Caution … this is a dated opinion piece – there is ongoing work in this area.
Cost of the NHS Market
The cost of the “internal market” has been the subject of speculation with some claiming that £10bn would be saved if it was scrapped and the purchaser/provider split abolished. Does this stand up to any kind of analysis? If the system was replaced by one more like that in Wales how much could be saved?
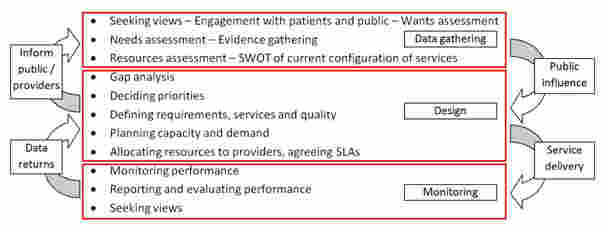
First there does need to be some agreement about what planning/commissioning involves. For any efficient system there has to be some objective basis for service planning, priority setting, allocation of funds, performance management. Hopefully this would be underpinned by good information and informed by local public and patient involvement.
The conceptual cycle can be illustrated by:-
These functions would be necessary in any system, and so would have to be paid for.
An estimate can be made of the cost of having the market over and above the cost that would have to be incurred just to carry out the necessary functions as above. The market means that commissioners and providers are joined by enforceable contracts, some agreed after various forms of tendering.
In the system as at 2009/10 the main costs were not in provider organisations that typically would only employ 5 – 10 staff whose jobs were solely related to market activities such as invoicing, contract disputes, and transaction level financial analysis. Most providers would accept that even now their information base around coding, activity based costing and service line accounting are still inadequate and if there were less “market” they would redeploy staff into these areas to improve internal management information. Given 260 providers the staff savings would be from £50m to £100m pa including some additional costs which might be envisaged around legal and contractual advice. No savings would be likely from estates or IT.
The 150 odd PCTs had a range of functions connected with commissioning and employed staff on many aspects of service design, monitoring, contract negotiation, and on a scale which did require some additional estate and IT. There are also legal and other external costs involved in running procurement exercises. There is much variation but something like 10 highly paid and 40 well paid staff can be assumed, on average, per PCT whose jobs depended on the “market”. A staff cost saving of around £300m – £400m would be reasonable. External costs might add £100m if competition and tendering took root. There are costs in SHAs and also in the DH but not on anything like the same scale.
Since 2010 there has been a dramatic reduction in staff in PCTs and SHAs shifting to clusters and nothing much has happened so it appears the costs could have been reduced anyway.
So overall an end to the “market” might save between £500m and £750m. A worthwhile sum but not anything like the £10bn claimed.
A rise in the volume of market transactions and the number of contracts is inevitable under the H&SC Act but the extent is a matter for speculation – depending on enthusiasm of CCGs for abuse. But as a reality check the allowance for all clinical commissioning groups in the new system is £25 per head which equates to about £1.25bn to which could be added a further £300m for specialist and other NCB led commissioning. But as set out above not all the functions associated with “commissioning” disappear when there is no market – there is still activity outside the providers which must be carried out. If we consider the function then assume a 50% split then the cost of the market in the new world would be of the order of £750m.
The calculations assume that it would be easy and cost free to identify the jobs and to make the job holders redundant and so to make the savings. It is unlikely to be that simple.
So at best the savings from ending the market and ending the formal C/P split replacing it by a planning system would be likely to be around £500m – £750m at best – only a small fraction of what is often claimed.