What is rationing / priority setting?
Rationing and priority setting are referred to somewhat interchangeably within the literature, with little focus on the actual terminology, and more upon the outcome of priority setting and its impact upon healthcare. Priority setting, “a more or less systematic approach to distributing the available resources among demands”, can lead to rationing of care, defined as “a failure to offer care, or the denial of care, from which patients would benefit”. Rationing can also be defined as any form, either implicitly or explicitly, of allowing people to “go without beneficial services” due to constrained costs.
A more identifiable form of rationing involves denial of treatment due to cost-ineffectiveness –although not adequate in the eyes of the public – as opposed to rationing where there is a shortage of medical staff at a particular moment in time. There is also rationing by waiting or delays in treatment, which appears as less visible than complete denial of treatment. Whilst all forms of rationing might not impact care, there is an issue of transparency of the healthcare service provided. Only if there is acknowledgment of rationing therefore, can “fair and reasonable priorities and standards be established”.
The role of priority setting and rationing within the NHS
Published in 2009, the NHS Constitution defines the NHS as providing a “comprehensive service”, but has not actually set out what the NHS does and does not provide. Given that the NHS in England is publicly funded with a multibillion-pound budget, it is inevitable that some form of priority setting based on economic grounds will be made, which, although largely denied by the Department of Health, is highlighted to a greater extent during times of fiscal pressure. Whilst the Department of Health is accused of being in “official denial that cost-motivated rationing is taking place”, there is ample evidence to suggest otherwise. For instance, the NHS has often “rationed with waiting lists”.
The National Institute for Health and Care Excellence (NICE) is the Non Departmental Public Body responsible for providing guidelines for the use of new medicine and treatments. For the purpose of this paper, NICE is arguably the most important aspect of healthcare in England due to both the praise and criticism that the organization receives, and can be described as a “finely tuned machine”. NICE’s influence within the NHS can be demonstrated by the list of “do not do” clinical interventions, ranging from only using major surgery as a last resort, to the use of vitamins in reducing cardiovascular risks. Additionally NICE can be described as “doing the Oregon for the NHS on a day-to-day basis”.
The current service, or “package of benefits”, funded by the NHS is “arrived at implicitly through the decisions of…politicians, regulators, commissioners, clinicians and patients” on a local level across the NHS, through PCTs. Such a process has the potential to lead to a variation in the service that is provided across England, and contributes to the notion of a postcode lottery, or “rationing by postcode.”
Such a postcode lottery therefore does appear to show a need for standardisation of priority setting from a PCT perspective, which could theoretically allow a more balanced level of healthcare to be provided. The most notable political response to the notion of a postcode lottery is the establishing of NICE itself by the Blair government “to develop national service frameworks” to deplete such a variation in care.
Whilst the postcode lottery can be attributed to the autonomy that each PCT has, one not entirely negative aspect of the disparity is that the NHS services in poorer areas do not appear to be disproportionately affected.
Regardless of whether such a lottery actually exists or not, it is necessary to look at the issue of priority setting further within the NHS. For instance, a report in 2007 found that 53% of doctors knew of cases where patients had suffered due to rationing of their healthcare. Additionally, 85% of GPs believe that “in the next 5 years the NHS will have to set out …what is – and what is not – available to patients” in the NHS.
The public will often show strong support for the NHS, but given some of the reaction to NICE decisions, there is not necessarily a connection made by the public to the limits of the NHS budget. One survey did however find that 61% of people surveyed believed that the “NHS will have to stop providing some treatments and services in the future due to rising costs and increased demand”. The same percentage also said it was “right that some hospitals stop providing certain services in order for the NHS to save money”.
Whilst there is little evidence of complete consensus on whether priority setting and rationing is occurring within the NHS, the use of terminology is varied within PCTs, perhaps making it difficult for national surveys to have full validity. For example, terms such as “Procedures of Low/Limited Clinical Value” and “Interventions Not Normally Funded” are used in an apparent attempt to avoid the association of priority setting or rationing.
An example of priority setting within the NHS is found at Croydon PCT where “34 low-priority procedures of ‘limited clinical value’” have been earmarked under four categories, from relatively ineffective to effective interventions. An important point to consider here is that priority setting processes adopted by other PCTs appear to have focussed upon new funding and developments, rather than existing funding too. Such a focus is also a criticism of NICE, and as will be discussed in Chapter 2, is in direct contradiction to the other approaches taken.
An argument can be made that the public should have as much information as possible about the way in which funds are spent in the NHS. Given the importance of healthcare to one’s own life, it is of utmost importance that any priority setting made in the NHS is explicit.
Discussing the role of priority setting is important because it can lead to variations in the level of care available, especially if left up to the PCTs to decide, as was shown with eligibility of IVF treatment. Given that a survey of PCTs found that 45% made public the criteria used by priority setting panels, and 44% made such decisions public, there is visible reluctance from some PCTs to engage with the public about priority setting and rationing.
The processes the NHS uses for determining what services to provide can be regarded as “obscure and lacking in accountability” to patients. An argument in support of a more transparent decision-making process for priority setting is that if “decision makers were encouraged to make their decision-making processes and decisions public, it would help to guard against inconsistency, unjust preferences and groundless exceptions”, and therefore theoretically leading to a more transparent NHS. Whether this necessarily leads to more accessible care – arguably more important than the transparency of the PCT – remains to be seen, however.
The politics of rationing/priority setting
Whilst the argument can be made that rationing is an “inherent feature” of the NHS, political leaders do not choose to talk about the NHS in such terms, due to the political sensitivity of the NHS and the political consequences that talking negatively about a well-respected public institution can have. It is common for ministers to occasionally “define what should be provided (for which they can claim credit) but will almost never explicitly decide what should not be provided (which might attract blame)”. The consequences for such an approach is discussed in the analysis and lessons for the NHS that can be taken away from the Oregon Health Plan.
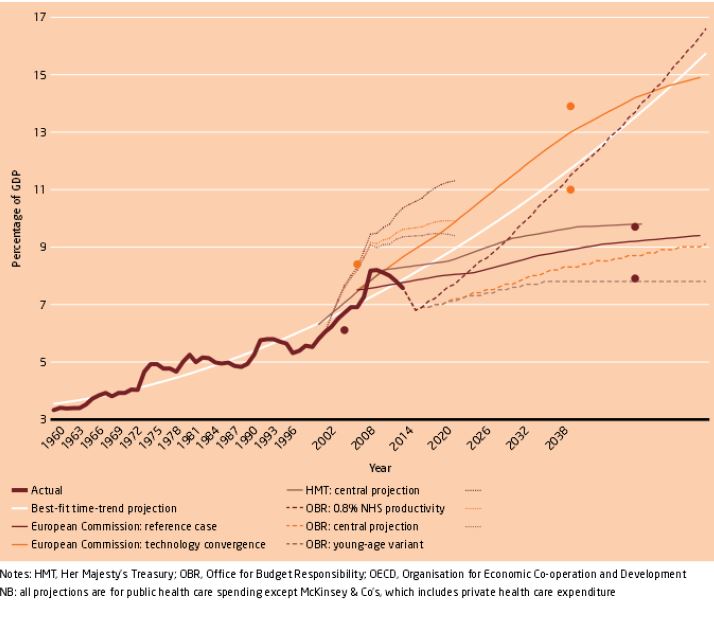
In addition, as the NHS budget comes under more pressure, the “willingness” of political leaders to engage with priority setting may diminish, particularly if this leads to unpopular decisions. The existence of NICE has however led to some distance “from decisions that risked attracting criticism” between policymakers and healthcare provided.
Ian has been working with us for the last year and this is part of his undergraduate dissertation submitted to the University of Sheffield.
