Notes on our Seminars:
Quaker Meeting House 10 St James Street, Sheffield, S1 2EW 27th May 2006
Toynbee Hall 28 Commercial Street, London E1 6LS Wednesday 21st June 2006

Barrett v United Health at Creswell

Patient Opinion: a new approach to public involvement
James Munro contribtion to conference
Who is Patient Opinion for?
- For patients
- to give feedback on their health services
- to easily see what others are saying
- For health care providers
- to hear – and respond to – patient concerns and thank-yous
- to compare their ratings with others
What is available now?
Patient Opinion is available across England but not (yet) the rest of the UK. It covers all acute trusts. Coming soon:
- Mental health and care trusts
- ISTCs
- Private sector hospitals
Feedback experience so far
- Around 50% of patient feedback positive
- Around 30% mixed
- Around 20% critical
- Usually in a thoughtful way
Feedback management
All opinions are reviewed before publication
- Editorial policy is public and evolving
- Critical opinions are flagged to subscribers
- Patient identity is confidential
- Anti-gaming safeguards are built in
How is Patient Opinion set up?
- A social enterprise
- A not-for-profit business
- Not a charity or a project
- Independent of the NHS
- But sharing NHS values
How is this funded?
- Through subscriptions to the service
- From providers, commissioners and the Healthcare Commission
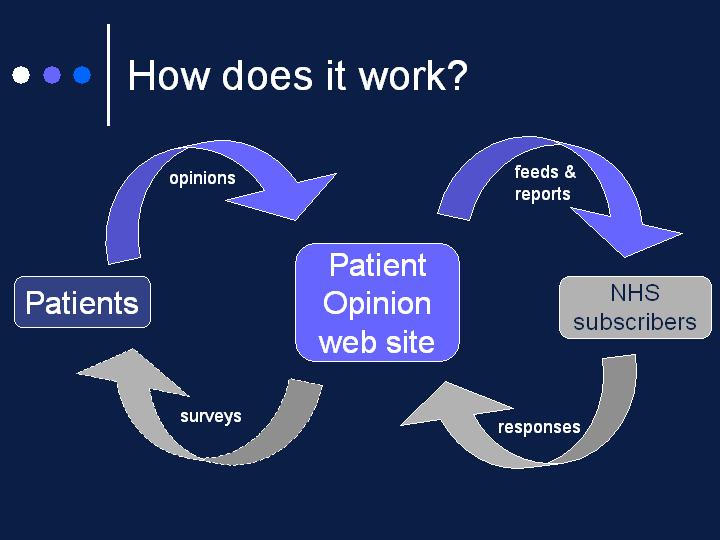
Subscribers receive
- Access to all Patient Opinion data through custom feeds and reports
- Ability to respond to patient feedback
Public use of Patient Opinion is free
How this fits with policy
- Patient Choice
- Patient-led NHS
- Complements PPI and PALS
- Healthcare Commission standards
- e-government
- Everyday democracy
Peter Johns, Board of Community Health Councils in Wales.
Community Health Councils In Wales
Health Wales Act 2003:
- Power to the welsh assembly to establish or abolish CHCs
- Change in membership proportions
- Access to primary care
- Establishment of a statutory welsh board of CHCs
Regulations Under The Act
- Came into force in april 2004
- Maintain previous powers and rights
- Add rights of access to primary care, nursing homes and private hospitals
- Power to monitor ppi activity of local health boards and trusts
The Board
- Consists of reps of all 26 CHCs and 2 staff reps.
- Non-voting reps from WAG and Powys LHB as well as WCVA
- Board`s powers include financial allocation and control and performance management of CHCs
Progress To Date
- All Wales corporate identity
- Performance review of all CHCs now in place
- New job descriptions and re-evaluation of all jobs in 2004
- Fully funded complaints advocates available across Wales
- Hospital patient environment work with nhs wales for last three years
- Protocols for primary care work and nursing homes
- All-Wales standard visiting format for hospital visits
- Enhanced role within NHS Wales
- Evidence to assembly health committee
- Annual report to the minister
- Improvements in funding
- Collaboration with NHS confederation
Where Next?
- Bringing all CHCs up to the same standard
- Ensure that the NHSchanges in Wales reflect patients` needs
- Keep in touch with other parts of UK
- Increase public awareness of Community Health Councils
- Changes in way members are appointed?
- Redistribution of funding?
- National focus on patient issues
- Improve profile in media
- Keep doing it for patients!!

Jill Knight, Chair Scarborough Whitby and Ryedale PPI Forum
A successful Patients’ Forum
Started ‘running’ with 300 patient long dentist queues and local people reported as extracting their own teeth
Successes Helped by Advantages of
- Public increasingly involved
- Keen members having a broad variety of backgrounds with a range of experience and skills
- Members prepared to travel and do more hours than Commission prepared them for
- A PCT committed to its PPI role
Sucessess:
- Lots of people attended meetings on Out of Hours service, Community Hospitals and Dentistry.
- Hope for same at next week’s meeting on health and transport
Early Successes
Forum was actively engaged in the PCT getting
- more NHS dentists
- an efficient Out of Hours service
- an active ‘Esk Valley’ public engagement, inviting a third of the PCT area to comment on their services
- podiatry to the remote Esk Valley area
- an exceptional treatment policy
- clarity on local cancer treatment
- lay visits to every local GP practices and a good and growing relationship with practices
New Successes
- Forum now actively engaged inMulti agency work in Whitby with many agencies ‘involved’ in health: GPs, health visitors, Sure Start, voluntary sector and Town, District & County Councils
- Multi agency work (health sector, councils and police) involved in domestic abuse
- Multi agency work with transport and access groups
What Future?
- Members currently inundated with letters and attending numerous meetings on the future of PPI
- Near future is a Forum covering a new PCT four times as big- over 100 miles wide
- THEN a network over the same vast area?

National Association for Patient Participation

Dr Brian Fisher, Lewisham PCT, Patient and Public Involvement Lead, NHS Alliance.
PPI OUTSIDE HOSPITAL – Listen Respect and Respond
Community-based Commissioning: PPI and the new way of doing business in the NHS
Presentation by Dr Brian Fisher, PPI Lead for the NHS Alliance 21st June 2006
Community-based Commissioning:
- What users want
- What NHSA recommends – process to PPI
- Payment by Results and Practice Based Commissioning
- PPI+PBC
- Community Development may be the key
What patients want the structure to look like (MORI)
- Representative
- But also local
- Independent
- Accessible
- a wider range of people to be involved
- Accountable
- Change needs to happen as a result of PPI
- Democratic process
What do the public want to influence? (MORI)
- The development of new services
- The improvement of existing services
- The monitoring of quality
- The minimising of waste
Start with processes not structures
Developing a continuous process that:
- Creates engagement without exhaustion for clinicians, the public and patients. Brief liaisons are OK,
- Is flexible, drawing in a range of people in different ways and in different places
- Challenges but can also cooperate with the establishment
- Obtains rich ideas and recommendations
- Gets changes made
Support the system to change
- HCC with clear developmental standards
- PPI takes up a large proportion of the points
- Democratic/accountable processes at all levels:
- PBC
- Practices
- Foundation style involvement at PCTs and practices
Suggestions from the floor, please: how do we get monolithic organisations to become responsive?
Payment by results
- Money follows the patient
- More patients, more money
- National tariff, so no ability to attract referrals through price
- The idea is to attract through:
- Quality, speed
- Better relationships with PBC groups
Payment by results
- If over tariff, the hospital will lose
- Gaming
- Less than 24h admissions
- 24-47h admissions
- Shut services if you can’t compete
- Alternative suppliers of care
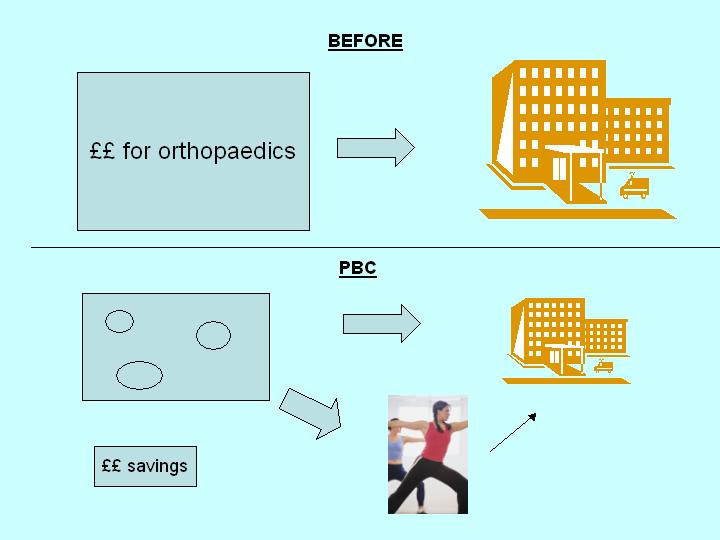
PBC+PPI
- Involve local people in:
- PBC cluster priorities
- Improving pathways
- Spending savings
- Monitoring quality
- PPI services should support clinicians
- Not confrontational
- Facilitating patient panels and PPGs
- Helping practices respond to wider determinants of health
- Using existing PCT techniques and agencies such as PALS. Expert patients are key here.
A SURVEY OF PCTs (NHSA)
- 172 / 299 responses: already active practice based commissioning in their areas.
- 70% PCTs say that PPI can have a positive impact on PBC and that they have good mechanisms for engaging with local people.
- 71% of PCTs who already have active PBC say there is little or no public and patient involvement involved.
WHAT WE WANT IS: ENGAGEMENT WITHOUT EXHAUSTION
One approach which is beginning to work well:
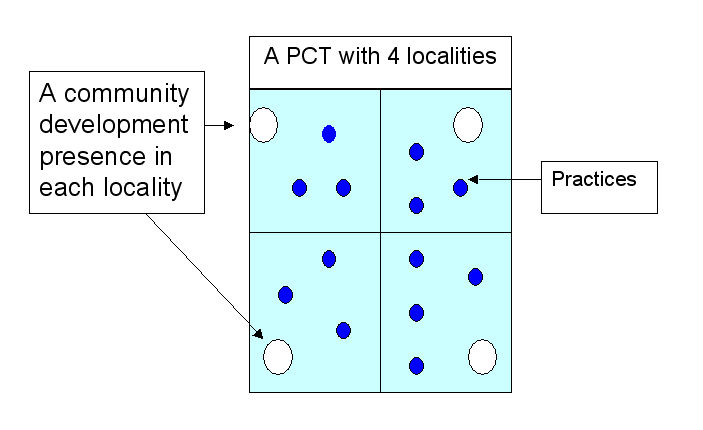
Community Development is the key
- A process that mobilises communities to become participants in both defining problems and developing solutions to health and health service issues, and that reaches out to those most likely to be excluded.
- Works with individuals and communities
- It promotes health by bringing people together in social networks
- Outreach flexibility
- Its raison d’etre is to get local voices heard and to support change
- Interdisciplinary because it listens to what local people say – links regeneration and health
- Light on practices, public and patients
Funding diversity reflects integration
- Community development approaches are already adopted by ODPM and the Home Office (Together We Can). Health needs to learn from them.
- Fund the CD workers from these diverse sources, spreading the load and increasing integration.
- Health Trainers ? Graduate MH workers offer another route
2 MODELS OF PPI FOR PBC CURRENTLY BEING USED IN THE BOROUGH OF LEWISHAM
- 4 PBC Groups in Lewisham – LCDP linked with each one
- Exploring change in the delivery of Diabetic services
- Starting in the most culturally diverse part of the borough
- Have developed a range of questions to explore in focus groups and with individual patients
- Following consultation will set up self help groups
- Positive impact on visits to A & E by these patients
LCDP has created a new model for patient involvement:
A PATIENT PANEL
- Inclusive and can capture views of the patients most difficult to reach
- A panel is being developed for the whole of a PBC area
- Very simple method of obtaining a lot of PPI quickly and cheaply

David Gilbert, Patient and Public Involvement Resource Centre
The New NHS Resource Centre for Patient and Public Involvement
Background to the Problem
- Long history of PPI
- Established in legislation – Health and Social Care Act 2001
- PPI led improvements are patchy
- PPI needs to be mainstreamed
- Build on good work being done
- PPI work needs to fit a new NHS
The new PPI Resource Centre
We are a consortium
- University of Warwick
- LMCA an alliance for health
- Centre for Public Scrutiny
Complementary responsibilities:
- Jonathan Tritter – Executive Director & Research Lead
- David Gilbert – Leads on Organisational Development
- Jill Brunt – In charge of Learning and Support
- Ian Brittain – Director of Communications
- Jane Martin – Facilitates Patient-Citizen Exchange
- David Pink – Facilitates the Health Voluntary Sector Network
- Sandy Sparks – Operations Manager
The new PPI Resource Centre
- Promote the value of patient and public involvement
- Create a one stop shop for information and advice
- Build capacity of organisations, staff and patient-citizens
- Develop and disseminate practical resources
- Generate evidence-based models & best practice examples
- Identify and maximise learning opportunities
- Develop networks and communities of interest
- Practice what we preach
If you have responsibility for PPI we will…
- Be your signpost to learning opportunities
- Put you in touch with people who can help
- Provide good practice examples
- Identify practical tools for your work
- Undertake research on key issues
- Keep you up to date on the PPI world
- Hold learning events and seminars
The Importance of Stakeholders
- Generating the concept of the Centre
- Bid to tender based on extensive consultation
- Our response as a consortium
- Vision shaped by work with over 40 organisations
- Need for continued collaboration
Work Domains
- Organisational Development
- Working with NHS Organisations to build PPI Systems
- Meeting Core Standard 17
- Learning and Support
- Identifying and responding to needs
- Curriculum development
- Identification and accreditation of providers
- Research and Best Practice
- Gathering and generating evidence
- Methodological development
- Patient-Citizen Exchange
- The People Bank
The Research & Best Practice Domain
- Identifying and distilling evidence
- Documenting examples of good practice
- Drawing on what works best from around the world
- Identifying what we don’t know
- Filling the gaps in our knowledge
- Ensuring that what we know informs, training, practice, evaluation and development
- Promoting high quality PPI
- In every healthcare context
The Learning and Support Domain
- Ensuring organisations can access high quality learning
- Mapping learning needs
- Developing learning pathways for:
- Members of PPI Forums
- Citizen governors
- PPI Champions
- PPI Professionals
- Linking with:
- the Skills Escalator
- the Knowledge and Skills Framework
The Organisational Development Domain
- Working on the ground to develop PPI systems in healthcare organisations
- Embedding PPI in the local health economy
- Building on the best of local notable practice
- Creating an organisational climate for change
- Promoting active learning
- Building capacity in organisations at local, regional and national level
The People Bank
- Training and supporting Patient-Citizens and PPI champions to shape the agenda of the NCI
- Promoting co-production
- in organisational development work
- in learning and support
- in research and best practice
The Patient-Citizen Exchange
- Facilitating online networks
- Enabling patient and public voice
- Developing mutual understanding
- Promoting accessible and innovative communication and dissemination
- Reaching diverse and traditionally hard to reach audiences
- Ensuring an inclusive approach to governance and management
- We look forward to working with you

Jane Sully National Development Officer- Health Age Concern England
Involving Patients in Commissioning
Background:
- Community Health Councils
- Commission for Patient Involvement in Health
- PPI Forums
- New arrangements on the horizon
- Commissioning a patient led NHS
- Practice Based Commissioning
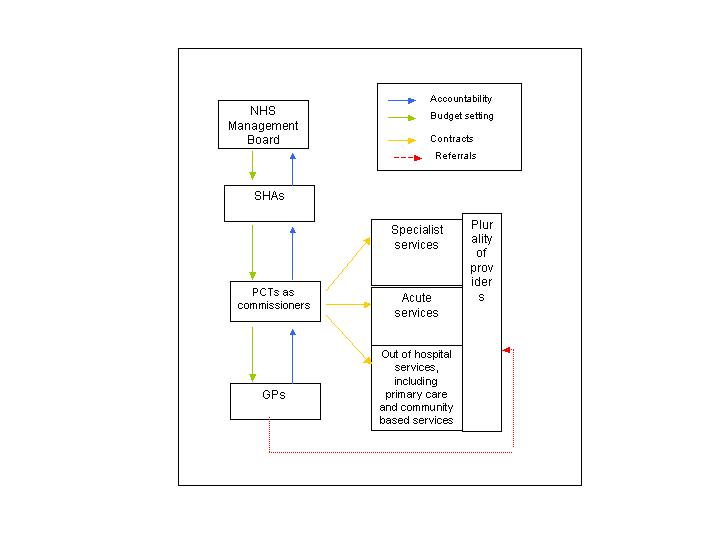
What Is Commissioning?
- No Common Definition
- Commissioning is the process of securing and managing appropriate healthcare services for relevant populations at value for money for taxpayers. In its purest form, it is composed of three phases:
- Understanding and segmenting the needs of local communities and individual patients and planning accordingly
- Defining services to meet these and contracting them from the most appropriate providers
- Monitoring provision and managing providers, to continuously improve outcomes for patients and local communities
Outcomes Of Effective Commissioning
The key outcomes of good commissioning might be summarised as:
- Improving health outcomes;
- Promoting a mix of services, in and out of hospital, that are appropriate to the scale and nature of the needs of the local community;
- Including patients, the public and all interested parties including, in particular, Local Authority partners, the voluntary sector and, when appropriate, the private sector;
- Providing services that comply with the core standards and are improving in line with the developmental standards;
- Offering value for money.
Why Involve Patients?
- Policy Developments around Patient Voice
- Healthcare Commission Ratings
- Practice Based Commissioning – service redesign/ demand management
- Learn from Patient experience
- Improved Self Care
- Monitoring Quality-continuous improvement
Approaches
- Not tokenistic consultation at the end of the process
- Choice is not Voice
- Target key groups
- Work through existing community structures
- Learn about your communities – not just statistics
- Location, Location, Location
How Do we Learn From the Experience of Ordinary People Like Me?
