Good integrated healthcare or neoliberal con?

The Alzira Model is named after the town in Spain where the La Ribera hospital, the first hospital using this model, is located

The Alzira Model:
- Goes beyond the PFI model of the building being privately operated to also include clinical services
- Paid for by a capitation fee
- The first contract covered only the La Ribera hospital and was signed in 1997, the hospital opened in 1999 and the contract was terminated in 2003 due to losses.
- Replaced by second contract, which widened the remit to also manage the primary healthcare of the surrounding health area.
The Spanish National Health System
There are operational differences to UK NHS
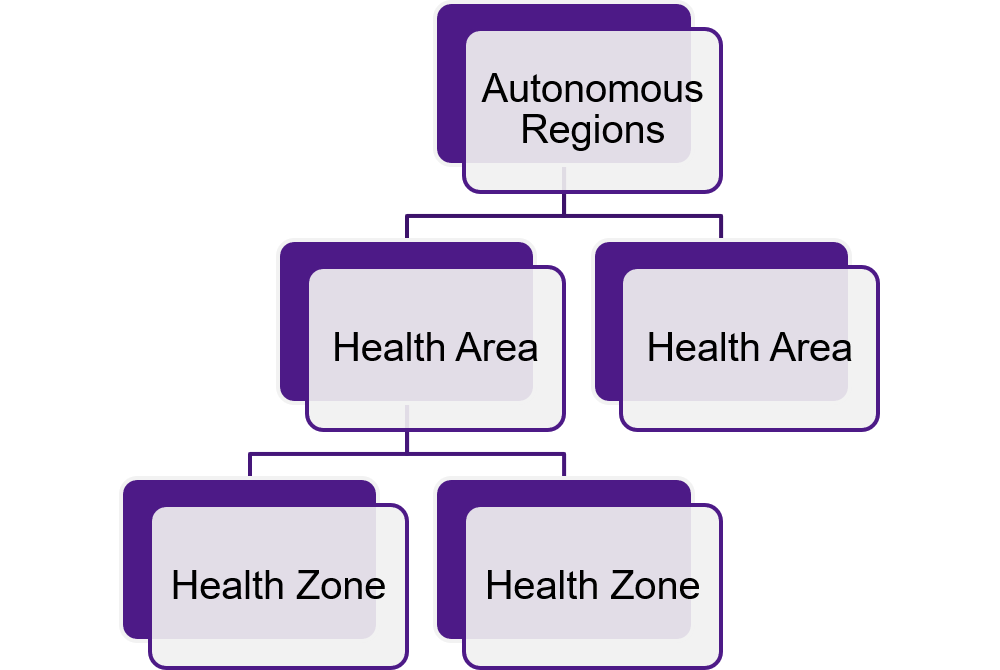
- Responsibility for healthcare has been devolved to the regions
- Specialist care (e.g. Children’s hospital) is covered at Health Area level
- A health zone contains a hospital plus primary health centres. Residents are allocated to primary health centres. (No choice of GP, as in UK) Residents are referred to hospital by a GP at their primary health centre.
The model was hailed as a tremendous success story by neoliberal groups around the world with the following claims:
- Cheaper to deliver than traditional public sector healthcare – savings of around 25% being achieved
- Good for patients and staff
- Affordable for the taxpayer
The Reality
(a) The Spanish context
- Labour costs in Spain: Clinical staff in public hospitals are part of the Spanish Civil Service, which has very generous pay, above OECD average, whilst working hours are less than average – if we compare to the UK NHS savings of around 20-30% can typically be made.
- Financing by regional savings banks Prior to financial crisis their governing bodies were dominated by regional politicians – so no risk transfer. Low rates of interest charged on loans
(b) No financial success story
- The integrated contract was only viable because of:
- Generous Increases in capitation fee in early 2000s
- Low interest rates
- Low labour costs
- Cherrypicking and freeriding
All of this was hidden due to poor governance systems and lack of accountability
Further flaws
- Very optimistic capitation fees at start
- 1st contract failed – political coverup on re-letting
- Wage protests
- High staff/patient ratios
- Additional costs of monitoring ignored
- Many items omitted from contract
- Recommended structures for managing PFI-style policy all missing in Spain (Specific Public/Private Partnership unit, model standardised contracts, public sector comparator, any method of project evaluation)
Proliferation of the Alzira Model
- Used for other integrated healthcare (i.e. hospitals and primary care) in Valencia region with similar findings
- When used elsewhere (both in Spain/elsewhere in world), it has tended to be for hospitals only
Implications
Given that it’s NOT a good cost effective way of delivering healthcare, what does the usage of the Alzira Model mean?
- A way of keeping artificially keeping debt off the public sector balance sheet?
- A way to impose an ideological right wing view of creating a market for healthcare?
Performative Frame
- Superiority of private sector style techniques in delivering a better quality service
- Linked with political will to create a market for Public/Private Partnership healthcare over the long term – shift from infrastructure (just 5% of global healthcare spend) to clinical services (lucrative and stable long term returns)
- Increasing involvement of healthcare companies
Conclusions
Breakdown of Alzira model in Valencia
Regional government changes from right wing Partido Popular to left wing coalition who scrap the policy amid corruption scandal of director of the healthcare group
The rhetoric of success from global consultants needs to be challenged
This was presented at our conference on Accountable Care Systems
