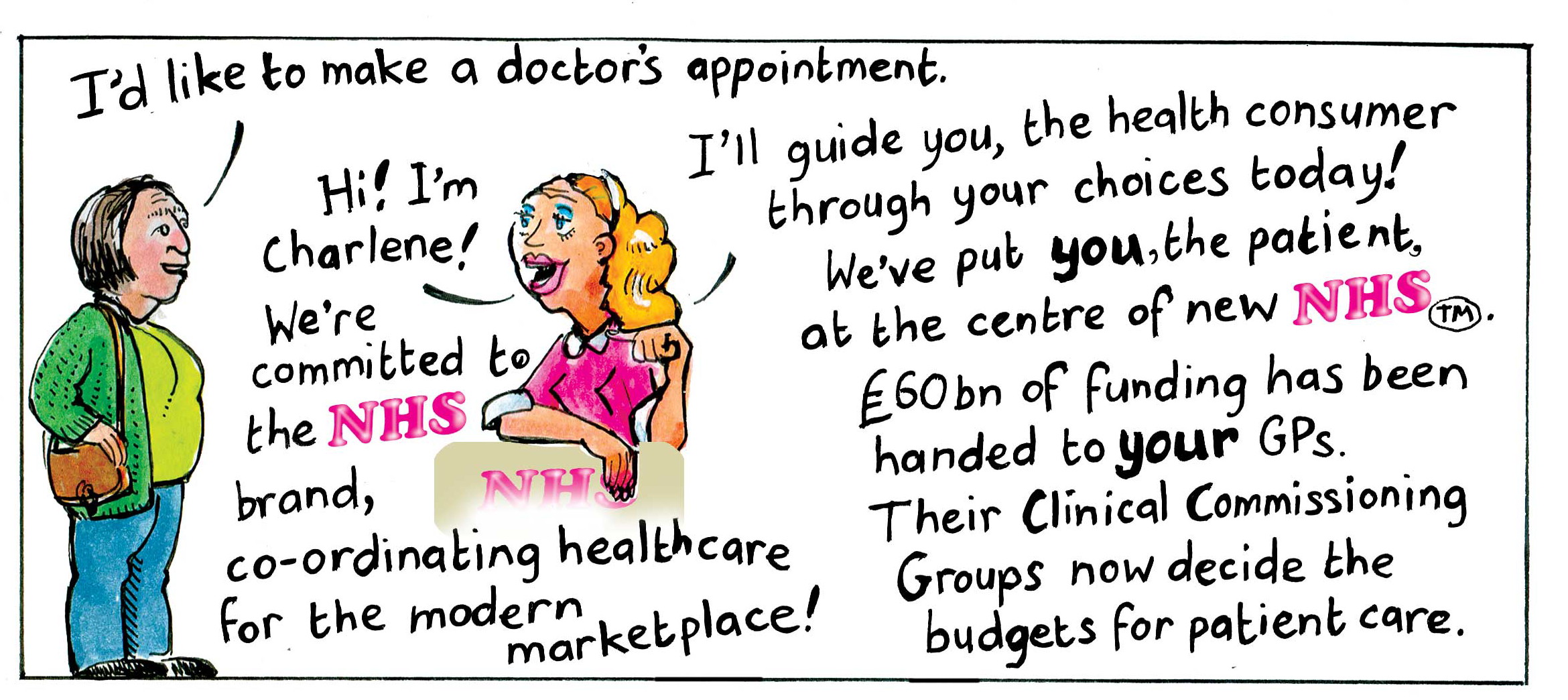
From 1 April the NHS moves into a new form. The NHS ceases to be the provider of healthcare and becomes just the commissioner; the Secretary of State ceases to have any meaningful responsibility and no longer has powers to direct and intervene, strategy and planning are replaced by market forces. A greater range of providers – some from the private sector, will be delivering NHS care.
As we have argued for almost 3 years the intention is to make a regulated market for our healthcare. We are convinced that this is but the first step in a process which inevitably leads to a different NHS with user charges, top up payments, queue jumping and with vouchers or personal budgets being used to pay for services in a proper market. Such an NHS will fuel inequality and destroy an institution which tried hard to encapsulate the principle that we are stronger together striving for social justice.
To help weaken opposition to this ideological shift there is now a concerted campaign to denigrate the NHS. It is far from perfect and there have been instances of poor and even appalling care, and some parts remain stubbornly inefficient, but the last thing the NHS needed was spending £2bn on a pointless reorganisation. There is ample evidence of the improvement trajectory and in most international comparative studies of efficiency or outcomes the NHS is up there with the best.
The likelihood is that users of the NHS will not notice any difference on 1 April, or indeed any time soon thereafter. The hospitals and GP surgeries will be just the same, prescriptions will be dispensed as always, waiting times may edge upwards but would anyone notice? Where, over time, new non NHS providers are used they may or may not be seen as giving better service. We know that people get very excited and angry if they fear their local facilities are to be shut down or if there is some perception of unfair post code lottery restrictions. But the evidence appears to be that few care who manages the service.
The workshops the SHA has been running around defending the NHS have shown how difficult it is to actually define what the NHS is. Perceptions of the NHS, what makes it good and what limitations it has are often misguided. But there is still a tremendous affection and pride from most of us directed towards what we see as one of the great national institutions. We know our NHS is free at the point of use paid for out of taxation and that it is both universal and comprehensive. Each part of that will come under gradual but increasing challenge.
Many other countries have health systems which are also free, universal and comprehensive but they take different forms and they all face a period of great challenge. Put simply the cost of providing care to the quality levels people increasingly expect is rising faster than GDP or even (perhaps) willingness to pay for it.
When the era of austerity began various attempts were made to look at the gap between the likely cost increases within the NHS and the assumed level of funding – no real terms increase. Since historically NHS funding has risen around 4% above the rate of inflation the impact had to be huge. This is the “Nicholson Challenge” – the £20bn; it is simply a measure of the gap over a four year period between the cost of delivering the NHS in its current form and the money available to pay for that.
Something radical does have to change; we do need a different NHS. Dealing with the funding gap by increasing efficiency is a task almost certainly beyond the capability of the NHS we know and the current organisational changes are likely to make things harder.
The NHS in England has gone from being an unmanaged service to one with some aspects of organisational management, to a quasi market (commissioner/provider split) and now to a regulated real market.
Within the SHA we reject the market/competition model and are continuing to develop our policies about a different kind of care service, based on whole person care. We are looking at ideas around accountability and opening up NHS information; viewing patients and communities as assets not as problems; using better service planning, cooperation and integration as drivers of improvement. We want to change
Until we get a government committed to our kind of care service we have to do all we can to slow down and inhibit the worst impact of the coalition NHS denigration and destruction policy.
