Presentation at our seminar New deal for patient and public involvement
Alyson Morley Policy Adviser Democratic Health Network 13th January 2007
What’s in the Bill?
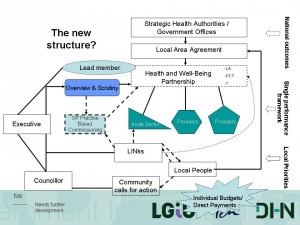
Where do LINks fit in?
The role of local authorities
Challenges and opportunities
What now?
Local Government And Public Involvement In Health Bill
LINks – Remit corresponds to PCT boundaries
Greater focus on commissioning
Remit extended to social care
Loose network – “open to all” individuals and organisations
Structure and accountability to be locally determined
How will LINks be resourced?
Local authorities funded to procure a host organisation to set up LINks
Money will not be ringfenced
Host organisations may be existing FSOs
No guidance on how members will be recruited, inducted or supported
Powers and responsibities of LINks
Contribute to the shape and quality of health provision
Focus on commissioning
Comment on service reconfigurations
Close working relationship with overview and scrutiny
Power to inspect NHS premises but not private and independent providers
Other provisions in the Bill
A duty for “partner authorities” including PCTs to agree Local Area Agreements
Community calls for action – a right for all councillors to act on community concerns
Scrutiny of partner authorities’ action on LAA priorities
Section 242 – strengthening the duty to consult
Where do LINks fit in?
The role of health overview and scrutiny committees
Cooperation between PPIFs and OSCs has been patchy
Build on best practice to push improvements
LAs will receive funding to procure a “host organisation” for LINks
Much is to be locally determined
Challenges
Accountability – how do you ensure accountability to the community?
Resources – will they be adequate?
Geography – how will LINks operate in large geographical areas?
Capacity and expertise – will LINks have the expertise to influence commissioning?
Credibility – with the community and with NHS
Ensuring that no one interest group dominates
Relationship between LINks and NHS foundation trusts
Relationship with sub-regional services eg ambulance trusts
Turning rhetorical commitment to involvement into a reality
Commercial interests – what about organisations that are providers of services?
Opportunities
A wider range of people and organisations involved
Following the patient journey rather than focused on one institution
Influencing commissioning to make care more patient-centred
Building on best practice of PPIFs
Embedding PPI into business planning of health and social care
Influencing local area agreements
What now?
Learning from “early adopters”
Lobbying/influencing Health Committee, Parliament and DH on resources, national standards, model contracts, national and regional bodies
Building on current best practice from OSCs and PPIFs
Reminding DH of its commitment to update regularly
Draw up terms of reference, codes of conduct and protocols with OSCs