically qualified Unit General Managers (UGMs) were no more likely to act assertively in these matters than were managers from other backgrounds. For some respondents, the Griffiths changes merely served to divert attention away from doctors’ activities:
No-one can control consultants: they influence everything, and this has got worse since Griffiths because the constant reorganisation of the Unit’s management structure has diverted attention away from their activities (Senior Nurse Manager, London DHA).
There are excessive numbers of juniors [medical staff]; they only work a one in four or five rota and there are no type B units of medical time [lower paid elements of on-call overtime] (Operational Services Manager, Northern DHA).
In the London district, private practice by consultants was quite extensive, especially following the 1980 relaxation in the consultant contract, so as to allow even whole-time NHS consultants to undertake it. The effect was both to undermine the collegiality of the hospital, to make it less manageable and to make surgeons, in particular, immune from criticism:
No-one’s [from the medical profession] around the hospital at lunchtime, so no-one goes to meetings. And no anaesthetist ever disagrees with a surgeon (Consultant Pathologist, London).
As distinct from these general views about the medical/managerial balance of influence, there were consistent responses which suggested a shift of influence in one specific area. This related to the districts’ straitened financial circumstances (see next subsection); general managers were much more easily able than their predecessors to make changes of the ‘cuts and closures’ variety. Thus in both districts, ward closures or service curtailments were
an important financial safety valve (Director of Finance, London DHA).
As a further result, doctors were increasingly aware that managers would detect ‘creeping developments’: changes in clinical practice – whether in terms of ‘hardware’ such as more expensive prostheses, or practices such as admission policies – which had financial consequences for the organisation visible to managers only in retrospect. Doctors’ perceptions of managers’ concerns in this area, combined with slowly improved information and budgeting systems, led many to be more circumspect than before and to consult managers in advance of changing practice. It was no longer easy to obtain even relatively small amounts of money by informal means, even though consultants in Northern DHA retained the right of direct access to the DGM:
I can’t take the administrator [sic] out for a beer and get a new cystoscope anymore (Consultant Neurologist, Northern DHA).
By the same token, a few slack resources in conditions of scarcity could be made to go a long way in terms of influence (Stephenson, 1985, p. 157):
I can buy a Consultant for £1,000 for an Amstrad [microcomputer]; just like a boy with a toy, which is what he is [sic] (UGM, London DHA).
Much of this was neatly summarised by one respondent, more favourably inclined than most towards the Griffiths changes:
Griffiths has concentrated the mind here; made people address a problem that they strongly resisted before, that is medical people’s clinical freedom and being demand-led in the face of finite resources (District Physiotherapist, Northern DHA).
As noted already, senior management respondents to the present study did not exhibit distinctive perceptions on matters of medical influence; thus, whilst general managers and other chief officers prided themselves on ensuring that decisions were actually taken (rather than issues simply being avoided), only a few claimed that the speed of decisionmaking had been improved or that their implementation was now more certain:
The DGM is a focal point and an arbitrator; where senior officers don’t agree upon a matter the issue does not simply get lost as it did under the old consensus system [but] decisions are no quicker as a result of Griffiths Griffiths has not made the implementation of decisions any easier, though there is some small potential for change, and managers are now able to ask more searching questions of doctors (Director of Planning, London DHA).
General managers themselves rarely expressed a desire to increase direct control over doctors; rather, their aspirations tended to be phrased in terms of a desire to change the organisational ‘culture’ to one in which doctors (and others) became more accountable for their actions, more aware of their broader consequences:
The prime role of general management is to change attitude and culture in the NHS though this is impossible overnight. We might be able to see change in three [more] years, though I can see light at the end of the tunnel. But progress is painfully slow (DGM, London DHA).
The approach in the London district, whose DGM had been influenced by In Search of Excellence (Peters and Waterman, 1982), was to be one of the first in the field with a statement of district philosophy, which had been promulgated via the in-house newspaper, hospital notice-boards and the staff handbook:
It is the philosophy of the London Health Authority:
- To provide continuing health care support and education for each individual and ethnic community in London ensuring the highest quality of patient care.
- To provide our employees with stability, job satisfaction, appropriate remuneration and good working conditions, promoting employee involvement on all matters affecting their work.
- To conduct our business with due care for the general public and the environment.
- To inform and account to the public, patients, staff and all other relevant bodies on the health care needs in the borough, our policies, plans and performance, and to discharge our statutory duties with integrity and openness in the most cost effective manner.
Familiarity with this philosophy was not, however, exhibited in interviews with respondents in the district other than members of the District Management Board (DMB), who claimed a degree of success for it:
General management and our philosophy are a success, but I can’t really say how (District Medical Officer, London DHA).
Our strategic and short-term plans are living – part of the culture -not just sitting in the bookcase (Director of Planning, London DHA).
The approach in Northern DHA was more prosaic: to encourage the developing trend of medical recognition of ‘creeping developments’ (see above) to turn into a series of planning agreements with groups of clinicians. (Further discussion of this takes place in the next subsection).
So far as management influence in other, non-medical, directions is concerned, respondents had noticed some differences. Firstly, the Chairmen of the DHAs were more visible and involved than their predecessors had been, though since both had been appointed around the time of Griffiths, it is difficult to disentangle the organisational changes from differences in style. Moreover, the approach of senior managers in both districts was to treat the chairman and other members of the Authority simply as a constraint, around which implementable policies had to be constructed:
The Authority is not supine, but it only reacts to what we give to it (Director of Planning, Northern DHA).
A second difference which respondents readily perceived was the ability of general managers to modify formal organisational structures. As noted in Chapter 1, both DHAs had had a number of general manager changes since the original implementation of Griffiths. Each new general manager had brought his or her own ideas, which could now be more freely introduced than before Griffiths. Not surprisingly, many lower-level respondents, who had been in post throughout the changes, took a rather jaundiced view of this constant ‘rearrangement of the pieces’, seeing it as a substitute for more substantive action
A third difference was that general managers were seen to have acquired a degree of control over non-medical professionals that had not been possessed by their administrative predecessors. Thus, nurses had been challenged on the necessity of long overlaps between shifts, and physiotherapists forced to address the continued need for certain routinely-provided exercises. In addition, nurses in both districts had been forced to decentralise to some extent, with ward-level budgets for consumable items, sub-unit staffing budgets (both of which had been received with a degree of enthusiasm by middle and junior nurse managers) and the complete removal of one tier of the nurse management hierarchy. For one sub-unit manager, however, this had not gone far enough:
I’m well-paid, but I pick up all the crap. It’s always me that’s making changes, making cuts and so on. Nursing gets away with excuses for not showing leadership, and instead spends its time looking at [patient] dependency levels, arguing about staffing (Operational Services Manager, Northern DHA).
One final difference, potentially significant for general manager influence, to emerge from the study is that, despite the grumbles and the frequent perceptions of general managers’ lack of achievement, the institution of general management was regarded as highly legitimate, both by doctors and others: no sign of a BMA or RCN insurrection here:
The main benefit of Griffiths is that someone is in charge (Consultant Psychiatrist, London DHA).
The NHS was crying out for strong management (Consultant Physician, London DHA).
We lacked a disciplinarian: I welcome this (Consultant Surgeon, Northern DHA).
You need general management: someone at the end of the day who makes decisions: one supremo (sic) (District Nurse Adviser, Northern DHA).
I believe in the philosophy of general management. I’d like to pursue it as a career (Senior Nurse Manager, also RCN branch officer, London DHA).
I still believe in general management, even though it’s [largely] turned out to be jobs for the [administrative] boys [sic]. They’re the ones who know how to manage their image. (UGM – a nurse by background – London DHA).
Proactive and reactive management
Despite the proactive paraphernalia of the Griffiths and contemporary reforms (such as the review process, IPR, and PRP) the continuing evidence of reactive managerial behaviour is strong. In particular, both districts were pervaded by financial pressures. The effect on DMB agendas was marked:
We have concentrated on keeping within the funds available possibly to the detriment of quality of care (DGM, London DHA).
The association of the Griffiths changes with resource shortages in the NHS is extremely unfortunate. It’s rendered the whole exercise somewhat less than credible (UGM, London DHA).
The [District Management] Board’s agenda is dominated by the resource issue it’s displaced our efforts. There’s an opportunity cost; we could have been looking for cost improvements or at the service needs of the population (Director of Planning, Northern DHA, emphasis added).
Finance is the main item on the DMB agenda; it seems to have totally paralysed planning (GP member of DMB, Northern DHA).
The pressures were just as clear elsewhere in the organisation:
As far as I can see, management’s agenda is completely dominated by coping with financial restrictions, even to the point where it has perverse results. When beds were closed with the intention of saving money, the throughput of patients actually went up and very little was saved. But the nurses were frantic and the quality of care fell (Consultant Anaesthetist, Northern DHA).
When they chop you, you are penalised for your earlier savings (Patient Services Manager, Northern DHA).
My Unit is a constant source of funds to support the rest of the District. For instance, the RHA provided [money] to upgrade [psychiatric] wards but a lot of it actually went to support overspending in the Acute Unit (UGM, London DHA).
Not surprisingly, such financial pressure pervaded other areas of decisionmaking:
Finance tends to preoccupy [us] and influences everything else, such as development or changes in organisation structure (District Works Officer, Northern DHA).
In fact, the Northern DHA had begun to adopt what might be termed a more proactive reaction to the finance problem; that is, it sought to design a system for reacting to financial exigencies. This consisted of a rough formula matching funds to staffing levels to beds to patient throughput. If funds were reduced, beds would be reduced in an attempt to keep throughput of patients in line with finance; this of course depended upon medical cooperation which, as suggested in one of the above quotations, was not always forthcoming. Indeed this was the basis of the DGM’s aspiration (also referred to above) of developing planning agreements with groups of clinicians. In contrast to this essentially decentralist response to financial pressures, the London DHA had reacted by centralising decisions, sometimes apparently arbitrarily:
Decisions are made behind your back and you are told afterwards (Senior Nurse Manager, London DHA).
We are not allowed to manage…. Sisters who I am responsible for see me wasting my time making decisions which are then overruled by others (Outpatient Department Manager, London DHA).
The DMB agenda often contains quite detailed issues, such as pottering services (GP Member of DMB, London DHA).
The London DHA had, in addition, an even less tractable service problem than Northern DHA. Partly as a consequence of the socio-economic and demographic characteristics of its catchment population, the Authority’s general hospital experienced an extremely high proportion of immediate admissions, either through the Accident and Emergency Department, or through direct GP approaches to the relevant specialist ‘firm’. This created both problems in controlling patient throughput and in ensuring that scheduled elective cases were dealt with; there was a high level of cancellation of the latter. The vicious spiral was continued by GPs’ learning to ‘beat the system’ by advising patients to attend the Accident Department, or by seeking to have them admitted as urgent cases. There was little interest by doctors or middle managers in tackling this problem (though it was widely recognised), and indeed little idea on the part of senior managers how to set about breaking the cycle:
Management is not interested in proactive bed management (Consultant Surgeon, London DHA).
Doctors aren’t interested in managing their beds (Senior Nurse Manager, London DHA).
[The managers] just come round with their clipboards when we’re short of beds (Ward Sister, London DHA).
In both districts, financial problems and the consequent difficulty in service planning extended into the relationship between acute (in the broad sense) services and other services, such as mental illness, mental handicap, the elderly, and community services. Quite simply, acute inpatient services and their costs dominated district-level decisionmaking. As a result, there were few attempts at integration of services, either between units, between hospital and community services, or between NHS and local government Authority services:
The existence of a community unit fragments the service [for the elderly]: a voice crying in the wilderness in both places (Consultant Geriatrician, London DHA).
The DHA managers deeply resent the local [government] authority’s lead responsibility for mental handicap they regard the commitment of joint finance [to it] as hi-jacking NHS money (CHC Secretary, London district).
My colleagues take almost no interest in the running of the hospital (GP, London district).
The [mental handicap] service was good and progressive at one time. Visitors came from other parts of the country to see it. It’s still not bad but initiatives have been lost because of the lack of influence of community services in planning (UGM, Northern DHA).
The weakness of community and mental handicap services is the other side of the coin [of concentration of acute services] (Director of Planning, Northern DHA).
I’m completely forgotten and abandoned by the District; they’re only interested in hospitals, not in family or socially based care (Consultant in Community Psychiatry, London DHA).
Although (as elsewhere in the NHS) both Districts had slowly improving information systems and, as noted in Chapter 1 above, both were amongst the pioneers of providing budgetary information to doctors, there was little evidence of a proactive approach to the resulting information. Performance indicators (Pis), for instance, were essentially something imposed upon districts by the RHA:
We see the RHA as arbitrary and directive, but not helpfully so. It’s the Russian bear to us we have to use Pis in internal discussions because the RHA has concentrated on a few supposedly key ones. The review process hasn’t impinged on clinicians at all (Consultant DMB Member, Northern DHA).
[The regional] review process and Pis reflect flavours of the month [ideally] health authorities should devise their own indicators for comparison over time, not with anyone else (Director of Personnel, London DHA).
The financial information provided by both districts to decentralised groups of clinicians did not amount to formal budgetholding on the part of the latter. But there was no evidence that this information was used by clinicians:
Having more information is becoming a panacea for doing anything else [sic] doctors will only take notice of what things cost when the money comes from their own pockets (Consultant Pathologist, London DHA).
[Budgetary information] is still provided, but we don’t use it. We note and nod, and then I throw [the printouts] in that pile in the corner [of my office] (Consultant Physician, Northern DHA).
The existence of this type of information, combined with the general recognition of the financial climate, did however contribute to the tendency, already noted, for many clinicians to modify their behaviour simply because they were aware of managers’ possession of it:
Doctors often don’t know very much. When facts leave them nowhere to run, they won’t embarrass themselves (UGM, London DHA).
[Budgetary information] has really changed doctors’ attitudes towards management clinicians are much more willing to identify rising costs in advance and to tell us about them (Director of Finance, Northern DHA).
A topic on which a large proportion of medical respondents volunteered strong views (though there was a small dissenting minority) was the perceived lack of impact of general management on hospital support services; medical records, laundry and linen services, portering, maintenance, and secretaries were variously cited as areas where longstanding problems of poor organisation and standards had been left untackled:
Medical records is particularly bad and no-one seems to care. At my previous hospital, it was a matter of pride if notes went missing, but not here. We [consultants] wanted to change the format of the front page of the records and it’s been impossible to find a manager who would take responsibility for this (Consultant Surgeon, London DHA).
However, examples of conscious attempts to introduce a more proactive approach to specific management topics did exist; these included budgets for equipment replacement in Northern DHA, and an attempt to manage news media relationships in London DHA. The District Medical Officer of the latter was working on a district health profile containing, inter alia, care targets for particular population groups, together with the contribution from NHS and other agencies which would be required for the achievement of these; ‘applied community medicine’ as he termed it. But other senior respondents in the district considered this to be
cloud cuckoo land (Director of Finance, London DHA).
Despite the generally reactive style of management which respondents described, the main symbol of the opposite approach, Individual Performance Review (IPR) remained popular with most managers (though Performance Related Pay was much less so). It should be said, however, that only one respondent volunteered the topic, and others had to be asked:
It’s good to have objectives, I think. Those who worry are those who have difficulty in achieving things (Acting Senior Nurse, Northern DHA).
Everybody likes to know what’s expected of them, and in the past it’s been too easy to avoid responsibility (Senior Nurse, London DHA).
A very few took the opposite view:
IPR objectives are often bullshit. Managers have to follow where doctors collectively go (Medically qualified UGM, London DHA).
The evidence from the present study leans towards the latter view. More precisely, many of managers’ IPR objectives (almost invariably kept close to hand in a desk drawer) were difficult to correlate with their oral accounts of personal work agendas. The IPR documents thus seemed more important symbolically than substantively. One prominent topic which usually appeared in IPR documents but remained conspicuously absent from accounts of activity was the broad area of ‘quality’ or evaluation of care and services. It was as if a tacit conspiracy existed to recognise that such matters were important but difficult and importune and so postponed in terms of action until some unspecified future. Moreover, even in respect of the dominant financial agenda, at least one respondent could discern a mixed message:
My first and key [IPR] objective is to manage the district ‘within the funds available’. But there’s an ambiguity even here; the more the districts in the Region overspend, the more the RHA can support its case for more funding (DGH, London DHA).
It was also difficult to correlate the ‘quality’ aspects of managers’ IPR objectives with accounts of organisational life provided by clinicians and junior and middle managers. The topic of quality is further discussed in the next-but-one subsection.
The focus of managerial agendas
The pre-Griffiths research, it will be recalled, provided a picture of managerial agendas dominated by responses to groups of NHS workers, especially professionals and trade unions, rather than by responses to natients, relatives, or the community. The present study suggests that a major change has taken place since Griffiths, though it may not be correct to attribute it to Griffiths. (The counterfactual problem is dealt with in the penultimate section of this chapter.) Managerial agendas since Griffiths have become driven from outside the organisation, though not by service users or the public. It is already clear from the preceding subsection that this external drive was largely political and financial in character, transmitted from government to RHA to DHA:
We see the Regional General Manager as a tool of the DHSS (Director of Planning, Northern DHA).
In the review process, concerns about overspending are the dominant message from Region. Patients never seem to appear in it (Consultant DMB member, London DHA).
It’s frustrating that cutbacks masquerade as efficiency savings. I feel sorry for the UGMs having to dress things up (Consultant Physician and DHA member, London DHA).
A patient is the last person that managers can think about my ward was temporarily closed to save money and the nurses felt so guilty and aimless that they had to be counselled by the hospital chaplain (Ward Sister, Northern DHA).
Our unit managers can’t worry about patients. All they can do is balance the books (Consultant Surgeon, London DHA).
Financial pressures also had the effect of sharpening inter-district competition for funds, with reported results that were not necessarily in the population’s interest:
They’re building new [sub-regional specialty] beds in [neighbouring district] when we’ve got empty ones which could be used …the waiting list money went to the inefficient districts. We could have treated more patients for the same money that went to [neighbouring district] (DHA Chairman, Northern DHA).
(The district had, however, been relatively successful, in a recent bid to the RHA for ‘windfall’ funds.)
It followed from these pressures that patient or population-related matters rarely appeared on the agendas of DMB meetings or on the personal agendas of managers:
We don’t take notice of what the community wants (GP member of DMB, Northern DHA).
Patients? Not really. There are too many problems for managers and DHAs to think about them (Director of Finance, Northern DHA).
The DMB has spent the whole of the first three years trying to make cuts; everything else has been secondary. It’s always bloody money on the agenda. I see my role and [consultant member of DMB] as preventing savings at the expense of patient services (GP member of DMB, London DHA).
Consumer interests aren’t to the fore. It’s bolt-on. There’s a gooddeal of tokenism (Director of Personnel, London DHA).
In such an environment it seems hardly surprising that no shift had been seen to occur in the relative influence of CHCs:
The NHS is so insensitive. I have to counsel disappointed complainants (CHC Secretary, Northern district).
Nothing has changed. The CHC is a still, small voice (District Physiotherapist, Northern DHA).
[The DHA chairman] loathes CHCs and has refused to consult us on any issue until plans are so far advanced that change is impossible. He also tried [unsuccessfully] to exclude the CHC from joint planning. The officers consider consumerism to be an impediment to getting things done (CHC Secretary, London district).
The formal consultation process is the biggest single block to the progress of general management. I’m not opposed to consultation -any good manager should do it – but we shouldn’t need ministerial approval for closures and major changes. If we are not to be trusted, we shouldn’t have been appointed (DGM, London DHA).
Just one (consultant) respondent took the opposite view; the CHC was over-ready to encourage complaints. In that district, however, there was little evidence that patient complaints were receiving closer attention than before Griffiths:
The consultant never has to answer the person who complains. It’s always the junior doctor or nurse who has to answer the questions. Managers won’t come and see a patient who complains (Ward Sister, London DHA).
In the other district, nurse managers were planning to help relatives complain to the CHC where they wished to do so. The reasoning was that complaints might be explicable in terms of nursing staff shortages, and thereby provide ammunition for additional resource requests.
Both districts had commenced patient-related initiatives of various kinds. In one, each psychiatric ward had established a relatives’ group to be consulted from time to time. In the other district, an internal campaign had been mounted with the intention of encouraging staff to treat patients more politely. This was extensively cited by respondents, though only one went on to comment upon its value:
Things have improved slightly, though they look better on paper than in reality consumerism is only talked about, not practised. No patient would notice a difference in things since Griffiths (Outpatient Manager, London DHA).
To summarise so far: it is clear that NHS management post-Griffiths was by no means as producer-oriented as it had been before. It will be noted that no mention of trade union influence has been made; in contrast to their prominent role for pre-Griffiths managers, they were simply not seen as a problem. Doctors, as was shown in an earlier subsection, were still problematic from a management point of view, but had been substantially displaced on the management agenda by externally imposed financial considerations. Despite the consumerist language of Griffiths, the NHS had become less producer-oriented but no more consumer-oriented than before.
Management and evaluation
The preceding section contained some evidence about consumer views: one way in which health services can be evaluated. It has been seen, however, that the dominance of finance on senior management agendas left little space for other considerations. In Northern DHA, a patient satisfaction survey had been conducted about a year prior to the fieldwork for the present study. What was striking was that whilst a large proportion of respondents were aware of this survey, only one person outside senior management seemed to be aware of its results:
The main lesson was that we [consultants] needed to spend more tune with individual patients, explaining diagnosis and prognosis Unfortunately, most of my colleagues have not seen the survey result as a home truth and have been able to defend themselves by finding grounds on which to criticise the data (Consultant Surgeon, Northern DHA).
This particular consultant had, as a result of the survey, been provided with funds to employ a counsellor in his breast clinic. Otherwise, there was no reported effect; indeed the patient services officer had been compelled to wind up a working group on service quality, for lack of support from either his superiors or clinicians.
Patient satisfaction is, of course, by no means the only measure by which health services can be evaluated, nor surveys the only mechanism for evaluation. In fact, various other evaluation efforts were underway in both districts. Some of these were stimulated by Regional interest in the topic. In Northern DHA, one senior nurse was a member of an RHA working group on standards of care for the elderly; at the time of the fieldwork, this group was in the process of investigating available conceptual tools for measuring and assessing care, and had not formulated any recommendations. The London DHA was participating in a regional scheme of microcomputer based surgical audit, though the RHA officer in charge was not convinced of the commitment of those taking part. One respondent seemed keen enough, though ambivalent about how far the process of audit of professional work should be distanced from management:
I was amongst those who pressed for [surgical audit] system to be introduced in the region. Then, I will accept that managers have the right to ask me questions. The Royal College of Surgeons is making death and complications meetings a compulsory condition [sic] for the recognition of training posts and I fully accept the logic of peer review. But all this is nothing to do with Griffiths. With this information, epidemiological predictions could be used to decide on what medical facilities are necessary and how much money would be needed. Diagnostic and treatment protocols would then be justified (Consultant Surgeon, London DHA).
The above quotation also draws attention to a source of external pressure for evaluation other than the RHA: the professional associations. Thus, the Royal Colleges of Surgeons and Physicians, the Association of Anaesthetists and the Chartered Society of Physiotherapy were all cited by respondents as beginning to demand a more critically evaluative approach to care, and in particular an approach based on outcomes (Donabedian 1980). In addition, several of the medical professional associations had recently collaborated in a confidential enquiry into perioperative death (Buck et al, 1987) which had been widely reported and was known to many respondents.
There were locally determined developments too. In Northern DHA the ‘Monitor’ and ‘Criteria for Care’ nursing quality systems were in the process of being introduced in four wards (for an outline of these systems, see Goldstone et al, 1983). In London DHA a scheme of evaluation of nursing care, using the occurrence of pressure sores as a proxy for poor standards, had been devised. A pharmacy information system had also been introduced to disseminate prescribing costs; medical respondents reported that they found the information derived from this to be credible and reported its use in their clinical practice.
Although these initiatives represent fragmented efforts from a variety of players, with no apparent conceptual or organisational cohesion, it can nevertheless be said that a marked change had taken place since Griffiths, though no respondent attributed it to general management. Quality of care as something other than a function of the level of resource inputs had entered the vocabulary of virtually all respondents to the present study. Not all developments were in this direction, however; for instance, several respondents drew attention to the decreased inclination of surgeons to ask for post mortem examinations:
In the [United] States, the pathologist is the hospital’s auditor. Logically, this ought to be more important in any competitive system (Consultant Pathologist, London DHA).
Ironically, the Northern District was the workplace of a medical consultant well-known nationally for his work in medical audit; in his own district, his ideas carried no discernable weight. Both managers and clinical colleagues regarded him as an outsider:
He might as well not be here at all when he is, he causes trouble by not working through the [Cogwheel] divisions (Consultant Physician, Northern DHA).
At the beginning of the fieldwork for the present study, the London DHA’s DMB were planning to discuss quality for the first time; until then, according to one consultant sympathetic to management:
Quality? Only the single issue of the waiting list. If they were interested in quality, they’d make a lot of trouble for themselves, because it isn’t easy either to define or achieve (Consultant Psychiatrist, London DHA).
And indeed, the meeting was not a success. It was described thus by one of those present;
A regional expert came and talked a lot of guff [about quality] (GP member of DMB, London).
By the conclusion of the fieldwork, the DGM had come to take the view that management had failed to get quality taken seriously; there were even doubts about the surgical audit. DMB members promised that quality would be the following year’s main agenda item.
Unsurprisingly, in view of the importance of the financial situation of both health authorities, one theme related to evaluation (though not to quality) was emphasised by a large number of respondents to the present study: increased cost consciousness:
People are now far more aware of costs and the need to control them (District Works Officer, Northern DHA).
People are beginning to think about how much everything costs (Unit Director of Nursing, London DHA).
Financial restrictions have provoked us to think about whether cheaper dressings can be used, and there’s a general feeling of cost consciousness on the Ward (Ward Sister, Northern DHA).
The role of financial constraints in the public services in bringing about the Griffiths changes in the NHS is discussed in Chapter 5. What is clear at this point, however, is that Griffiths did not bring about the financial constraints in the NHS. The counterfactual question therefore arises; is the general level of cost consciousness observed in the present study one of the effects of Griffiths, or would it have occurred anyway? The latter was the view adopted by the ‘counterfactual panel’ (see Chapter 1) established for the present study, though it was also volunteered by several respondents:
The NHS has become progressively oriented towards [resource] management, but financial constraints have more to do with this than had Griffiths (Consultant Surgeon, Northern DHA).
[Cost-consciousness] is more due to the economic climate than to general management (Senior Nurse Manager, London DHA).
Summary and comparisons
If, as argued in the opening section of this chapter the key element in the character of pre-Griffiths ‘diplomatic’ management was its relative lack of influence in relation to doctors, then the key finding of this part of the present study is that only very modest changes in this relationship have taken place as a result of the introduction of general management. Specifically, managers pressed by an external financial agenda have been relatively enabled to make facility and service reductions. In addition, doctors’ awareness of these financial pressures, coupled with developments in management information, have made them more inclined to police their own activities against ‘creeping developments’.
The pressures of this external agenda upon managers have also helped to modify the producer orientation of their administrative and professional predecessors, though without replacing it with a consumer orientation. This external agenda has also helped to perpetuate a generally reactive orientation in management, though the problems faced are, of course, different. The financial pressures have also made for a generally enhanced level of cost consciousness than before, but broader concerns with evaluation and ‘quality’ in health care, denied space on the managerial agenda, have remained muted, fragmented and sometimes rhetorical.
Whilst general managers, assisted by unprecedented discretion over organisational structures, have secured enhanced influence over non-doctors, so far as doctors are concerned they remained ‘diplomats’. The principal for whom these diplomats act is, post Griffiths, different however. Having previously been, in effect, agents of the medical profession, managers became agents of government. Yet despite all this, and despite the subsequent acid comment of (by then) Sir Roy Griffiths that
Whilst my name at the time was primarily connected with general management, I personally took this as shorthand for the introduction of an effective management process. I did not intend that the result should be yet another profession in the National Health Service (Griffiths, 1992, p. 65),
the existence of general managers seemed both legitimate and welcome to respondents; no-one wished to see a return to consensus team management.
In making comparisons of data from the present study, two possibilities arise: comparisons between the two districts studied, and comparisons with other, contemporary, studies. On the first dimension (and bearing in mind the considerable contextual similarities between the two districts: see Chapter 1), there were few differences. This is of some interest since, in conventional terms, the Northern DHA showed every sign of being better organised that its London counterpart. The former had experienced greater stability of managerial personnel, exhibited a more unitary management style, and had managed to create a situation where respondents to the present study were aware of the research and its objectives and arrived at the appointed time and place of interview.
By contrast, the London DHA had had a rapid turnover of managers, exhibited a conflictual atmosphere in which respondents were very ready to criticise each other, and often failed to communicate the purpose or logistics of the present study. Yet, and this is the crucial point, it cannot be said that (with the single exception of Northern DHA’s attempt at more proactive caseload management described in the preceding section) there were substantive differences in terms of the impact of the Griffiths changes on the two.
Turning to comparisons with other studies, it must be cautioned that the great variety in scale, focus, and level employed in the two dozen or so empirical research projects conducted in the aftermath of Griffiths (for a comprehensive listing, see Harrison et al, 1992, pp. 75-7) makes firm conclusions difficult. Nevertheless, these studies do at least exhibit agreement on the salient points emerging from the above account of Londonand Northern DHAs, suggesting that generalisation is not unwarranted.
The relative weakness of general managers in the face of consultants was observed in Pindar’s (1986) interview study of general managers, and in Harrison et al’s, (1992) study of nine districts in addition to the present study. It is summarised graphically, along with the bureaucratic role of DHSS and RHAs, in Strong and Robinson’s ethnographic account:
Local initiative was frustrated by ministers, by civil servants, by supervisory management tiers, and by powerful professional bodies. Doctors still gave orders, nanny still knew best (Strong and Robinson, 1990, p. 164).
The generally perceived legitimacy of the institution was noted in studies by Harrison and Schulz (1988), Banyard (1988), Flynn (1988) and Williamson (1990). The reactive character of management in the face of Departmental and Regional pressure is evident from studies by Bardsley et al (1987), Owens and Glennerster (1990), whilst Williamson (1990, p. 7) failed to find any evidence that general managers’ self-descriptions in terms such as ‘directive’, or ‘inspirational’ bore any resemblance to their activities. The cosmetic nature of approaches to service quality was noted by Strong and Robinson (1990, p. 182), and the pervasive effect of financial pressures by Flynn (1988; 1992).
At this general level of analysis, only one piece of contemporary research seems to question any of the above key findings. Generalising from their extensive work on sixteen NHS case studies, Pettigrew et al comment that:
Historically, health care organisations have been seen as highly change-resistant in part because of the highly political nature of health care delivery, in part because of the numerous professional tribes, and in part because of the special veto power of clinicians. It is now worth questioning whether this is increasingly a dated view (Pettigrew, Ferlie and McKee, 1992a, p. 27).
(For accounts of these case studies, see Pettigrew et al, 1989a; 1989b; 1992b; McKee and Pettigrew, 1988; 1989; Ferlie and Pettigrew, 1988). Two of these case studies seem to particularly important sources for this alternative view of medical/managerial relationships.
One of these concerns the closure of a large psychiatric hospital, in which medical-managerial conflict arose from the fact that each group claimed for itself the pioneering role in developing community care for the mentally ill, and thereby ultimately allowing closure of the hospital:
The consultant psychiatrists interviewed in the present study felt that their initial pioneering role as a profession in introducing care in the community was being denied and denigrated by the local general managers …
They found it ironic to be perceived by managers as laggards and resistant to community schemes.
….the role of social and medical change [was] endorsed while managerial direction [was] dismissed. When managers were asked from where they saw the pressure to provide care in the community services stemming (and congruently the hospital closure), they were much more likely to tie it to policy imperatives and to managerial action such as the review process than to clinical or scientific advances.
The common view of a number of managers interviewed here was that the clinicians’ part in the service change ranged from, at best, passive to, at worst, obstructive (McKee, 1988, pp. 311-2).
Since this is a conflict of interpretation over the origins and rationale for change, rather than over its substance and does not provide any resolution, it cannot offer much evidence about the substantive influence of the parties. The second case study concerns the response of Parkside DHA in north London to spread of AIDS. The study concludes that the DGM’s intervention was crucial in the production of a community-based, rather than inpatient-based strategy for the provision of AIDS services:
The financial question arose when it became clear that the 1987/88 special allocation was only going to be £1.25 million as opposed to the £3 million asked for. This was a major gap, given rising expectations, and difficult to respond to. The first meeting of the Aids Executive Committee [which included consultants] determined -despite the new strategy – that the first priority should be to protect extra beds, even if this meant that community care or health education developments could not be funded. Some members of the Aids EC were convinced that the hospital (on a shared care crisis) still had a major role to play:
AZT, the whole range of treatment now, points to the next decade meaning more and more hospital admissions, not less and less. It points to a whole range of resources, the more successful we become at treating these patients, the more resources we will have to use inside the hospital as well as out.
It was at this point that the DGM firmly moved to bounce the bid back for revision:
When we saw the paper that came and divvied up the cash, it seemed to say mega beds, home care team firmly controlled by the hospital end, and if there is anything else left, we just might manage to get the odd bit of community care, but it might get eaten up.
Whereas the acute sector strategy which the district had developed in the 1970s could be seen in Day and Klein’s [1983] terms as mobilising consent from a complex array of different interest groups, implementation of the Aids strategy depended in part on the exercise of managerial power. As the DGM put it:
I suppose my role is really to make sure that the thing is on the road. The major intervention that I made was at the management group meeting which looked at the funding for this year, where everyone sat around like a lot of lemons, and I kept on saying ‘no’. Otherwise we would have ended up with more and more beds. (Text and quotations from Ferlie and Pettigrew, 1990, p. 211.)
There are obvious limitations in what one might expect to conclude from a single case study (hence the comparison of the present study with the work of others), but it is in any case not necessary to see Ferlie and Pettigrew’s conclusion as deviant from other work. The DGM’s influence was partly enabled by financial restrictions, and was, in addition, supported by other clinicians:
Managerial intervention chimed with the wish of many clinicians and the finance function to contain the AIDS workload (Ferlie and Pettigrew, 1990, p. 212).
Thus important elements of the work of Pettigrew et al, are not so incompatible with those of the present study. At root, however, it may be that different kinds of case study must be expected to produce different results. Thus, Pettigrew et al’s work was based on particular issues in particular locations, whereas the present study, whilst concerned with particular locations, attempts to assemble a more general picture of medical/managerial relationships.
