The need to defend the NHS and its core principles is so important that it is sometimes difficult to have conversations on the left about ways people can direct their own health care alongside supportive professionals. Ideas that stray from the need for more cash and more staff (both of which I think are needed) are often vehemently dismissed as at best naïve (dupes of the right, inadvertently opening doors to privatisation) or at worst evil (deliberately seeking to smash collectivism). It sometimes seems that to dismiss any innovation, all that is needed is to use one of the dog whistle words – consumer, market, private, top up, voucher etc. It feels like everything has to be presented as very simple – good or bad, right or wrong, market or state. This is not in the interests of people who use the NHS, and especially people with long term conditions. They need the left to be focussing strongly on how to maintain the core principles and elements of the NHS in ways which increasingly accept people as experts in themselves.
We sometimes seem to need a dilemma-free understanding of public services, where the interests of people who run them are seen as identical to those who use them. We can agree on the dangers of the uncaring market, but little attention is paid to the limitations that a bureaucratic state can place on users of public services. We seem to want to put our head in the sand and ignore, for example the kind of findings reported recently by the Institute for Public Policy Research:
“A 2010 Commonwealth Fund report compared seven developed-world healthcare systems and ranked the NHS top for effective care and efficiency, but bottom for patient centred care (Davis et al 2010). While this may matter less to those seeking one-off treatment for an acute health issue, it has a significant impact on people who have lifelong conditions that cannot be cured but only managed”.
My gentle plea is for us to have a better debate on the left, based on the need to focus first on the interests of people who use the health service and our understanding that power matters and needs to be shared. The Spirit of ’45 made me proud of our country – watching the NHS launched by Bevan at the hospital where my youngest was born. My parents were the first generation to benefit from the NHS and in later years were also employed by it – mum as a pharmacy stores manager and dad as a driver. I was also proud when my wife became a district nurse.
But in the final months of my mum’s life last year, our family saw both the best of the NHS and things that need to change – like a microcosm of the national strategic challenge. We saw fantastic GP support, great specialist cancer services and unbelievably supportive hospice care. We also saw insufficient community support (not enough district nursing and too few hours of home support via continuing health care). But this was not just an issue of insufficient resources in the wrong places, there were also problems related to a lack of shared decision making. My mum felt too powerless in the face of decisions made by systems that professionals felt they had to go along with and managers enacted.
Mum’s ability to control her support was first challenged when she qualified for fast track continuing health care at home. The professionals involved directly contracted with an agency (unknown to us) which phoned to say they were coming round that night. This despite mum (with family help) having already chosen an agency, met the staff and designed how she would be supported (who and how many people, when they would come, what they would do). Though this agency cost no more than the contracted one my mum’s decision to choose and direct her own care was seen as strange and it took quite a lot of negotiation to get agreement to keep the agency she selected.
A bigger issue arose as mum’s condition worsened. She had always been very clear that her worst nightmare was to die in a nursing home. Her view was that nursing homes were too institutional in how they operate and she wanted to be at home amongst family, friends and the familiar – be able to decide who came into her house, when and how they should support her. However, after she was admitted to the local hospice for some symptom relief, a move to a nursing home is exactly what would have happened if me and my sister hadn’t intervened forcefully. The senior consultant and other professionals felt it was best – partly given what they saw as the risks of her being at home but more importantly because this was what always happened. The PCT clearly had contracts with nursing homes and if you needed something different from three, one hour visits a day at home and a couple of nights, that is where you went. There was an attitude of “what is your mum’s problem with nursing homes” rather than an acceptance that she just didn’t want to go to one for her last days. It felt like most of the professionals were a little trapped in a “this is how we do things and how it has to be” culture. To their credit, after a lot of discussion the professional group listened to our ideas and agreed to a plan to get mum home and avoid nursing home. This was when we hit the final hurdle – the assessment disappeared into the vacuum of the PCT and never came out. Three weeks later mum died in the hospice.
I am not for a moment saying my mum’s care was poor – in the main it wasn’t. I’m not saying the professionals weren’t skilled and caring – they were. What I am saying is that she and those closest to her needed to be heard and responded to much more and that the problems with how the system worked weren’t just about the quantum of resource available.
There have been positive developments in recent years which give some people more of a say in their health care – self-management and shared decision making approaches . They have far to go before they are standard practice but are important elements of a continuum through which those who commission and provide health care can share decisions or “co-produce” (in the current jargon) with people using public services. For some, however, they won’t be enough. That is why we need to have, at the end of the continuum and for some people who choose it, the right to direct the resources for your care via personal health budgets.
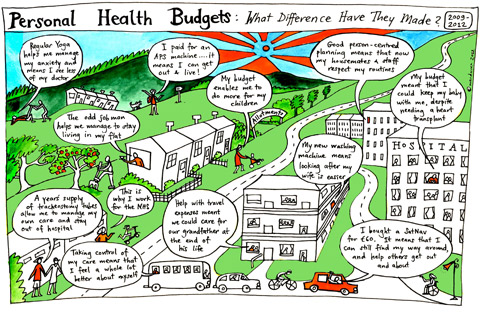
If my mum had been able to say “I want the resources available to me to be used in ways that I decide will work for me, though I am happy to hear your advice about managing risk and accept skilled professional support”, I am pretty confident she would have died where she wanted, at home. I have now met many people who love the NHS and would go to the barricades to defend its key principles who have found that using personal health budgets has allowed them or their loved ones to make their health support work for them when it wasn’t working before.
There are many arguments and understandable concerns about any system that monetarises care. Some of these are practical and technical – “how do you do this stuff?” Some of them are ideological and political – “is this opening the door to top-ups and insurance?”. All of these deserve debate – there are few powerful innovations without risks and potential downsides. It will be vital that personal health budgets are done well, that there are boundaries around the parts of the NHS they apply to, that they are not used as a trojan horse for the “selling off” of the NHS. But people on the left should engage in these debates seriously. We should consider how real and enduring problems in how people with mental health needs and other long term conditions are currently served might be positively impacted upon by personal health budgets.
Currently there is too much angry polemic, sometimes almost contempt for those (including “patients”) who are advocating for personal health budgets. Their detailed stories of how personal budgets have allowed them to have greater control over their care and improve outcomes are too easily dismissed as anecdotes rather than “data with soul”. When people do look at research evidence they seem to be looking for cold fusion – a perfect, dilemma-free innovation – or they point to the things that the research hasn’t yet found out as the key reasons PHBs are a bad idea. It is not helpful to dismiss a three-year independent academic trial with a control group as worthless evidence as some have done. It sheds heat not light to use the somewhat flawed experiment in the Netherlands – where personal budgets were so popular that the system buckled – as proof that PHBs are a bad idea. It is certainly a strange argument on the left to say in effect “too many people wanted to control their care – we musn’t allow that to happen here”. We might as well have said in 1948 “too many people are getting their eyes checked and teeth fixed – stop it now!”
I want to see an NHS that is properly funded and offers great health care. I also want to see an NHS that increasingly acknowledges that people and families are experts in themselves and should have a much stronger say over their care if they want that. Money on its own won’t solve this. It is really instructive that many disabled people are very anxious about proposals to integrate health and social care within a health-led system. They fought in social care for the social model of disability (a battle far from won) and fear the return of the medical model into their support. People like the idea of joined up support very much, but not the idea of integration being done to them via systems and practices they have no real influence over. Disabled people fought a decade’s long campaign for direct payments because they knew that however well intentioned, the interests of the system and the professionals staffing it are not simply identical to their own. They knew that in some cases they needed the power to be able to say “I know you think that is best for me and I respect your professional judgement but I also need to be heard and want the resources for my care spent in ways agreed with me”.
Often people sympathetic to these arguments but wary of making resources directly available say “It’s true we need to be more person centred but we don’t need personal budgets for that, it’s about culture change and using some of the new approaches and practices”. I hope that we can continue to make culture shifts and adopt new power-sharing methods. At the end of the day though for some people to be heard and while we are waiting for these culture changes (its taking a while), some will want and should have the option to use personal budgets to direct the resources for their care. I respect that others on the left have different views but let’s talk about it. As Mrs Merton wouldn’t have said, “let’s have a slightly less heated debate.”
(The views in this blog are my personal opinions and should not be taken to represent those of my employer)
