This is a slightly edited version of Chapter 6, the discussion of health inequalities policy, from the book Health Divides. The printed version is fully referenced.
Previous chapters have explored the relationship between health and place across different scales showing consistent evidence of spatial inequalities in health within local areas, between the regions and countries of the UK, as well as within and between countries internationally. They have shown that the causes of geographical inequalities in health are complicated and multifaceted, a combination of compositional (people), contextual (environment) and ultimately political and economic factors. This chapter examines how public policy has had an impact on health divides using a case study of the UK since the 1980s. It provides an overview of health inequalities policy since 1979, drawing on the key actions during this period. The successes and failures of UK policies in terms of reducing health inequalities are critically examined with reference to the wider context of the neoliberal political economy and the social and spatial determinants of health.
The UK is chosen as a case study because the Thatcher governments of 1979—90 played an important role in the promotion of the international neoliberal policy agenda, which remains influential today; because the Blair Labour governments from 1997 to 2010 implemented the most extensive health inequalities strategy in Europe; and because the coalition and Conservative governments since 2010 implemented austerity. The chapter critically reflects on how policy has had an impact on health inequalities from 1980 to 2015, analysing some of the key developments in this period. It ends by reflecting on what could or should have been done, drawing on evidence from a series of government-commissioned reviews into tackling health inequalities.
Thatcherism and health inequalities, 1979-97
The need to reduce health inequalities across the UK contributed to the decision to establish the National Health Service in 1948. Yet, despite this universal, free at the point of use health service, by the 1970s it was becoming increasingly evident that free access to healthcare had not been enough to stem socioeconomic and spatial inequalities in health. In as far as a health inequalities policy existed at this time, it was within the NHS. So, in 1977, the Labour government (1974-79) faced fresh calls to do something about the issue. They responded by asking the Chief Scientist, Sir Douglas Black, to appoint a working group of experts to investigate the issue and to make policy recommendations for the government. The resulting report, which is widely referred to as the Black Report, argued that materialist explanations were likely to play the largest role in explaining health inequalities, and, therefore, that policy-makers ought to prioritise the reduction of differences in material and economic circumstances between socioeconomic groups and between deprived and affluent areas. The report was published in 1980 (on a Bank Holiday Monday in August to minimise publicity, and with only 260 copies produced), when the commissioning Labour government (left-wing, social democratic) had been replaced by the first Thatcher-led Conservative (right-wing, neoliberal) government (1979-83). The new government wholeheartedly rejected the report’s recommendations (which included increasing welfare benefits and decreasing child poverty). In an infamous foreword to the report, Patrick Jenkin, the then Secretary of State for Social Services, claimed that the report was ‘wildly unrealistic’ and ‘seriously flawed’. This set the tone for the next 20 years as, under the Conservative governments of 1979—97, health inequalities were not on the official policy agenda at all. Even the term ‘health inequalities’ was discarded, and health differences between socioeconomic groups and places were instead referred to using the less emotive term, ‘health variations’, implying that health differences could be ‘natural’, individual and therefore not something for which politicians and policy-makers were responsible.
Table 6.1: Overview of the Black, Acheson and Marmot reports
| Black Report | Acheson Report | Marmot Review |
| The Black Report (1980) on health inequalities was commissioned by the outgoing Labour government in 1977 and brought health inequalities into the spotlight and represented the first example of a comprehensive strategy to draw attention to health inequalities over the life course. Health inequalities were not recognised as a problem by many at the time. | The Independent Inquiry into inequalities in Health chaired by Sir Donald Acheson was commissioned by the newly-elected Labour government in 1997, which committed itself to implementing the evidence-based policy recommendations. | Following publication of the WHO report on the social determinants of health, Sir Michael Marmot was commissioned to consider the implications for health inequalities in England post-2010. As with the Acheson Inquiry, the Marmot Review was expected to make evidence-based recommendations. |
Aims |
||
| 1. To assemble available information about the differences in health status among the social classes and about factors which might contribute to these, including relevant data from other industrial countries; | 1. To review the latest available information on inequalities of health, to summarise the evidence of inequalities of health and expectation of life in England and identify trends. | 1. Identify, for the health inequalities challenge facing England, the evidence most relevant to underpinning future policy and action |
| 2. To analyse this material in order to identify possible causal relationships, to examine the hypotheses that have been formulated and the testing of them, and to assess the implications for policy; | 2. In the light of that evidence, to conduct – within the broad framework of the Government’s overall financial strategy – an independent review to identify priority areas for future policy development, which scientific and expert evidence indicates are likely to offer opportunities for Government to develop beneficial, cost effective and affordable interventions to reduce health inequalities. | 2. Show how this evidence could be translated into practice |
| 3. To suggest what further research should be initiated. | 3. To report to the Secretary of State for Health. The report will be published and its conclusions, based on evidence, will contribute to the development of a new strategy for health. | 3. Advise on possible objectives and measures, building on the experience of the current PSA target on infant mortality and life expectancy |
| 4. Publish a report of the Review’s work that will contribute to the development of a post-2010 health inequalities strategy. | ||
Explanatory theory |
||
| Took a multi-causal approach to explaining health inequalities but suggested the role of behavioural and cultural determinants in producing inequalities in health were significantly outweighed by the role played by economic and social conditions. | Acheson also supported a multi-causal approach to explaining health inequalities, using a model composed of different layers including individual lifestyles and the socioeconomic environment. Similarly to Black, this approach emphasised the importance of material and structural conditions in shaping other key determinants, such as lifestyle-behaviours. | The distribution of health and wellbeing is once again understood to be caused by interplay of various determinants, with material circumstances playing an important role. However, psychosocial factors such as social cohesion, and other social stresses are given more prominence in explaining the relationship between material inequalities and health inequalities. |
Key Recommendations |
||
| 37 recommendations, prioritizing giving children a better start in life within a wider anti-poverty strategy | 39 recommendations; key priorities similar to those of Black report, namely; | 6 policy objectives: |
| 1 . All policies likely to have an impact on health should be evaluated in terms of the impact on health inequalities. | 1. Give every child the best start in life | |
| 2. High priority should be given to health of families with children. | 2. Enable all children, young people and adults to maximise their capabilities and have control over their lives | |
| 3. Further steps should be taken to reduce income inequalities and improve living standards of poor households | 3. Create fair employment and good work for all | |
| 4. Ensure healthy standard of living for all | ||
| 5. Create and develop healthy and sustainable places and communities | ||
| 6. Strengthen the role and impact of ill health prevention |
See also Tackling Health Inequalities in the UK 1997-2010 – Evaluating the Acheson report
Understanding Thatcherism, Conservatism and New Right ideologies in this period helps explain why Thatcher’s government made the decision to reject the recommendations put forward in the Black Report (1980). Margaret Thatcher (1925-2013) was UK Prime Minister from 1979—90. Her critique of UK social democracy during the 1970s and her adoption of key neoliberal strategies, such as financial deregulation, trade liberalisation and the privatisation of public goods and services, were popularly labelled ‘Thatcherism’. Thatcherism was an ideological project that set out to radically re-cast the relationship between labour and capital and between the state, society and the individual. Thatcherism and the New Right provided a narrative that explained the crisis of British capitalism in the 1970s as a crisis of the welfare state, high wages and low productivity, of the ‘undemocratic’ power of what in 1984 she called ‘the enemy within’, that is, the trade unions. Thatcherism set out to systematically dismantle the structures of the post-war Keynesian consensus around the social wage, full employment, the corporatist state and the size and role of the public sector. This goal was pursued through the aggressive promotion of the free market alongside the ‘hollowing out’ of the state.
Thatcher’s political programme included:
(1) deregulation of the labour and financial markets (including the ‘big bang’ deregulation of the City of London in 1986);
(2) the privatisation and marketisation of the main utilities (water, gas and electricity) and state enterprises (for example, British Steel, British Rail and British Airways);
(3) the promotion of home ownership (including the widespread sale of public housing stock under the ‘Right to Buy’ scheme);
(4) the curtailing of workers’ and trade union rights (for example, bans on the ‘closed shop’, obligatory membership ballots before any industrial action, restrictions on the right to picket including a ban on secondary picketing, and removal of trade union immunity from damages);
(5) the promotion of free market ideology in all areas of public life (including healthcare and the civil service);
(6) significant cuts to the social wage via welfare state retrenchment (for example, a 7% reduction in state expenditure on social assistance between 1979 and 1989; removal of 16- to 18-year-olds from entitlement; reductions in state pensions; abolition of the inflation link for welfare benefits);
(7) an acceptance of mass unemployment as a price worth paying for the above policies; and (8) large tax cuts for the business sector and the most affluent (for example, during Thatcher’s premiership, the rate of Income Tax for the top tax bracket was reduced from 83% to 40%).
These changes all led to a fundamental rebalancing of British economic and social life that saw a reassertion of social class divisions. The growing economic equality experienced as a result of UK social reforms since 1945 was reversed, with income inequality increasing significantly (for example, the richest 0.01% had 28 times the mean national average income in 1978, but this increased under Thatcher’s tenure to 70 times in 1990). Additionally, as a result of welfare state retrenchment, high unemployment and falling wages for many poorer workers (due to the decreased bargaining power of trade unions), there was a near doubling of poverty rates in the UK, from 6.7% in 1975 to 12.0% in 1985 By the 1990s and 2000s, these new high levels of income inequalities and poverty became normalised. Social mobility gains were also stalled via changes to the education system as well as the ‘lost generation’ of young people who left school and went straight onto ‘the dole’ in the early 1980s. From 1980, the number of unemployment claimants rose from around 1 million to around 3 million in 1983, and a further peak was seen in the early 1990s. Meanwhile there was also a steady rise in the number of claimants of long-term sickness (disability) benefits. The rise in the number of disability benefit claimants has been attributed to a government desire to move people off the unemployment register and because of the lack of jobs in the economy.
The new economy that emerged in the 1980s was seriously unbalanced. Manufacturing and extraction industries, public utilities and collective housing provision were displaced by finance and banking industries, privatised utilities and rampant property speculation. The ‘big bang’ of 1986 saw the deregulation of the City of London, and with that, the unleashing of hitherto unimaginable forms of financial speculation. The ostensible ‘giving power back to the people’ through privatisation led, in fact, to the radical de-democratisation of the power industry — now largely externally owned — and other utilities. And the ambition to create ‘a nation of homeowners’ produced a mushrooming of homelessness due to a chronic shortage of affordable social housing, creating the preconditions for the more recent emergence of a new breed of ‘Buy to Let’ landlords charging ‘market rents’. It also underpinned a new culture of speculation and chronic indebtedness – on which a new breed of amoral ‘entrepreneurs’ in banking and finance would be able to prey. All of this generated sharply increased inequalities of income and wealth across Britain, and a dramatic increase in poverty. It also put in place most of the prerequisites for the great banking and finance crisis of 2008. In this way Thatcher’s governments wilfully engineered an economic catastrophe across large parts of Britain, and began the dismantling of the welfare state and the privatisation of the NHS in England.
The impact of these changes on other key social determinants of health was, in many cases, dramatic. Inequalities in educational outcomes and in access to healthcare, for example, both increased following policies implemented under Thatcher’s leadership. In housing, Thatcher’s government quickly implemented a ‘Right to Buy’ initiative, which gave council tenants the right to purchase the homes they occupied, often at greatly discounted rates. This policy reflected the ideological belief in the superiority of the market and was popular among many of those it helped move into the housing market. However, it contributed to the growing wealth inequalities and, more broadly, the policies of Thatcherism sowed the seeds of the housing market crash in 1989, which left many homeowners trapped by ‘negative equity’. Meanwhile, as the better quality houses were sold off, local councils were left with responsibility for a far smaller and increasingly poor quality housing stock. All of this contributed to growing levels of homelessness. Longer term, these significant changes in housing policy also resulted in the current housing crisis in the UK.
Although Thatcher backed off from any wholesale reform of the NHS, allegedly fearful of an adverse public reaction to such a move, her government did introduce a number of policy initiatives that set the NHS on a course from which it has not deviated since. That course might be characterised as a shift from a welfare state to a market state. The most significant NHS development that took place under her premiership was the introduction of a quasi-market in healthcare centred round competition and choice. Among the most controversial changes Thatcher introduced was the policy of contracting out or outsourcing, introduced in 1983, whereby health authorities were required to set up competitive tendering arrangements for their cleaning, catering and laundry services. Additional non-clinical services were later added to the list. The main significance of this development was the establishment of the principle that the core responsibility of health authorities was no longer to directly provide non-clinical services, but merely to ensure that they were in place at the least cost. A key negative impact was a loss to the public sector ethos of the NHS in which, for example, cleaners were perceived as members of the ward team, whose friendly, reassuring presence made important contributions to the wellbeing of patients. This contribution disappeared once the tight schedules of competitive contract cleaning took over. Equally important was the perception that ward cleaning became substantially less thorough, leading over time to the current high prevalence of hospital-acquired infections. The NHS and Community Care Act 1990 introduced market-style mechanisms into the NHS, notably the purchaser—provider separation and GP fundholding, whereby GPs were allocated budgets that they were free to spend as they saw fit, to meet their patients’ needs. This marked a substantial break with the past, and opened up the NHS to market forces.
These significant and rapid social and economic changes had an impact on health divides in the UK. Mortality rates in the UK, and across Western and Central Europe, have been improving for around 150 years. This long-run improvement continued throughout the period of the Thatcher government, with all-cause mortality rates declining at a similar rate to those in other countries and compared to the time periods before and after. However, underlying the overall improvement in mortality rates, some specific causes of mortality increased markedly, either during the period of the Thatcher government, or immediately afterwards. For example, alcohol-related mortality increased dramatically during the late 1980s and early 1990s in the UK in contrast to the improving trends in other parts of Europe.
Increases were also seen in drug-related mortality, suicide and violence at this time, all of which are causes of death that are clearly socially produced rather than due to biological or physiological mechanisms. Further, within the UK, mortality rates improved much more slowly in Northern and inner-city areas than in the more affluent Southern England, to the extent that in some local areas, mortality rates actually worsened. Indeed, for young adults in Scotland there has been no improvement over the course of the last 30 years. Figure 6.1 shows that the gap in mortality between the least and most deprived postcode areas in Scotland increased rapidly between 1981 and 2001, to leave Scotland with the highest inequalities in Western and Central Europe. The rise in spatial inequalities in health during the 1980s was also reflected in a rapid rise in mortality inequalities by occupational social class in England and Wales. Life expectancy increased for all social class groups among males and females over time, but the increase was more rapid among higher social classes than in lower ones, such that the inequalities increased (see Figure 6.1). The rises in cause-specific mortalities such as alcohol- and drug-related deaths, suicide and violence, and the widening health inequalities occurred during the same time period in which unemployment, poverty and income inequality all rose.
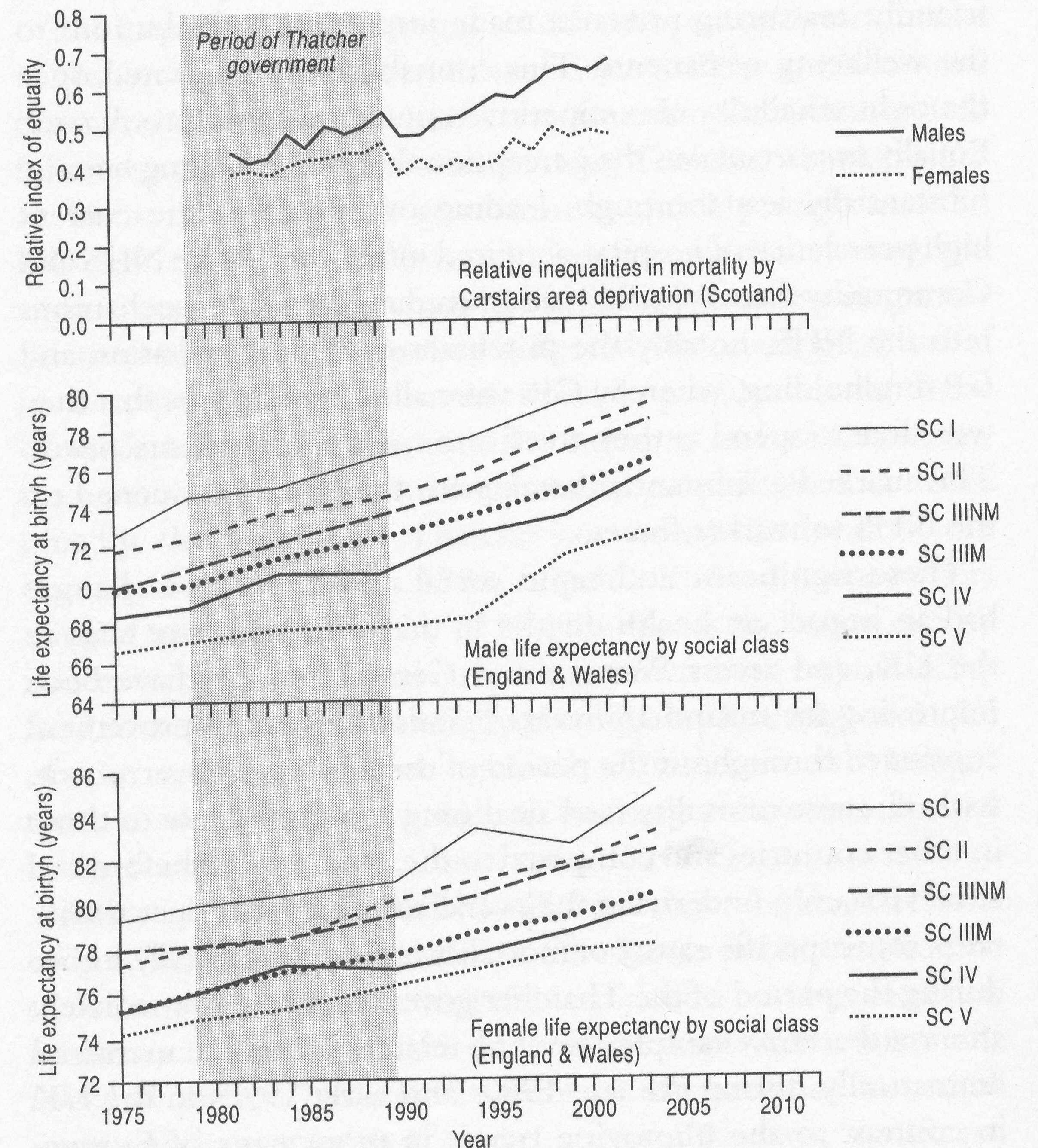
Figure 6.1: Trends in health inequalities in England and Wales, 1975-2003 (by occupational social class) and Scotland, 1981-2001 (by Carstairs area deprivation)
New Labour and health inequalities, 1997-2010
Labour was re-elected in 1997 with a landslide victory and a manifesto that had highlighted the need to tackle various social inequalities, promising to tackle the ‘root causes’ of ill health, such as poor housing and unemployment. The new government was keen to emphasise the previous Conservative government’s failure to address health inequalities. The Labour government initially criticised the Conservatives for placing an ‘excessive emphasis on lifestyle issues’, casting the responsibility for ill health onto individuals rather than the economic and social structures of society and the places where people live. In addition, and as promised in their manifesto, the Labour government commissioned a follow-up to the Black Report, announcing an independent inquiry into health inequalities. The Acheson Inquiry, as it became known, was commissioned by Tessa Jowell, the first ever Public Health Minister. On publication in 1998, its recommendations were officially welcomed, used as the basis of a new health strategy, and the government stressed that they were already implementing many of them.
In broad terms, many of the resulting Acheson Report’s 39 recommendations reflected the conclusions of the earlier Black Report: both highlighted the need to have a multifaceted approach to health inequalities, and both advocated a reduction in income inequalities, with a particular focus on child poverty.
The key difference was that the Acheson Report was released in a far more favourable political climate than its predecessor and might, therefore, have been expected to have more of a policy impact. However, Labour had also stipulated that the Inquiry’s recommendations should recognise the government’s fiscal commitments which, at that time, included a two-year agreement not to increase public spending. This restriction led to an under-representation of any attempt to tackle the fundamental economic and political determinants in the emerging policy initiatives that were linked to the report.
A wealth of policy statements referring directly to the report were produced, indicating that policy decisions had, as promised, been directly informed – or at least influenced – by the recommendations of the report. Certainly in the period 1997-2003, health policy across the UK reflected some of the ideas set out in the Black and Acheson Reports, including a consistent rhetorical emphasis on the need to tackle the social and economic determinants of health inequalities as well as a commitment to employing cross-cutting government policies (that went beyond the Department of Health and the NHS) to tackle health inequality. Most notably, by 2004, national targets to reduce health inequalities were also introduced with a focus on life expectancy and Infant Mortality Rate.
These targets, however, reinforced the idea that policy-makers could tackle health inequalities through specialised health improvement measures, directing efforts to the least well-off individuals and areas such as the Spearhead local authorities that were the 70 most disadvantaged local authorities in England. They all received additional financial resources to improve area health, and area-based initiatives emerged. These tried to get different sectors – particularly the NHS, local authorities and the voluntary sector – to work in partnership together to improve the health outcomes of a specific deprived area. Examples from this period include Health Action Zones, Healthy Living Centres, Health Improvement Programmes and New Deal for Communities . This target culture is perhaps one reason why, in the period 2004-07, public health policy moved away from the initial concern with social and economic determinants and instead focused increasingly on health services and lifestyle behaviours. This shift was associated with a reduction in the level of responsibility that the central government appeared to be taking for health inequalities, as policy documents increasingly emphasised the importance of individual responsibility for health outcomes. Targets to reduce health inequalities were abandoned across the UK in 2011.
Description of area-based health initiatives, 1997-2010
Health Action Zones (HAZs)
HAZs were area-based initiatives designed to tackle social exclusion and inequalities. Acknowledging the wider determinants of health, HAZs were intended to develop partnership working between the NHS, local government and other sectors with the aim of tackling ill health and persistent inequalities in the most disadvantaged communities across the UK. Initially 11 HAZs were launched in the first wave in April 1998, followed by a further 15 in April 1999. Collectively, HAZs were awarded £320 million over a three-year period. It was originally intended that the lifespan of HAZs would last between five and seven years, with successful services being mainstreamed thereafter. However, HAZs were effectively wound down by 2003.The projects facilitated by HAZs varied extensively, but included initiatives that aimed to address social and economic determinants (such as services providing advice on benefit support); promote healthy lifestyles (for example, breakfast clubs); empower individuals and communities (for example, a Gypsy and Traveller Project Advisory Croup); and improve health and social care services (for example, the Integrated Substance Misuse Service).
Health Improvement Programmes (HImPs)
HlmPs were action plans developed by NHS and local government bodies working together. They were introduced in 1999 and, despite being re-named Health Improvement and Modernisation Plans in 2001, they continue to form a key approach to public health in England. The plans set out how these organisations (with, where deemed appropriate, voluntary and private sector input) intend to improve the health of local populations and reduce health inequalities. The programmes offered a three-year plan for identifying local health needs and developing relevant strategies to improve health and healthcare services at a local level. HlmPs were founded on the basis of multi-agency partnership working between local government and regional Strategic Health Authorities (SHAs).
New Deal for Communities (NDC)
As part of the Neighbourhood Renewal Strategy, NDC was developed to tackle health and social inequalities experienced by the 39 most deprived communities in the UK. In partnership with local communities, NDC sought to address embedded issues of deprivation and long-term poverty by improving outcomes in terms of housing, education, employment and health. Interventions mainly focused on promoting healthy lifestyles, enhancing service provision, developing the health workforce and working with young people.
Healthy Living Centres (HLCs)
HLCs were introduced in 1998 to tackle the broader determinants of health inequalities and to improve health and wellbeing at a local level. Funding was awarded for 352 community projects that varied in terms of focus, ranging from service-related issues to activities addressing unemployment, poverty and social exclusion. Example interventions included health-focused projects such as a physical activity outreach programme in rural localities, support programmes such as a Community Health Information Project that trained members of the local community to act as ambassadors for HLCs, and services such as ‘Bumps to Babies’, which provided midwifery and health visiting services for young families.
The effects on actually reducing health inequalities of these policies between 1997 and 2010, however, have only been partial, and even these small effects have been superseded by recent events such as austerity. Following the election of a Labour government on a mandate that included a commitment to reducing health inequalities and implementing evidence-based policy in 1997, the UK became the first European country in which policy-makers systematically and explicitly attempted to reduce inequalities in health. A raft of policy measures designed to reduce health inequalities were introduced since 1997 (as previously described), and, although the UK’s political system has become increasingly fragmented as a result of political devolution in Northern Ireland, Scotland and Wales, health inequalities have remained consistently high on policy agendas throughout the UK. However, despite having the most systematic policy around health inequalities in Europe, by the time Labour left office in 2010, mounting evidence indicated that local health inequalities in the UK and between the countries of the UK had not changed substantially, and in some cases had continued to get worse.
The key targets of the Labour government’s strategy were to reduce the relative gap in life expectancy at birth between the most deprived local authorities (called Spearhead areas) and the English average by 10% by 2010, and to cut relative inequalities in Infant Mortality Rate between manual socioeconomic groups and the English average by 10%, from 13% to 12%. The strategy failed to meet its own targets as the relative gap actually increased between 1995/97 and 2008 by 7% in terms of male life expectancy and by 14% in terms of female life expectancy. However, the relative gap between manual socioeconomic groups and the England average for Infant Mortality Rate actually fell between 1995/97 and 2007/09 from 13% to 12%, with a further fall to 10% in 2008/10.The latter represents a reduction in relative inequalities of 25%.The absolute gap also decreased from 0.7 in 1997/99 to 0.5 in 2007/09 with a further fall to 0.4 in 2008/10, an overall reduction of 42%. This suggests that regarding its own – albeit very limited – terms, the English health inequalities strategy was partially successful.
Table 6.2: Infant mortality rates in England, routine and manual socioeconomic group compared with national average (infant deaths per 1,000 live births)
| Time Period | Routine and Manual | EnEnglish Average rate | Absolute gap | Relative gap |
| 1997-99 | 6.3 | 5.6 | 0.7 | 13% |
| 2002-04 | 5.9 | 5.0 | 0.9 | 18% |
| 2003-05 | 5.7 | 4.9 | 0.8 | 17% |
| 2004-06 | 5.6 | 4.8 | 0.8 | 16% |
| 2005-07 | 5.4 | 4.7 | 0.7 | 16% |
| 2006-08 | 5.3 | 4.5 | 0.7 | 16% |
| 2007-09 | 5.0 | 4.4 | 0.5 | 12% |
| 2008-10 | 4.7 | 4.3 | 0.4 | 10% |
| Change since 1997-99 | -1.6 | -1.3 | -0.3 | -3.0 |
| % change since 1997-99 | -1.2 | -0.7 | -0.5 | -8.0 |
Another area of success of the strategy was around inequalities in ‘mortality amendable to healthcare’. Amenable mortality is defined as mortality from causes for which there is evidence that they can be prevented given timely, appropriate access to high-quality care.’ NHS funding was increased from 2001 when a ‘health inequalities weighting’ was added so that areas of higher deprivation received more funds per head to reflect their higher health needs. Analysis has shown that this policy -of increasing the proportion of resources allocated to deprived areas compared to more affluent areas — was associated with a reduction in absolute health inequalities from causes amenable to healthcare. Increases in NHS resources to deprived areas accounted for a reduction in the gap between deprived and affluent areas in male ‘mortality amenable to healthcare’ of 35 deaths per 100,000 and female mortality of 16 deaths per 100,000. Each additional £10 million of resources allocated to deprived areas was associated with a reduction in 4 male deaths per 100,000 and 2 female deaths per 100,000.
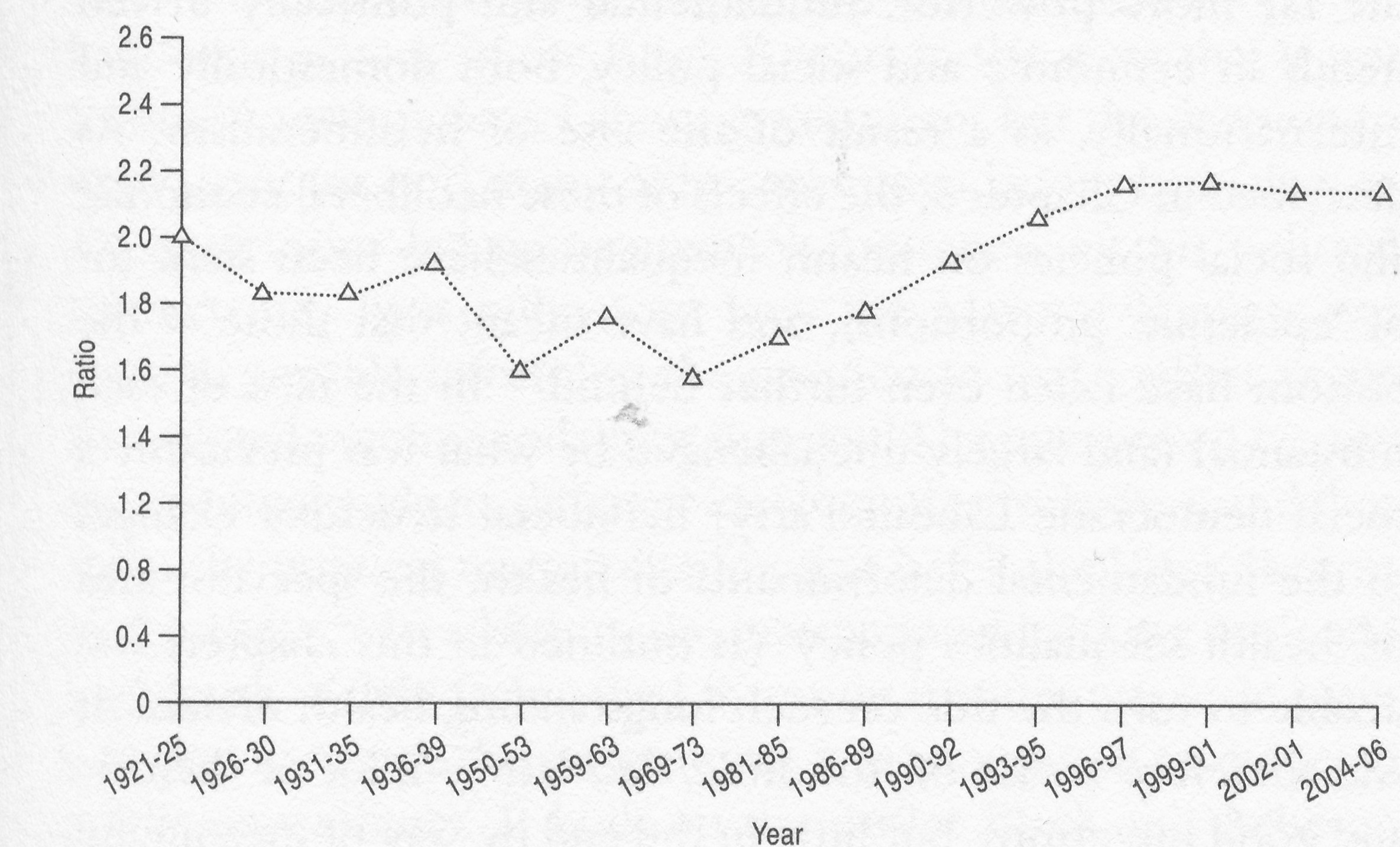
Figure 6.2: Divide in under-65 years death rates between the 10% most and 10% least affluent neighbourhoods in England, 1920s to mid-2000s
However, when looking beyond these arguably rather minor changes in very specific areas (Infant Mortality Rate and mortality amenable to healthcare) and examining the broader social and spatial patterning of death and disease, health inequalities remained high, and indeed grew during this period. This is shown in Figure 6.2, which tracks trends in the size of the gap in death rates between the most and least affluent 10% of neighbourhoods for those aged less than 65 from the 1920s to the mid-2000s. The health divide between the richest and poorest areas had decreased until the late 1970s, but then increased since the 1980s and throughout the post-1997 years of the Labour government.
The most important reason for the very limited success of health inequalities policies in the UK since 1997 is the ‘lifestyle drift’ whereby policy went from thinking about the wider economic and social context to focusing almost exclusively on the individual-level, behavioural, compositional factors. The only very limited success of the English strategy is therefore because there is only so much that can be achieved by focusing on individual behaviour change or the provision of more smoking cessation programmes or by increasing access to healthcare services. While there were policies enacted under the 1997-2010 New Labour governments that focused on the more fundamental determinants (for example, the implementation of a national minimum wage, the minimum pension, and tax credits for working parents, and a reduction in child poverty) as well as significant investment in the NHS, there was, however, little redistribution of income between rich and poor individuals or areas. Nor was there much by way of an economic rebalancing of the country (for example, between North and South). Indeed, a senior Labour government minister claimed at the time that he was ‘seriously relaxed’ about people getting rich. Further, in wider policy, the New Labour governments continued the neoliberal approach of Thatcherism – including, for example, further marketisation and privatisation of the NHS.
Health inequalities policy was therefore overshadowed by the far more powerful, fundamental and politically driven trends in economic and social policy, both domestically and internationally, as a result of the rise of neoliberalism. The effects of these neoliberal economic and social policies on health inequalities have been stark (or of ‘epidemic’ proportions), and have meant that those at the bottom have fallen even further behind. In the face of such substantial (and largely unchallenged by what was previously a social democratic Labour Party) neoliberal structural changes to the fundamental determinants of health, the specialist area of ‘health inequalities policy’ (as outlined in this chapter) was unable to turn the tide on such longstanding health divides. It was therefore a case of ‘too little, too late’ – a lot of rhetoric and good intentions, but little in the end by way of meaningful action. The earlier post-war experience — in which smaller health inequalities were achieved through a more extensive welfare state and a different spatial and socioeconomic distribution of national wealth — and the results of the various policy reviews examined earlier in this chapter – do, however, provide clear evidence as to what is actually needed to really ‘turn the tide’ on health divides. The likelihood of such substantial change happening became even more remote with the election of the coalition (Conservative—Liberal Democrat) government in 2010 and then another Conservative majority government in 2015, both of which were committed to neoliberal-inspired austerity.
Coalition, (more) Conservatism and health inequalities since 2010
In 2008, a third policy review of health inequalities was commissioned, the Marmot Review. It was commissioned by a Labour government that was coming towards the end of its third term and was not enjoying public or media support. The government had also by this stage moved some way from its initial commitment to tackling the ‘upstream’ structural determinants of health, and was more focused on ‘downstream’ individual lifestyle factors. Within three months of being published in February 2010, a Conservative—Liberal Democrat coalition formed a new government. Indeed, the timing of the Marmot Review had ‘eerie echoes’ of the Black Report in the sense that it was commissioned under a Labour government but the decision to implement (or not) many of its recommendations had fallen to a Conservative-led government. Awareness of this political context may have influenced how the Marmot Review was drafted, possibly informing the decision to make rather vague and diluted recommendations that could be interpreted by, and remain acceptable to, different ideological perspectives, and thus avoid the political marginalisation that befell the Black Report in the 1980s. In addition, the international banking crisis and high levels of debt facing the UK meant that this was once again a period in which the government was committed to reducing public expenditure. It built on the earlier Black and Acheson Reports, although following 13 years of policy efforts to reduce health inequalities it had far more evidence on which to draw. Nevertheless, as Table 6.1 outlines, the Marmot Review’s policy recommendations largely mirror those of the earlier Black and Acheson Reports.
The coalition government accepted in principle the majority of the Marmot Review headline recommendations (all except the recommendations under heading 4, on income and poverty), and cited it as the basis for setting out a new public health system for England — in their 2011 White Paper Healthy lives, healthy people. This included the transfer of public health responsibilities from the NHS to local authorities with the establishment of Health and Wellbeing Boards (between, local authorities and local clinical commissioning groups [CCGs] of GPs), and the creation of a new organisation, Public Health England. In 2012, the government also created the Public Health Outcomes Framework, a set of indicators to monitor the new system that includes the aim of ‘reduced differences in life expectancy and healthy life expectancy between communities’. Under the new system, local authorities — via the Health and Wellbeing Boards were tasked with reducing health inequalities via actions on the local contextual and compositional determinants of health. This means that health inequalities and public health can now be ‘placed’ within broader local policies.
Public Health England was also created as a national body, and it has some responsibility for reducing health inequalities at the national level and between local communities. Its core mission is to ‘protect and improve the nation’s health and to address inequalities’. NHS England and CCGs, established under the Health and Social Care Act 2012, were also given a legal duty to reduce inequalities in access to — and outcomes from — NHS care. The Department of Health maintained a role in reducing health inequalities via its mandate with NHS England, and a framework agreement with Public Health England. The Secretary of State for Health is also required to ‘have regard to reducing health inequalities’. So now, in England, central government responsibilities for reducing health inequalities have been devolved to local authorities, the NHS and Public Health England, all of which have very limited powers to have an impact on the contextual or fundamental determinants of health (that is, the ‘rules of the game’).
In light of the new public health system set up by the coalition government in which local authorities have lead responsibility for reducing health inequalities, in 2014, Public Health England commissioned an independent inquiry to examine health inequalities specifically affecting the North of England, with a particular focus on how to reduce the North—South health divide in England (and, to a lesser extent, reducing inequalities in health within the towns and cities of the North), the Due North report. This concluded that the underlying causes of the North—South health divide in England and local health inequalities within Northern towns and cities were social, economic and political inequalities: differences in poverty, power and the resources needed for health; differences in exposure to health-damaging environments, such as poorer living and working conditions and unemployment; differences in the chronic disease and disability left by the historical legacy of heavy industry and its decline; and differences in opportunities to enjoy positive health factors and protective conditions that help maintain health, such as good quality early years education, economic and food security, control over life decisions, social support and feeling part of society. In order to tackle these root causes, the Inquiry set out four sets of recommendations (supported by evidence and analysis) to target inequalities both within the North and between the North and the rest of England. They focused on addressing:
(1) the economic and employment causes of health inequalities — calling for a regional strategy that ‘not only ameliorates the impact of poverty but also seeks to prevent poverty in the future, not least by investing in people, as well as investing in places’;
(2) the role of unequal early years in the development of health inequalities across the life course — calling for increased welfare support for families with children and for universal childcare;
(3) the need to share power over resources and to increase the influence that the public has on how resources are used to improve the determinants of health via the devolution of power within England; and
(4) strengthening the role of the health sector in promoting health equity as the NHS can influence health inequalities by providing equitable high quality healthcare, by directly influencing the social determinants of health through procurement and as an employer, and as a champion and facilitator that influences other sectors to take action to reduce inequalities in health.
Scotland, Wales and Northern Ireland maintained the pre-2010 NHS-based system with responsibility for reducing health inequalities lying solely with the healthcare sector — leading to increased divergence across the four UK countries in their approaches to health inequalities. In Labour-run Wales there has been little change, with a continuing focus on health promotion (as opposed to tackling health inequalities). Meanwhile, the restoration of powers to the Northern Ireland Assembly facilitated a fresh concern with public health, and a new Public Health Agency was established in 2009. The most significant developments, however, occurred in Scotland and England, where policies moved in very opposite directions. In SNP-governed Scotland (Scotland was led by a Labour-Liberal Democrat coalition from 1999 to 2007, and then the SNP from 2011), public health policy continued to articulate a social determinants approach to tackling health inequalities and that accepted the need for central government action. In contrast, the UK-wide Conservative and Liberal Democrat coalition government’s Public health White Paper for England paid little more than lip service to the wider social, economic, environmental and political determinants of health, choosing instead to stress that the causes of premature death are dominated by ‘diseases of lifestyle’ (compositional factors), for which the government accepts only limited responsibility. The lifestyle, individualised and very partial approach to health inequalities is continuing under the current majority Conservative UK government (elected in 2015).
What is to be done? Evidence-based health inequalities policy
So far this chapter has outlined how the UK governments from the 1980s onwards had an impact on health divides, showing a pattern of increasing inequalities despite (limited) action by the 1997-2010 Labour government. It has also alluded to what policy-makers and governments should do if they want to reduce health inequalities. However, this latter task is not reliant on mere speculation as the health inequalities reports commissioned by government agencies themselves over the last four decades — Black, Acheson, Marmot and Due North — provide an evidence base to underpin what could and should be done.
The four reports have much in common in terms of the explanations of the underlying causes of health inequalities: all four clearly state that health inequalities are a result of other societal inequalities and differences, and all take a ‘multi-causal’ approach to explaining their existence. Furthermore, they all emphasise the importance of considering determinants across the whole life course, not just the point at which health inequalities are most apparent, with emphasis placed on the early years of life. Indeed, the Marmot Review’s statement that it is the ‘cumulative effects of hazards and disadvantage through life’ that produce the social patterning of disease and ill health in the UK echoes almost precisely the Black Report’s conclusion that ‘inequalities in health tend to arise from the cumulative deprivation of a life-time’. Each places an emphasis on the social and economic (material) drivers of inequalities in health, although Acheson, Marmot and Due North — drawing on the wealth of health inequalities research undertaken since the 1980 Black Report – also highlight the complexity of the way in which material factors often interrelate with various other determinants, particularly psychosocial determinants.
The Black Report was published before psychosocial theories had emerged as a credible body of academic work, and hence, unsurprisingly, does not refer to psychosocial determinants. The Marmot Review and Due North both place considerable emphasis on psychosocial explanations of health inequalities, giving issues such as isolation, a sense of control and individual and community empowerment far more prominence than in the earlier reports. Due North, however, is much more materially (and psychosocially) focused than either Acheson or Marmot in that it overtly rejects the role of behavioural factors.
Despite the existence of some theoretical differences between the reports, as described above, and a gap of almost 35 years, many of the evidence-based policy recommendations are remarkably similar. This section provides a brief thematic comparison of the main recommendations.
- Early years and young people: For all four reports, the recommendations relating to early years bear striking similarities. While Black aimed for children to have ‘a better start in life’, with recommendations relating to increasing child benefits, improving pre-school childcare and providing free school meals, almost two decades later the Acheson Inquiry strongly echoed these recommendations. The Marmot Review is less directive, but as part of a policy objective to ‘give every child the best start in life’, various recommendations relating to maternal care, pre-school childcare and care within the education system are made. Similarly, the Due North report has ‘promote healthy development in early childhood’ as one of its four strategic recommendations.
- Education, training and employment: The Black Report and the Acheson Inquiry both focused largely on pre-school services so the Marmot Review recommendation that reducing inequalities in education outcomes should form a central part of efforts to reduce health inequalities could be said to represent a new focus. The Black Report featured no direct recommendation relating to employment either. In contrast, the Acheson Inquiry highlighted the detrimental effects of unemployment, and suggested increasing opportunities for work and training. The Marmot Review continued the strong emphasis on employment and training opportunities, but supplemented this with an emphasis on the quality and flexibility of employment. Likewise, the Due North report highlighted the need for employment opportunities to be increased within the North, and for good quality early years education proportionate to need.
- Working conditions/environment: The Black Report highlighted the need for ‘minimally acceptable and desirable conditions of work’. This was expanded by the Acheson Inquiry to include a call to address psychosocial work hazards. The Marmot Review further developed these concerns, placing particular emphasis on psychosocial-related issues such as equality and stress. All three of these national level reports recommend that the workplace be used an arena in which to undertake health-promoting activities. Due North does not talk about the work environment beyond a call for the living wage to be implemented.
- Tackling poverty and redistributing wealth and resources: The Black Report put forward the ambitious aim of abolishing child poverty as a national goal for the 1980s, although it acknowledged that this was likely to be very costly, and also included a number of other recommendations (particularly around benefits) that were intended to tackle poverty. Fast forward to 1998, and while Acheson did not recommend such an ambitious goal, it, too, emphasised the need to tackle income inequality, specifically recommending that: ‘Further steps should be taken to reduce income inequalities and improve living standards of poor households.’ This focus is echoed in the Marmot Review, which recommends the implementation of a more progressive taxation system and the introduction of a minimum income for healthy living. The latter is also recommended by the Due North report alongside tackling child poverty and introducing a living wage.
- Housing: All four reports call for an upgrading of housing stock. The Black Report focused on the quality and availability of local authority housing. The Acheson Inquiry added recommendations on fuel poverty and insulation and reducing accidents in homes, and placed particular emphasis on the housing of older people. The Marmot Review, less specifically, calls for the creation and development of ‘healthy and sustainable places and communities’, but in the longer term, it, too, calls for the ‘upgrade of housing stock’. Due North – reflecting the rising housing crisis in the UK – calls for a licensing scheme to improve private housing stock.
- The role of the NHS: All the reports stress the need for cross-departmental working at local and national levels of government. None of the reports suggest that the NHS can (or should) play a prominent role in addressing health inequalities, but the Black Report and Acheson Inquiry both make some recommendations concerning the need to ensure fair and equal access to healthcare services, and the Marmot Review suggests the ‘prevention and early detection of those conditions most strongly related to health inequalities’ should be prioritised. Due North highlights the importance of integrated local services and joint commissioning, and notes the role of higher funding allocations in deprived areas as a way of reducing mortality amenable to healthcare.
- Empowerment and community control: As noted earlier, the Black Report pre-dated research into health inequalities that emphasised the role of psychosocial factors. The Acheson Report made recommendations about control at work. However, in the Marmot Review, social capital, described as the ‘links that bind and connect people within and between communities’, is presented as a ‘source of resilience’ and ‘a buffer against risks of poor health’. Related to this, the phrase ‘capabilities’ is used throughout the report to help illustrate the importance the review places on enabling individuals to have the opportunity to live fair and healthy lives throughout their life course. Due North goes even further in terms of having one of its four strategic recommendations to ‘increase the influence that the public has on how resources are used to improve the determinants of health’. It has the devolution of power from central to local government and down to communities as a central theme of the report.
- Health behaviours: The first two reports also made some specific recommendations concerning the supply, marketing and consumption of tobacco products, whereas Marmot does not. None of the reports make similar recommendations for alcohol. In terms of diet and exercise, the Black relatively vague in suggesting that measures were required to ‘encourage the desirable changes in people exercise’. In contrast, Acheson made some rather specific recommendations, including increasing the availability of food to ensure the supply of ‘an adequate and affordable diet’. The Marmot Review is more similar to Black than Acheson, marking a return to relatively broad and unspecific suggestions such as ‘efforts to reduce the social gradient in obesity. Due North is very overt in rejecting the role of behavioural factors as an issue in the North—South health divide, and makes no recommendations in this area.
So these reports provide a clear policy agenda for what should be done to reduce health inequalities. However, as is clear in the review of actual policies from the 1980s outlined earlier in this chapter, the national policy effects of the reviews were minimal beyond leading to a welcome discourse around health inequalities. This is because good evidence alone does not lead to action — political support is required. The future politics of health divides in the UK and beyond is the subject of the final concluding, chapter.
The Health Divides website enables you to compare characteristics of local authority and regions with each other, and against England averages.
