Baseline integration
At last the government seems serious about pushing for health and social care integration in England. Integrated Care and Support: Our Shared Commitment[1], backed by a collaboration of national partners outlines a 5 year road map and pioneer areas are now beings selected. Integration will take place at a number of linked levels from overall macro commissioning, through workforce development and quality assurance to service redesign and the integration of services around the needs of individuals.
The baseline for integration will incorporate a range of changes including:
- Alignment – where commissioning intentions and the groups of staff from the different sectors work together on a daily basis. This may or may not be supported by the formation of joint teams under unified management.
- Process integration – for example, pooling of budgets at a macro or personal level, single health education and care plans, as in children’s services, and joint practice protocols.
- Service substitution – the implementation of integrated rapid reablement and emergency response teams that enable people to avoid having to be treated in hospital, or speed their discharge and produce better outcomes.
- Relocation – for example, the movement of acute services out into integrated community health and social care services so that they are delivered closer to where people live.
Putting co-production at the centre of integration
Making use of this full range of changes will make a big difference both to the service experience of people, their health and wellbeing as well as enabling much more efficient use of resources. However the agenda of the Collaboration requires us to go further by:
- Prevention – redesigning services so that ill health and functional impairment can be avoided, or where it occurs, be managed much more effectively leading to improvements in people’s quality of life as well as further savings.
- Broader focus on health and wellbeing – tackling those issues which are outside of the reach of both health and social care services that undermine people’s current health and wellbeing and others which can contribute to improved future health and wellbeing.
- Coproduction – engaging people in the planning and design of services, in assessing their own needs and deciding which treatments and supprts would best meet them. Co-delivering services in ways that that enable people make best use of, and further develop, their own strengths and assets and those of their local communities to improve the health and well-being of themselves and others. The Making It Real[2] ‘I’ statements spell out what co-production should look like from the point of view of people who us services and their carers. These statements have been incorporated into, and are central to, the National Commitment to Integration.
Implementing these elements of the agenda requires a radical change in perspective on integration:
- Looking beyond single conditions and social care tasks – it would be quite possible to pursue an integration agenda that focuses on set of integrations each targeting a specific long term health condition and its functional impact on people’s lives. A well-coordinated and integrated care pathway seems to be a no brainer. However the growing number of people who have 2 or more long term conditions would find themselves stretched across a set of pathways. Whilst each pathway would be integrated in itself, together the set of pathways required by any one individual would not. Hence people with multiple conditions would still face the extra burden of both making use of a number of separate sets of processes and having to integrate the advice and supports that each provides into their own lives. An alternative would be to adopt what NESTA[3] terms a ‘networked’ approach to using care pathways which redesigns them so that they can be drawn on in a coordinated way to meet the needs of different individuals.
- Broad service sector focus – the determinants of health and wellbeing require changes in many other aspects of the environment and people’s lives. For example having a job can produce a massive boost to a person’s mental wellbeing. Hence developing links between health, social care and employment services is critical. Integration will also require some service redesign. For example, free bus passes are of no use to older people unless the way buses are driven enables them to reach their seats safely. Parks are unattractive to people with learning disabilities if they become places where they are open to harassment. Left untackled these and other features of services can restrict people’s lives, undermine their health and lead them to becoming dependent on targeted services. Hence integration must, at its core, work across all parts of the public sector as well as the private sector including commercial services such as shops, cafes, pubs and financial services.
- Assets as well as needs – currently, at a strategic level, most Joint Strategic Needs Assessments and, at an individual level, most diagnoses and assessments, focus on what’s wrong i.e. people’s needs. These are important. However focusing solely on needs neglects what people can, and already do for themselves drawing on their own and their local communities’ strengths and assets. Focusing solely on needs leads to a reliance on organisational resources to meet needs and ignores the potential of complementing people’s own and their communities’ resources with those of organisations to further improve outcomes.
- Shared decision making – self-directed support in social care and ‘no decision without me’ and Choice in health[4] recognise the importance of taking into account people’s lived experience and involving them in jointly deciding what treatments and supprts would work for them. However the reality is that the power imbalances and the way diagnostic processes and assessments are structured reinforces a culture in which people are at best consulted but where professionals make the final decisions. The choices of treatments and supprts available are also constrained by those which are currently provided and the professionals’ conception of what is appropriate. This effectively rules out the ability of people to propose and access alternative approaches.
- Co-delivery – people and communities though their own actions have always had a major impact on their own and others’ health and wellbeing. However recognising this and building coproduction of outcomes into the redesign of services is still in its infancy. This means that people are currently not enabled to make best use of their own strengths and assets or develop them in ways which would be of greatest benefit to themselves and others. Similarly organisations are often unwittingly doing things that people would be happy to do for themselves whilst not providing the support that people might require to help them do so. This wastes everyone’s resources, undermines people’s ability to directly improve their own health and wellbeing and produces poorer outcomes.
Understanding the transformation
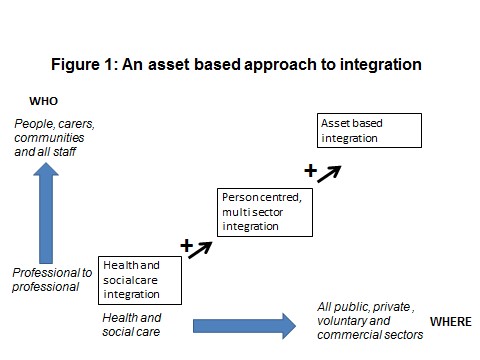
The change in perspective required is one that moves from a narrow health and social care ‘technical fix’ to one that puts the ‘coproduction of outcomes’ at the centre of the integration agenda. The journey involved in this change in perspective can be represented by three stages of development (See Figure 1).
Each stage incorporates the developments of the preceding stages and then adds further value by either extending their range or changing their focus:
Stage 1: Health and social care integration – organisation to organisation integration that aims to smooth out the connections required between health and social care commissioners and providers and the processes that they use. The focus is on achieving better service to service integration and staff utilisation. Whilst it is recognised that this will also bring benefits to people who use services this is not the major aim of the change. Typical changes include: joint commissioning intentions and teams; single care plans and integrated provider teams.
Stage 2: Personal centred multi sector integration – at this stage the focus on health and wellbeing and its determinants is broadened. At the same time the organisational focus widens from health and social care to include the roles played by the full range of public, voluntary and commercial organisations across all relevant sectors. Dementia friendly communities and the use of community budgets are examples of this stage of integration. Whilst, within this stage, people and communities and outcomes are the centre of integrations the focus is still on how to make best integrated use of organisational resources.
Stage 3: asset based integration – incorporates the developments from the previous two stages and then goes further by putting the role that people and communities are, and can play, in enabling health and wellbeing at the centre of all integrations. Organisational processes and services are redesigned to complement the existing and changed actions of individuals and communities. This includes rebalancing the power between, on the one hand professionals and on the other people and communities so that lived experience is given equal value alongside professional expertise. Investment is also made in community development. NESTA’s People Powered Health system level changes, OPM’s vision of an integrated approach to coproduction across health and social care and TLAP’s new programme focusing on enabling wellbeing through improved coproduction linked to community development are examples of this stage of integration.
Conclusion
The national collaboration puts the coproduction of health and wellbeing with people and communities at the centre of its vision for integration. If this is to happen the pioneers should be aiming to go much further than technical fixes. They should also move beyond the bounds of the health and social care sectors and embrace approaches that treat people and communities as equal coproducers of outcomes and rethink the use of organisational resources so that they complement and support the development and use of individuals’ and communities’ own assets.
Clive Miller, Associate, OPM, February 2014
[1] Integrated care and support: our share commitment, National collaboration for integrated care and support, May 2013
[2] Making It Real: marking progress toward personalised, community based support, Think Local, Act Personal Partnership, 2012
[3] Martha Hampson et.al, By us, for us, , People Powered Health project, NESTA 2013
[4] Vidhya Alakeson, Antonia Bunnin and Clive Miller, Coproduction of health and wellbeing outcomes: the new paradigm for effective health and social care, OPM April 2013