Tom Smith, BMA Health policy and economic research unit, presentation at our conference Regulating Health and Social Care Professionals October 2006
A FEW HEADLINES ON THE DONALDSON REPORT
- Changing the burden of proof. Why no sliding scale?
- The airline analogy
- Affiliates
- Separating adjudication and investigation
- Separating diagnosis and treatment
- The tone of the report
A dictionary definition of professionalism ‘An occupation whose core element is work based upon the mastery of a complex body of knowledge and skills. It is a vocation in which knowledge of some department of science or learning or the practice of an art founded upon it is used in the service of others. Its members profess a commitment to competence, integrity and morality, altruism, and the promotion of the public good within their domain. These commitments form the basis of a social contract between a profession and society, which in return grants the profession the right to autonomy in practice and the privilege of self-regulation. Professions and their members are accountable to those serviced and to society’ – OED
Professionalism for everyone?
There has been a blurring of meaning. The term is applied to all occupations not particular roles. It is understood to mean, “good at your job”
A whole of range of management and self-development books have been published urging everyone to be professional, which is seen as an attitude to work.At the same time others are feeling more confident about applying this label to themselves, doctors seem less so. Why?
Profound changes in medical professionalism:
- Bristol
- Shipman
- Scandals over poor individual standards
The key characteristics of medical professionalism are coming under attack
Characteristics of professions
- A profession possesses a discrete body of knowledge and skills over which its members have exclusive control.
- Professional associations serve as the ultimate authorities on the affairs relating to their domains
- Within the constraints of the law, the professions control admission to practice and the terms, conditions, and goals of the practice itself
- The professions are responsible for the ethical and technical criteria by which their members are evaluated
- Individual members remain autonomous in their workplaces within the limits of rules and standards laid down by their associations and the legal structures within which they work
- It is expected that professionals will gain their livelihood by providing service to the public in the area of their expertise
- Members are expected to value performance above reward, and are held to higher standards of behaviour than are non-professionals
Sylvia R Cruess and Richard L Cruess. Professionalism must be taught BMJ, Dec 1997; 315: 1674 – 1677

What’s gone wrong with the traditional view of medical professionalism?
“It is because it doesn’t feel to me that the use of the word ‘professional’, in the sense of having consistently high standards of conduct as a class of people, is any longer very convincing. In the shifting meaning of words ‘professional’ now means little more than well-paid and exclusive.
Traditionally professionalism has been defined through the personal qualities of the person including their private moral conduct. And this idea that professionalism is a matter of personal qualities holds today. Qualities such as mastery, altruism and a commitment to do good, personal probity and integrity.
In the modern world I find a disturbing smugness and self-satisfaction about this kind of definition. I prefer Bernard Shaw’s definition in ‘A Doctor’s Dilemma’. ‘All professions are a conspiracy against the laity’”.
Harry Cayton – Some thoughts on medical professionalism and regulation
Some think that everything about professionalism has changed?
- Exclusive knowledge
- control over knowledge
- workplace autonomy
- influence over policy
“All of these attributes are now gone, except influence over public policy, which has diminished” – The then President of the Royal College of Physicians, Dame Carol Black speaking to the Joint Consultants Committee conference (8th October 2005)

“Administration is going to be the chief headache for years to come” – Nye Bevan
Five key dates in NHS reform ….two are before Labour came to power
- 1983 the introduction of general management
- 1990 the introduction of an internal market and dividing the purchaser and provider functions
- three are after…
- 1997 National guidelines, standards and a statutory requirement for managers to demonstrate systems for continuous quality improvement
- 2003 Patient choice, the return of an internal market and health policy concentrates more on incentives
- 2006 A brewing argument about the direction of reform

Current policy lacks a narrative – It doesn’t engage health professionals
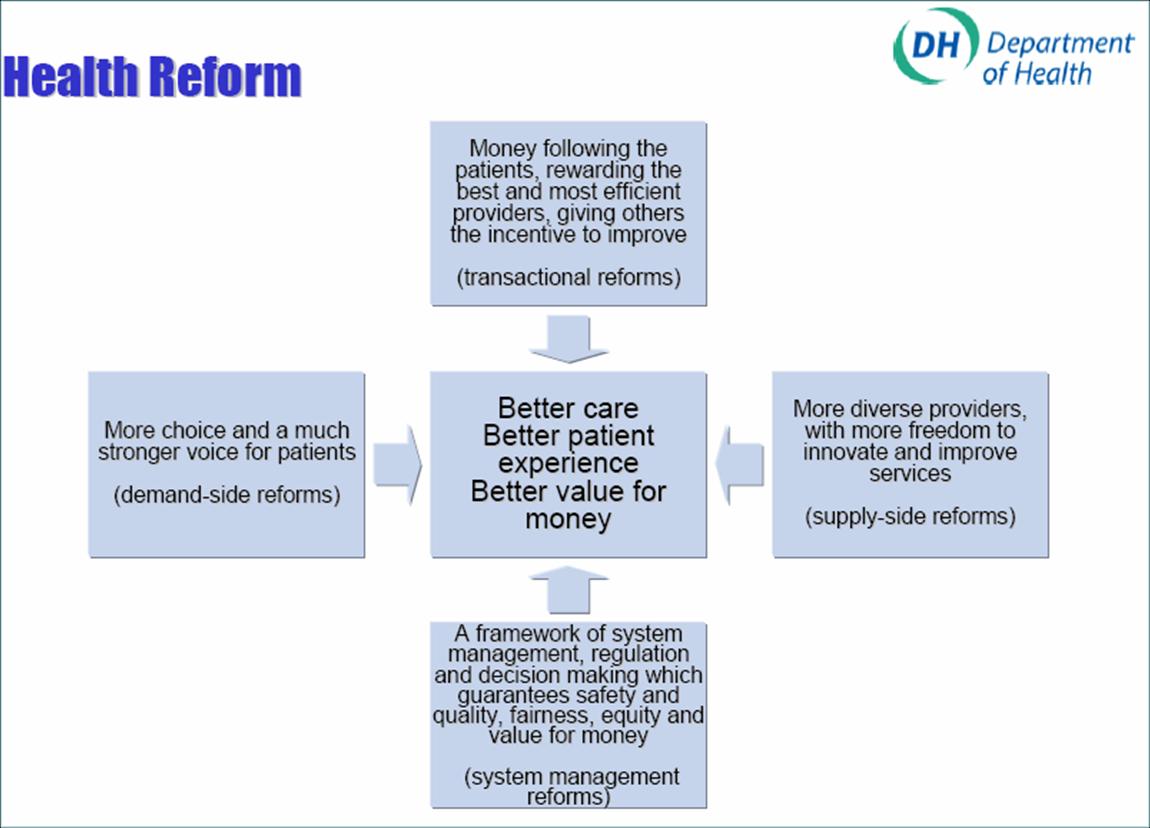
The DH framework for developing policy:
Given this uncertainty, should reform go faster or slower?
Faster: “Contrary to what critics claim the reforms are not the cause of the problems, but the solution. The reform agenda is vast and is effectively a revolution. The outcome will be better healthcare still free at the point of use (Tony Blair speaking today at his monthly press conference).
Slower: “The government must slow down the implementation of some NHS reforms to give the service a chance to regain financial balance. “We need an urgent review of the key changes to make sure we push forward the things that are needed to make a rapid difference, while being more measured on initiatives that have a longer-term payback”. (Gill Morgan, ceo of the NHS Confederation)
Have doctors retreated, or been alienated from health policy and service reform?
Building blocks from the system reform conference that need cementing together
Commissioning
|
Reconfiguration
|
Values
|
Future services
|
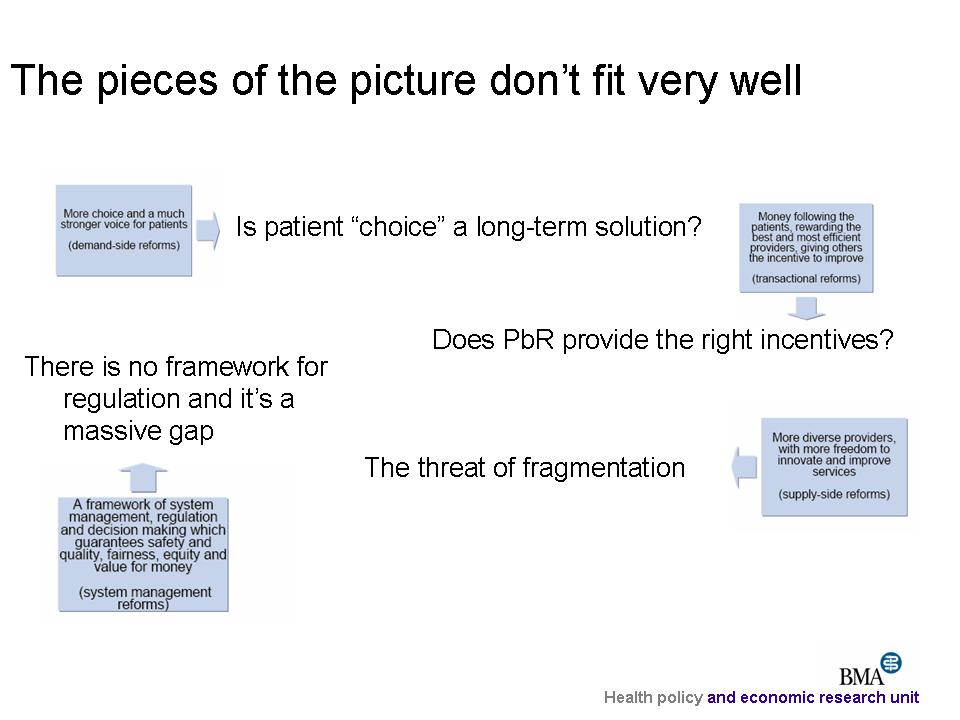
The system needs regulation to address uncertainties
The operating framework within which the NHS works, needs to be established. A lot of the uncertainties in Payment by Results, choice and plurality are compounded by the lack of a regulatory structure. A structure is needed that covers all providers, which safeguards systemic thinking and creates a level playing field between providers.
- We need a seamless service – fix the rough edges around poor connections
- A strategy is needed for failing systems
- We need audit across the board
- Training in ISTCs is needed
- A level playing field across all providers.
The critical question of ownership:
The question of ownership has become increasingly fraught. GPs are independent providers, but also more than that. They are plumbed into the system, rooted in the community, connected with patients
The plight of the employed
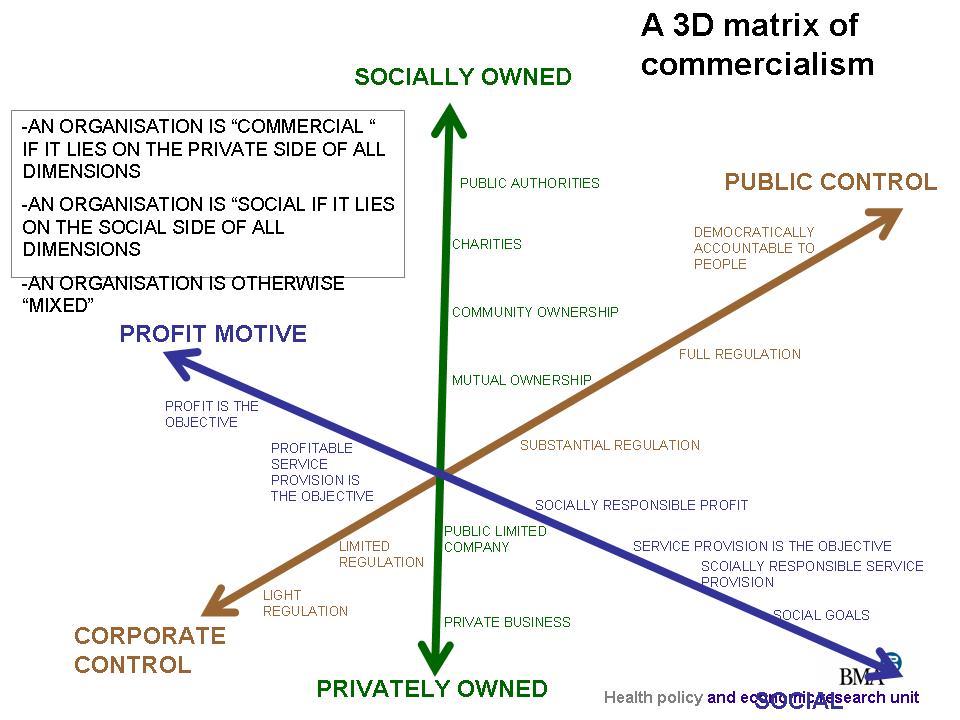
Questioning the involvement of the private sector:
Does it matter who provides the service? (The Clause IV debate)
- “Elephant and gnats” – a picture of the NHS and new providers
- Can regulation be maintained to ensure small independent organisations? (Can we have the Parisian rather than London model?)
- An increasing concern relates to the long-term impact of plurality and a fear that it tends towards the take-over of small business by large ones; a fear that health will become a corporate concern rather than consisting of providers rooted in the community
Simplifying health policy: for or against private involvement
Is all private provision wrong?
The real issue is ownership over work
Social enterprise
These new organisations provide a way of doctors to form collaborations
Are social enterprises a rearguard action against the private sector – to try to retain the NHS ethos in a more pluralistic health service or simply a step towards privatisation of the NHS? (Health Service Journal)
Social enterprises are seen as a way of protecting areas from private sector influence
Although GPs are sometimes described as “independent contractors”, they are more than this. They are rooted in communities and have the potential to better engage and involve patients in service improvements
Regulation in a changing world
The Donaldson report is a little old-fashioned
- Devolution
- It implies a stability within organisations that is not present
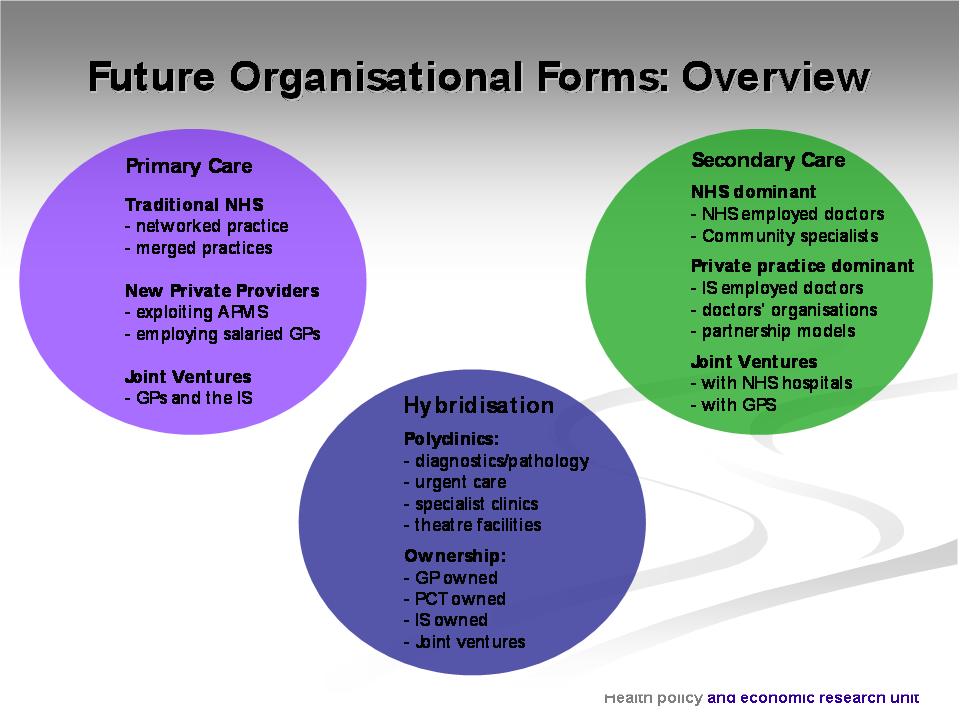
- What about the independent sector?
- Changing employment models in England
- Strengthen quality focus within organisations
- Stop management looking up to politicians rather than down to organisational development
- Panels of affiliates across regions
The importance of professionalism to effective reform:
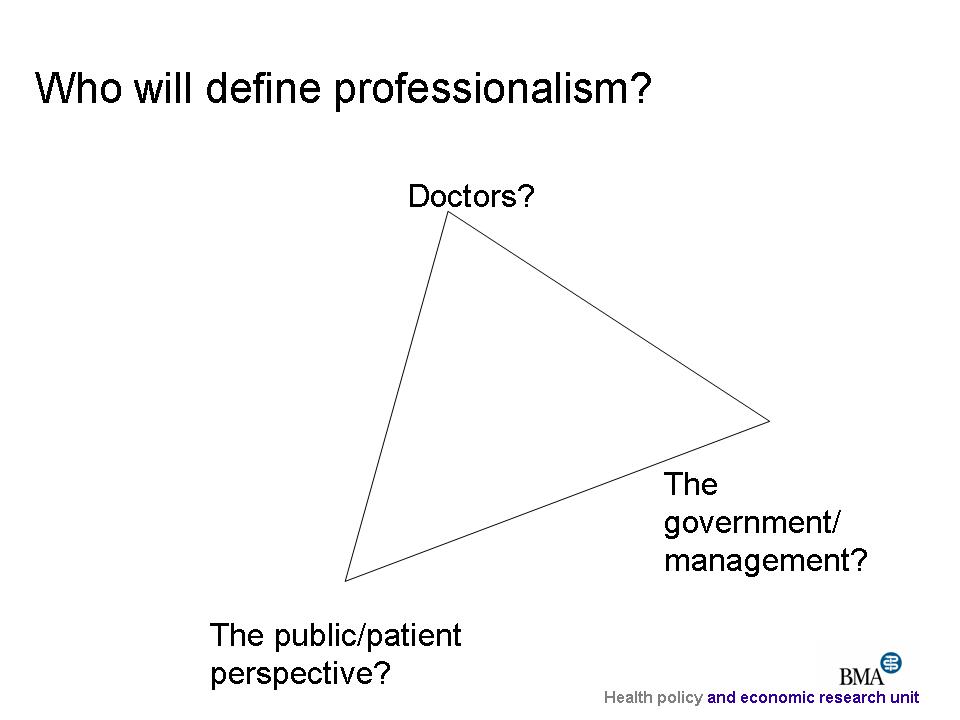
There is an unhelpful stand-off between the government and the professions
- More than anything, greater consultation and engagement is needed
- Policy has gone as far as it can without the active support of the professions
- Talk of “devolving power”, “independent boards” and so on must not replicate the same divides we have now. An element of devolution to the profession is needed, a change in approach which cuts against the grain of the Donaldson report
- Doctors need to re-engage with health policy and play a leading role in reform
The government’s search for a “narrative” to explain reform
“We have now reached crunch point where the process of transition from one system to another is taking place” T Blair (18th April 2006)
“The stakes are high. If we fail to reform the NHS, the privatisation agenda will take over” P Hewitt (24th April 2006)
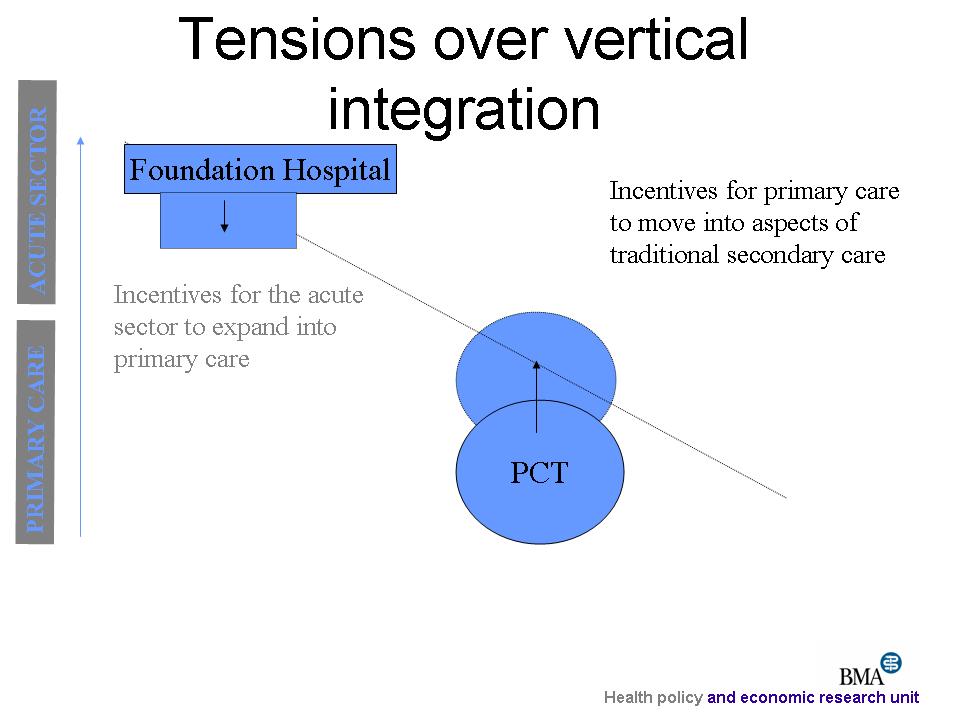
Potential tensions within reconfiguration:
Between doctors and clinicians
The Royal College of Surgeons reconfiguration working party
- Critical need to work across primary and secondary sectors
- Between the public, managers and doctors
- Reconfiguration will cause local concern
An independence of view is critical
The exercise of medical professionalism is hampered by a fiercely disabling environment. Yet the conditions of medical practice are critical determinants for the future of professionalism
Doctors need to have an independence that strives for clinical quality
Physicians are the stewards for quality, and they must aggressively develop an agenda for improvement…we are at a critical cusp of time in which we have a last chance to retain our professional role, and to do so we must become protectors of quality. Activism must persist and grow if we are to promote the professional/quality link at the level of patient care. This responsibility reaches to every physician.”
Brennan TA. Physicians’ professional responsibility to improve the quality of care. Acad Med 2002; 77: 973-80.
Conclusion:
The Donaldson report is not catching the headlines on the NHS at present – Plurality, financial deficits, reorganisation
Yet it could be argued that it is one of the more important current proposals because it offers a way of changing fundamental relationships between doctors and organisations
A change is needed but one that is more cultural than structural with a local focus on quality improvement and service development. There is a need to revive clinical governance
Professionalism needs to be renewed; doctors need to be more engaged in health policy and service change
see Doctors in Society Royal College of Physicians

