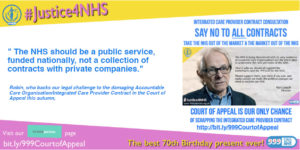
Scrap a new contract that could wreck our NHS!
The quango NHS England is currently holding a badly-publicised public consultation on its new Accountable Care Organisation contract – which it has renamed the Integrated Care Provider contract.
Most people won’t have heard about this. Have you?
Why is NHS England consulting on it now, before they even know if their new contract is lawful?
This autumn, 999 Call for the NHS is challenging the lawfulness of this contract in the Court of Appeal.
Many thanks to over 750 individuals, NHS campaign groups and trade union branches, who have crowdfunded the £18K costs of the Appeal through CrowdJustice – info here. http://bit.ly/999CourtofAppeal
NHS England’s consultation is online here.
999 Call for the NHS’s response is online here. (Downloadable word doc.) You’re welcome to use and adapt it for your own response. We do not accept the basic premise of the consultation – that contracts are an appropriate way of planning, delivering and managing NHS services. We are campaigning for the NHS Bill to reinstate the NHS as a fully publicly funded, managed and provided service.
If you prefer a consultation that is shorter and more to the point, 999 Call for the NHS will shortly be carrying out our own consultation online. Please come back soon to find the link. We will collect the responses and send them to NHS England before their consultation ends on 26th October.
The proposed new contract might sound like a dry legal issue that’s hard to get bothered about. The reality is anything but.
This is about whether patients can continue to access the treatments they need, or whether the doctor – patient relationship will be undermined by making doctors put financial considerations ahead of patients’ clinical needs.
This new 10 year contract is driven by NHS England’s cost-cutting aim of avoiding a projected £22bn funding shortfall by 2020/21 – the result of nearly a decade of NHS underfunding by the government.
The Accountable Care Organisation/Integrated Care Provider contract would pay a new type of legal entity for a whole range of NHS and social care services in a given area. It would use the same lump sum payment arrangement that has been used to pay for psychiatric intensive care – with disastrous results. Just think about the dire shortage of acute mental health beds.
This contract is explicitly intended to “manage demand” for NHS services – in other words, to restrict patients’ access.
Its cost-cutting payment mechanism would drive down safety standards as well as restricting patients’ access to care.
An Integrated Care Provider could be a private company or joint venture
The new type of single legal entity could be an NHS organisation like a hospital Trust, or a GP Federation, a private company or a joint venture or special purpose vehicle that could include NHS providers and private companies.
This is a complex contract where the legal entity that holds the contract would then subcontract to a number of different healthcare providers – whether NHS, private or 3rd sector companies. This comes with all sorts of risks and hazards. (For more info, see our answers to questions 3,4 and 5 in NHS England’s Integrated Care Provider Contract consultation.)
The Contract’s wide loopholes would allow far greater privatisation of NHS services – under this contract, a private company could control the delivery of the whole range of out-of-hospital NHS and social care services for a large area. Or indeed could win multiple contracts across many areas, and so establish a near- monopoly.
NHS England has admitted that under current NHS and social care legislation, it is powerless to stop private companies bidding for this – or any other – contract.
Un-evidenced, cost-cutting “care models” and “modern workforce”
This Accountable Care Organisation/Integrated Care Provider contract is designed to cement new NHS “care models” that copy the USA’s Medicare/Medicaid system. This provides a limited range of publicly-funded health care for people who are too poor or ill to access private health insurance.
Under the new “care models, District General Hospitals are being cut and downgraded. Community Hospitals beds are being closed. Family doctors are going under, as they are asked to take on more and more while there is a shortage of GPs and GP funding is flat. They are being replaced by huge new GP super practices serving 30K-70K patients, that are likely to become Integrated Care Providers.
Increasingly, these practices are being taken over by companies like Modality. Modality now operates in 7 Sustainability and Transformation Partnerships across England and has over 300,000 patients registered with it.
Budding local Accountable Care Systems (now rebranded as Integrated Care Systems) say that this is all fine, as care will be delivered out of hospital, in people’s homes, in large scale GP hubs and by means of digital technology.
But the new “care models” come with a “modern workforce” employing cheaper, less qualified new grades of staff – and relying on unpaid volunteers, friends and family.
None of this adds up to a comprehensive NHS that cares for everyone on the basis of clinical need. Instead care will be allocated on the basis of decisions about money.
NHS England laid out its plan for setting up these new care models in its 2015-2020 Five Year Forward View. Since then it has set up Vanguard schemes to trial these new ways of providing NHS and social care. There is just one small problem. There is no real evidence that they work. That is the conclusion of the National Audit Office report.
Opening the NHS to deregulated trade
The NHS quangos are aiming to change the whole architecture of the NHS, so it can deliver these American care models. All the better to open the NHS gates to American corporations, post-Brexit.
Stewart Player recently pointed out that
“…the aim is to impose a kind of global homogeneity of healthcare organization. Such standardization will attempt to safeguard and simplify investment strategies, and to embed corporate control of both purchasing and service delivery within rapidly evolving ‘mixed economies’ of care…
“The use of capitated budgets for ACO providers, for example, is expressly geared towards private investor interests, as the upfront capital can be invested in the global markets, with returns on equity in excess of 16%.”
