The NHS is a source of British pride. It is often described as “the envy of the world”. But what objective evidence exists to prove that belief?
It should be noted that comparing health systems is very difficult for a number of reasons. For instance, lifestyle differences influence how many people die of certain diseases. No definite conclusions can be drawn from the studies below. The World Health Organisation last attempted to rank health systems in 2000 (when France came 1st and the UK 18th), refusing to do so again because of the complexities involved.
How do health systems in other developed countries work?
Before we compare health systems, it’s worth comparing how they are organized.
The UK’s NHS uses what is known as a “single-payer” model – healthcare free at the point of use, funded out of taxation, and health workers are employees of the government. This arrangement is favored by many people on the left of the political spectrum. In recent years, single-payer systems in England and Sweden have made greater use of the private health sector to provide services, while keeping the services free.
Some of our European neighbors, including the Scandinavian nations, Italy and Spain, are also single-payer. But our closest neighbors – France, the Benelux countries, and Germany – follow the model the 19th-century German chancellor Bismarck established in his country in the late 1800s. Everyone (almost) is legally obliged to take out health insurance, which is provided by numerous competing non-profit insurers. The government regulates the insurance providers, to make sure they do not decline any applicant on grounds of health conditions, and provides subsidies for low earners. There is also less of a split between public and private health providers. A third of hospital beds in France are private non-profit or for-profit, according to the WHO, rising to almost 2/3rds in Germany.
Many Britons, either from the media or their own experiences, know something about the American health system. The American public debate about healthcare also means that most Americans know, or think they know, something about the British NHS. We usually think of the American system as being overwhelmingly private, but even before Obamacare was passed, about half of overall US spending on healthcare was by the federal government or state governments. The Medicare and Medicaid federal programmes cover the elderly and the poor, respectively, and the government also owns and runs hospitals for military veterans and Native Indians. The rest of the population is covered either by private insurance (often provided by employers), or do not have any health insurance.
Health outcomes: The UK and other developed countries compared
Survival rates, mortality statistics, and resources
The UK has a relatively poor record on treating cancer, although survival rates have improved hugely over the last few decades. OECD data shows that, out of 23 developed countries, the UK ranks 20th worst in bowel cancer 5-year survival rates. About 55% of Britons survive this time period: in Germany, over 64% do. The UK performs significantly better on treating breast cancer, but the data shows only 82% survive breast cancer for 5 years after diagnosis, while in Sweden over 87% do. The UK also doesn’t do well on measures of heart attack and stroke in-hospital mortality.
The UK has fewer hospital beds when compared to the size of the population. Germany has about 2 and a half times more hospital beds available adjusted for population size than the UK. In 2014, the Guardian reported that the only European country to have fewer hospital beds per head was Sweden. An OECD report from 2014 showed the UK has fewer doctors per person than any other western European country except Ireland, and relatively few MRI or CPR scanners per person.
The OECD study
In 2010, the OECD, a organization covering the world’s richest countries, published a lengthy report (UK summary here) which stated “The quantity and quality of[UK] health care services remain lower than the OECD average”.
The Commonwealth Fund study
The Commonwealth Fund is an US-based organization that “aims to promote a high performing health care system that achieves better access, improved quality, and greater efficiency, particularly for society’s most vulnerable, including low-income people, the uninsured, minority Americans, young children, and elderly adults” according to its website.
The CF’s 2010 report ranked the Netherlands first out of seven countries across a range of healthcare indicators, including efficiency, equity of treatment, access to care, and healthy lives. The UK ranked second.
In 2014, using data from a few years prior, the CF now found that the UK was the best healthcare system out of 11 countries, with Switzerland now second. The report was featured all across the British media, including in the Guardian, Independent and Telegraph.
Problems with the study
As the Institute of Economic Affairs explains here, the study had problems in it’s methodology. It gave more weighting to “inputs” than “outcomes”. In the “health lives” category – that measures health outcomes –the UK ranked second-to-last. It also favoured single-payer systems like the NHS, for example, paying over $1000 in medical expenses was seen as a bad thing by the study. Many would agree high medical bills are a bad thing, but it’s a matter of opinion. Another potential flaw is that, with the exception of the health outcomes category, the study relied almost entirely upon survey data. Questions about objectivity apply here.
This doesn’t mean the CF’s methods are wrong. They’re one way of measuring things, out of many ways of doing so.
The European Health Consumer Index
This study is published by the Health Powerhouse, an organization based in Sweden, describing it’s mission as “[to compare] healthcare systems among 35 countries, including all EU member states as well as Canada. “
The organization has published comparisons of European health services since 2005. The most recent one, from late 2013, showed the Netherlands as the best system out of all the European countries studied. England and Scotland ranked above average, though all of our geographical direct neighbors outperformed us, except Ireland. A press release stated: “The NHS urgently needs further reform if it is to match the services offered by Western Europe’s leading health systems.”
Problems with the study
It’s easy to observe that the Health powerhouse has a bias against single-payer systems. Just as the Commonwealth Fund has a bias towards single-payer healthcare, the EHCI appears to have one against it.
This doesn’t, however, impact the quality of the data. The EHCI makes more use of real-world data alongside surveys, so the problems of subjectivity that surveys bring are not as big an issue here. Official data is not always comparable, though.
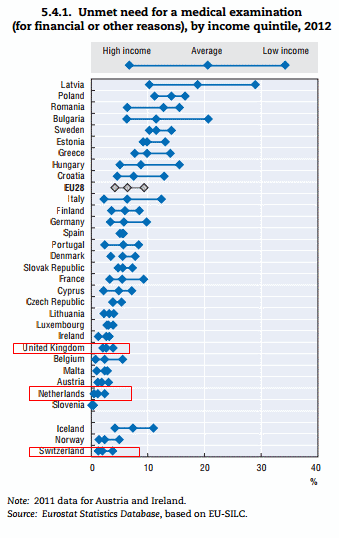
There are also flaws in some of the categories the study used. Health equity was determined by the proportion of health spending from public sources (taxation and social-insurance). But there are more useful measures of equity, like the one used in the 2014 OECD data below, on unmet medical needs:
How cost effective is the NHS?
NHS spending is just over 9% of GDP, which is just about average for developed countries. As a percentage of GDP, countries such as Finland, Ireland, Australia, Iceland and Italy spend less than the UK on health, while the US, Germany, France, the Netherlands, Canada, and Japan spend more.
Different studies have different answers on how cost effective the NHS is. The OECD 2010 study described above, in a complex model that looks at outcomes (infant mortality, life expectancy, and mortality amenable to healthcare) and tries to control for other differences between countries, said the UK was the 24th least efficient country of the 30 high-income states studied. The EHCI gave England and Scotland average “bang for your buck” scores – with, perhaps surprisingly, Albania coming top in this measure.
The Commonwealth Fund 2014 report said the NHS was the most cost-effective system of the 11 countries they looked at. A 2011 study found the NHS saved more lives per pound spent than any other country studied except Ireland.
Lastly, a analysis by Bloomberg, looking at life expectancy only, found the UK to be the 10th most efficient health system overall. The most efficient was Singapore.
Conclusion
In summary, little evidence seems to exist to prove the belief that the NHS is the “envy of the world”, at least if we are talking about the developed world. The UK’s health service surely provides adequate and often excellent care, but many questions remain about whether that care is as good as the standards of our cultural and physical neighbors in Europe and the rest of the world. The author believes that the British public deserves a rational debate about how best to finance, organize and provide healthcare in the UK today.