I INTRODUCTION
I am greatly flattered to be invited to deliver the 1998 annual lecture of the Office of Health Economics, partly on account of my distinguished predecessors, but also because this invitation provides an opportunity for a more explicitly historical perspective than is usual on these occasions. This year of the fiftieth anniversary of the National Health Service(NHS) is an especially appropriate opportunity for such an exercise.
Building on the important insights provided by Sir Douglas Black who, in the 1994 OHE Annual Lecture,1 alluded to the fallibility of the reorganisation process, in this lecture I would like to turn the historical spotlight on the phenomenon of NHS reorganisation. As Professor Reinhardt reminded us in the 1997 OHE Annual Lecture,2 growing insecurity about the condition of our health services represents a global problem. He rightly points out that our anxieties stem from the anomalous economic characteristics of our transactions relating to health care, which resolutely refuse to be ordered according to the formulae applied with success to other parts of the economy. According to this account, even the most successful western economies have lapsed into a seemingly permanent malaise about their health care systems. Professor Reinhardt sees confirmation for this malaise in the ‘periodic calls for bold reforms that are followed periodically by feeble attempts at reform, only to be followed by further calls for reform’. At any one time, some task force or other is likely to be at work finding its way out of this labyrinth, but on the basis of the record of contemporary history, he understandably expects that these efforts are likely to end in frustration.
For most of the life of the health service, reorganisation has been high on the political agenda. There could be no better reminder of the salience of this issue than the production of the three national White Papers, on NHS reorganisation in England, Scotland, and Wales, by the Labour government, only a few months after its return to office.3 My main purpose in this lecture is to suggest, however, that the NHS has not always been assisted by the haphazard nature of political intervention over health service reorganisation.4 I will argue that we are unlikely to extricate ourselves from the dilemmas outlined so compellingly by Professor Reinhardt unless we take steps to elevate decision-making to a higher plane of rationality. On account of its state-funded and unified nature, the NHS is particularly exposed to the vagaries of gratuitous political interference. On the other hand, these same factors offer great prospect of rapid improvement of the entire system if politicians’ judgement is exercised using the best available evidence. On the basis of this case study involving the cluster of important policy issues associated with reorganisation, I will offer some tentative suggestions about a possible means to improve the quality of political decision-making about the NHS.
The basic chronology of change in the UK health care system is self-evidently a story of sharp contrasts, and it presents a major paradox. As comprehensively chronicled in the recent book by Geoffrey Rivett , biomedical research and its technical application represents a cumulative, accelerating and in many respects inspiring record of achievement, which has inevitably fuelled progressively higher levels of aspiration. On the other hand, the translation of these innovations into a viable and effective system of health care has constituted a faltering and accident-prone process. Failure of the health care system to respond to changing demands and expanding aspirations has inevitably produced a high level of anxiety concerning the adequacy of our health service. In this respect the UK is participating in a problem that is shared by the entire western world. For better or worse, the centralised character of our health service and the politicised character of the decision-making process have thrown our problems into sharper relief than in the predominantly decentralised and insurance-based systems prevalent among our neighbours. Since major structural overhauls have featured as one of the predominant responses to particularly acute moments of crisis, I would suggest that evidence concerning reorganisation exercises provides one of the most sensitive indicators of the state of the health care system.
A brief glance at the chronology of reorganisation of health care in Britain confirms the sense of gathering insecurity about the system. Even superficial inspection indicates that the interval between major reorganisations has been progressively diminishing. The administrative system bequeathed by Lloyd George after 1911 persisted for 37 years. Bevan’s new health service lasted for 26 years. Even with the correctives introduced in 1982, the Joseph reorganisation, of 1974 survived for only 17 years, while the internal market changes of 1991 are about to be radically altered after only about 7 years. Indeed, the 1990s will have witnessed almost incessant structural change. Historians of the future will recognise this decade as the period of greatest structural instability for health care in Britain in the course of the present century. The optimist will regard this as indicative of a healthy spirit of innovation and progressive problem solving; others will adopt a more pessimistic interpretation, and detect dangers of infinite regress.
II FIFTY YEARS AGO
With good reason, the establishment of the NHS is regarded as a major turning point against which all later change is assessed. Consequently, it is not at all surprising that the Labour government’s recent White Paper, The New NHS, implicitly adopts the 1948 model as its point of reference, even to the extent of taking its main title from the heading of the house-to-house leaflet distributed exactly fifty years ago to explain the benefits offered by the new health service. A photographic illustration of the title page of the house-to-house leaflet is granted a place of honour as the first illustration in the White Paper, taking precedence over the photograph of the Prime Minister in the Foreword.6
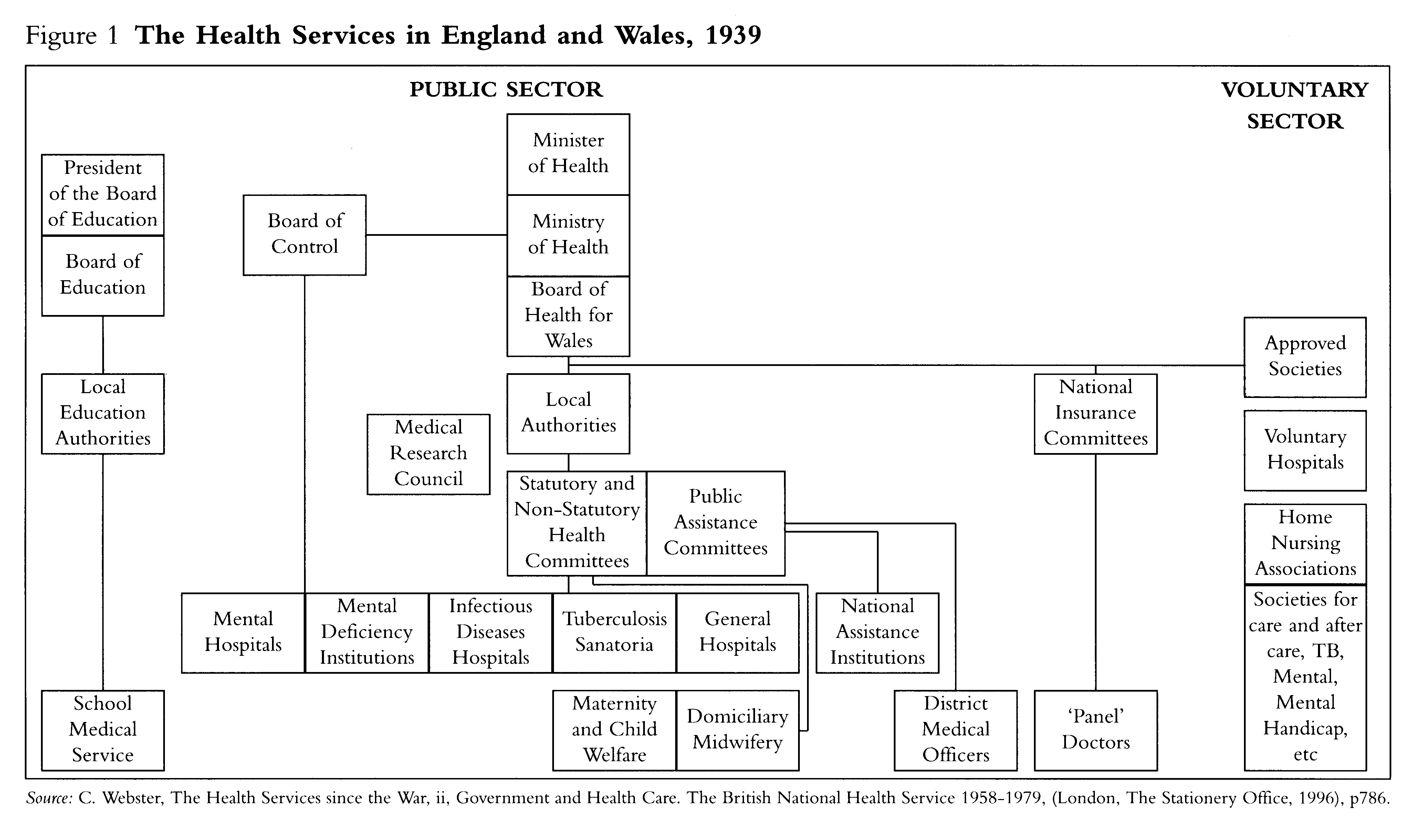
Allowing for the unfavourable circumstances existing at the time, it is possible to treat shortcomings of the planning operation at the outset of the health service with some indulgence. Aneurin Bevan deserves huge credit for turning an almost impossible situation to advantage. From the perspective of the 1990s, the mix of public and charitable providers existing before the NHS (indicated in summary form in Figure 1) might be regarded as an inspired anticipation of the internal market. However, at the time these market arrangements seemed the embodiment of inefficient utilisation of scarce resources. It was universally accepted that creation of a comprehensive and modernised health service required a substantial element of administrative integration and imposition of planning on a scale never before regarded as practicable. This conclusion reflected the approach to social and economic planning popularly associated with the names of Keynes and Beveridge, which was conducive to bold planning initiatives of a kind that had had been out of place at an earlier date. This latter factor accounted for the persistently negative response by government to the ambitious proposals for a comprehensive health service contained in the Dawson Report of 1920.7
Intractable medico-realities stood in the path of enlightened planning goals. After years of futile wrangling bet-ween the vested interests, the health service was no nearer to realisation in 1945 than at the beginning of the war when planning had first begun. The Labour Party, the local government associations, and the Ministry of Health had not helped the situation by clinging on to their longstanding objective of placing the new health service under the existing form of local government administration. This was unrealistic, not only on account of the unsuitability of local government structure and the local taxation system, but also because this proposal was unpalatable to the medical profession. Ever since the beginning of the century, general practitioners in particular had bitterly resisted the prospect of becoming full-time, salaried employees of local government, working under the authority of the Medical Officer of Health for the locality. The resurfacing of the idea of salaried employment in the context of proposals for a national health service alienated the medical profession to such an extent that it took more than a generation for their hostility to subside.
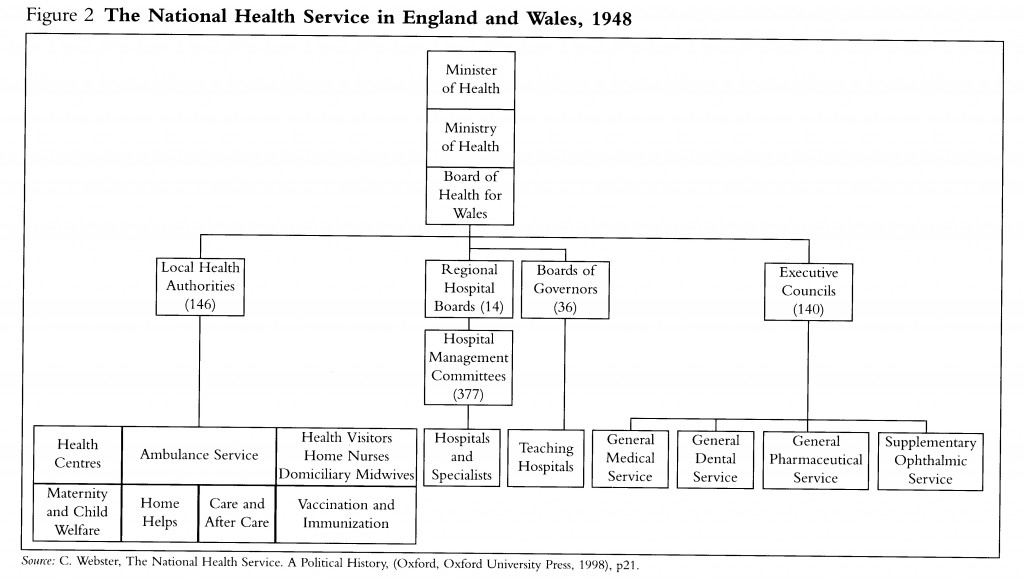
The Attlee government was under pressure to make rapid strides to realise its reformist objectives. The public would have been unforgiving of any repeat of the policy failures, including total inaction over the Dawson Report, that had occurred after the First World War. Owing to his joint responsibilities for housing, local government and health, Bevan occupied the frontline of the government’s social programme. His plans were evolved with remarkable speed; indeed, his health service scheme seems to have been formulated within a few weeks of taking office. Success in the accomplishment of this mission was predicated on a decisive break with the ill-fated wartime planning exercises. This entailed, however, a significant cost – the abandonment of the administrative unification of health services at the local level. As indicated by Figure 2, local authority clinic and independent contractor services were in essence frozen under their pre-1948 forms of administration. This concession was particularly helpful in circumventing a potentially disastrous confrontation with the BMA, thereby enabling Bevan to concentrate on the main innovation of his scheme, the nationalisation of all municipal and voluntary hospitals to create a unified regional hospital system. Bevan’s choice of nationalisation and regionalisation certainly went against the grain of thinking among the dominant health service interests of the time. On the other hand, Bevan’s solution was consistent with the thinking of the best-informed and innovative leaders of the medical profession and with many leading theorists on the financing and reform of local government. This trend in thinking was for instance reflected in the columns of The Economist, which throughout the war years consistently advocated the unification of the hospital system under state control and outside local government. Although seeming to operate impetuously and on the basis of personal inspiration, Bevan was arguably drawing on the best-argued and most appropriate alternative available within the expert literature of his day8. Bevan may have been responding impressionistically, but it is likely that a more deliberate act of policy assessment would have resulted in the same conclusion.
Both independent contractors and local authorities greatly extended their functions under the new health service. However, its strengths rested on success in establishing comprehensive consultant and specialist services. Although in the 1980s, Bevan’s regionalised hospital system came under a shadow on account of the unpopularity of its so-called command and control management system, it was a remarkable improvement on the chaotic market arrangements that had existed before the Second World War. Despite evident shortcomings in the new system and the handicap of an environment of severe austerity, the regional hospital service succeeded in keeping up with the demands of modernisation and recorded impressive increases in output. On account of this firm record of achievement, despite all of its idiosyncrasies, Bevan’s health service fully deserves the positive image by which it is remembered.
III THE 1974 REORGANISATION
From our present perspective, it is scarcely credible that such an unsatisfactory result as the 1974 reorganisation should have emanated from a lengthy planning exercise. Whereas Bevan had no choice but to arrive at his ambitious plan within the space of a few weeks, the much lesser reform of 1974 was the result of a leisurely exercise extending from at least 1966, a period in excess of eight years. The deliberations were shared almost equally between Wilson’s Labour and Heath’s Conservative administrations. Taking England and Wales together and including one suppressed White Paper; no fewer than eight major policy documents on health service reorganisation were produced between 1968 and 1972. Accordingly, in this instance, the assets of time were squandered in the course of a lengthy and futile attempt to appease all the relevant interest groups. This was a repeat of the process of horse-trading that had occurred during the Second World War, and which had created such disarray on the eve of the return of the 1945 Labour government. On this occasion there was no Bevan to exercise decisive influence in favour of an effective and realistic solution. The politicians drifted from one unsustainable policy to another according to the balance of pressures reaching them. It is striking that, despite the fashion for expert enquires at this time and calls for such a committee to investigate this problem, at no stage was this course of action seriously considered. The existing central machinery for taking expert advice was not actively involved in discussions of policy concerning reorganisation. Given this unsystematic and haphazard approach, it is perhaps scarcely surprising that an unsatisfactory conclusion was reached.
The record of failure to engage meaningfully with reorganisation was even worse than indicated above, since this had been a live issue since 1962, owing to its promotion by the Porritt Report, produced by a group of medical experts representing nine leading medical organisations.9 The reorganisation exercise also enjoyed the advantages of the learning experience offered by the first twenty years of the new health service, the growth of expertise in the fields of health service management and health economics, and finally, access to the findings of a variety of expert committees investigating problems having some bearing on reorganisation. The most authoritative of the latter were the Royal Commissions on medical education and local government and the Seebohm Committee on personal social services, all of which were established in 1965. The final reports or at least the provisional findings of these committees were available to the authors of the first Green Paper on health service reorganisation published in 1968.10
As in the case of the reform of local government, the personal social services, and medical education, other expert committees of the period insisted that their objectives would be better achieved if the three strands of the health services (the hospital, local authority, and family practitioner services) were unified. Accordingly, NHS reorganisation of some kind became regarded as an inevitability, if only as a defensive measure. By the mid-sixties, there was also a growing consensus that unification of health service administration was essential on grounds of economy, efficiency, and effectiveness. By this stage, practical progress on many policy fronts, such as the development of integrated health services in new towns, was impeded by continuation of the existing fragmented system, which perpetuated the failings of lack of integration that had afflicted the pre-war market system.
The ideal of unifying the administration of all publicly provided health services in any one natural area under a single system of administration had been an aspiration of most leading thinkers ever since the Royal Sanitary Commission of 1871. This goal was broadly adopted, but had in succession defeated such major luminaries as Sir John Simon, Sidney and Beatrice Webb, Sir Robert Morant, Lord Dawson of Penn, as well as the wartime NHS planners, and finally Bevan himself in 1948.
The ideal of unification was supported by a consensus, but agreement on the way forward ended at this point. It is now largely forgotten that the main problem facing the planners related to the relationship between the health service and local government. Unification of the health services under local government was a paramount objective in the century before 1948. Even after establishment of the NHS, it was widely accepted that the 1948 arrangements were a temporary expedient pending local government reform. It is therefore not surprising that the idea of reintegrating the health services with local government should again become a live issue when local government reform returned to the political agenda. The late sixties may well turn out to have been the final occasion upon which this policy option was accorded serious consideration. There were indeed well grounded objections to this proposal, but it was no more objectionable than rival policies that have continued to be regarded as viable options and remain on the policy agenda. The elimination of the local government option therefore relates more to ideological change than to the merits of the case. Indicative of the huge cultural change that has occurred since 1974, it is now virtually inconceivable that any role for local government would be considered in the administration and management of the health service.
Within the health service there was deadlock concerning two alternative routes to reorganisation. The two-tier, region: district model was the preferred option within the hospital sector. This possessed the advantage of natural evolution from the regional system of hospital management introduced by Bevan. The alternative was the single-tier area system favoured by the family practitioner and community care lobbies. This accorded more with traditional aspirations about ‘unitary authorities’ as the basis for health service and local government reform.
The above issues by no means exhausted the areas of contention upon which opinion was evenly divided. The Treasury for instance actively canvassed the need for a top down management structure, which was at odds with demands from elsewhere for greater local accountability or for consensus management. Also the Treasury believed that efficiency in the use of resources demanded full assimilation of the family practitioner services into the integrated health authorities. This was actively resisted by the family practitioners themselves, partly on grounds of their long-standing antipathy to erosion of their status as independent contractors. Other groups, such as the long-term care specialties, or public health doctors, were also fearful about their futures under reorganisation. The reorganisation mission was therefore bristling with opportunities for confrontation, and open to the real danger that the outcome would represent an insufficient improvement on Bevan’s system for the exercise to have been justified.
It is interesting that on this occasion the reorganisation initiative emanated from the medical profession rather than the health departments. The Ministry of Health noticeably failed either to appreciate the strength of the case for reorganisation, or to take effective command of the situation when this case was conceded. When shaken into action, the Ministry adopted the Porritt model, which embodied the single-tier solution -widely favoured within the BMA, which was in fact the filial descendent of the scheme contained in the 1920 Dawson Report. Naturally, the Porritt plan decisively rejected association with local government, and indeed assumed that all existing local government social services would be annexed under its proposed area health boards, which was diametrical opposed to the course proposed for unification of the social services by the Seebohm committee. The Ministry prepared its first Green Paper on reorganisation without enthusiasm, in conditions of secrecy and with no ‘outside’ consultations, even with expert bodies within the standing advisory machinery. Although slavishly following the Porritt model, the first Green Paper issued in July 1968 carried little conviction, and it won support neither within the medical profession nor elsewhere. 11
The next phase of the planning exercise was undertaken under Richard Crossman. This marked a complete reversal of approach, involving frenetic and almost indiscriminate consultations conducted in a highly personal manner by the Secretary of State himself. As the diaries of Crossman testify, this process was associated with many changes of direction. With his customary self-confidence, Crossman initially believed that casting aside the Porritt model and reverting to the region:district scheme could readily solve the reorganisation conundrum. Indeed the latter carried greater support within his department, but in practice relations with local government precluded elimination of the area tier. Crossman was therefore driven into retreat, and was obliged to restore the area to a place of prominence as a statutory authority. However, interposing the area would have resulted in a three-tier hierarchy, which was regarded as unworkable. In order to avoid this complication he decided to sacrifice the region, but once again ran into opposition, especially from the entrenched regional authorities. Crossman left office before this problem was resolved, but he was well on the way to conceding defeat and sanctioning a three-tier system. At this stage Crossman’s self-confidence finally collapsed; he concluded that his whole approach to reorganisation had been mistaken, although he predictably blamed his officials for this outcome.12
Since the expectation was aroused that local government and the health service -would be reorganised simultaneously in 1974, time was running out for Sir Keith Joseph when he assumed office under the Heath administration in the spring of 1970. Joseph’s scepticism about the justification for reorganisation compounded this problem. Joseph’s consultative document was not issued until May 1971, and even this was self-evidently an over-hasty production. Given the pressure of time and absence of agreement on the way forward, Joseph was persuaded to accept the three-tier plan embracing region, area and district. This largely represented the state of thinking reached under his predecessor. A scheme entailing combining all previous alternatives was designed to appease all vested interests, but with the risk that it would bring satisfaction to none.
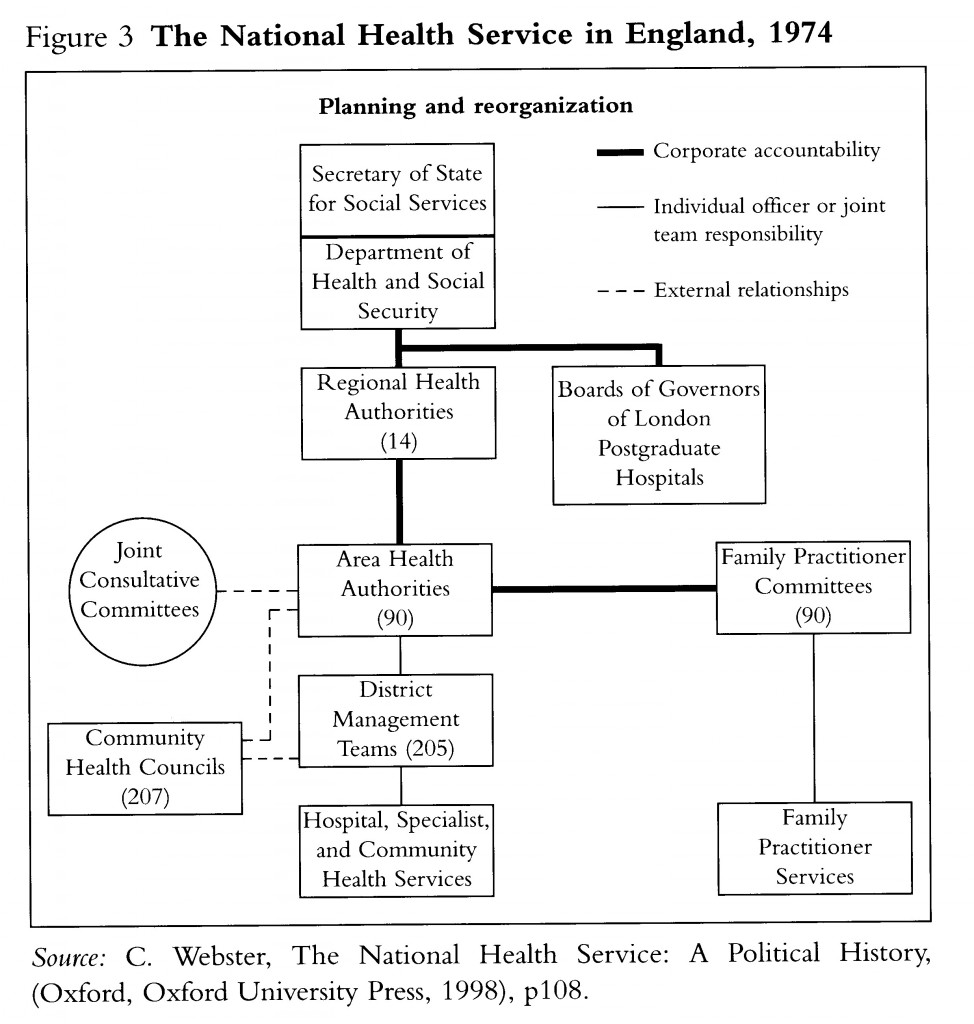
The erratic path towards the 1974 reorganisation is reminiscent of events during the wartime coalition government in 1945, which also produced a plan of such impossible complexity that was wisely thrown out by Bevan. As indicated by Figure 3, by the time the Joseph edifice was complete, it was only a modest step towards unification, and it made virtually no contribution to simplification of health service administration.
Indeed, these hitherto primary objectives were largely lost sight of during the later stages of the reorganisation exercise. Joseph pinned his hopes for improvement on imposing a strong management emphasis throughout the new structure. It should not be forgotten that both friends and enemies alike regarded the 1974 reorganisation as a product of the latest management thinking, and management experts were co-opted to convert Joseph’s plan into a workable management structure. The management experts were, however, more divided over the merits of Joseph’s scheme than they seemed on the surface and Joseph, like Grossman, was by no means convinced that his officials were justified in their preferences. Indeed had Joseph and his business allies been heeded, there would have been no need for the Griffiths management reforms of the late-1980s, and the 1974 experiment in consensus management would never have been launched.13 Instead, in 1974 the health service would have been placed under some form of NHS Corporation and directed by a chief executive, while a system of general management would have been introduced at all three levels of the NHS hierarchy.14 These changes would have involved dispensing with the regional authorities, substituting regional offices of DHSS, so anticipating the changes eventually made in 1996.
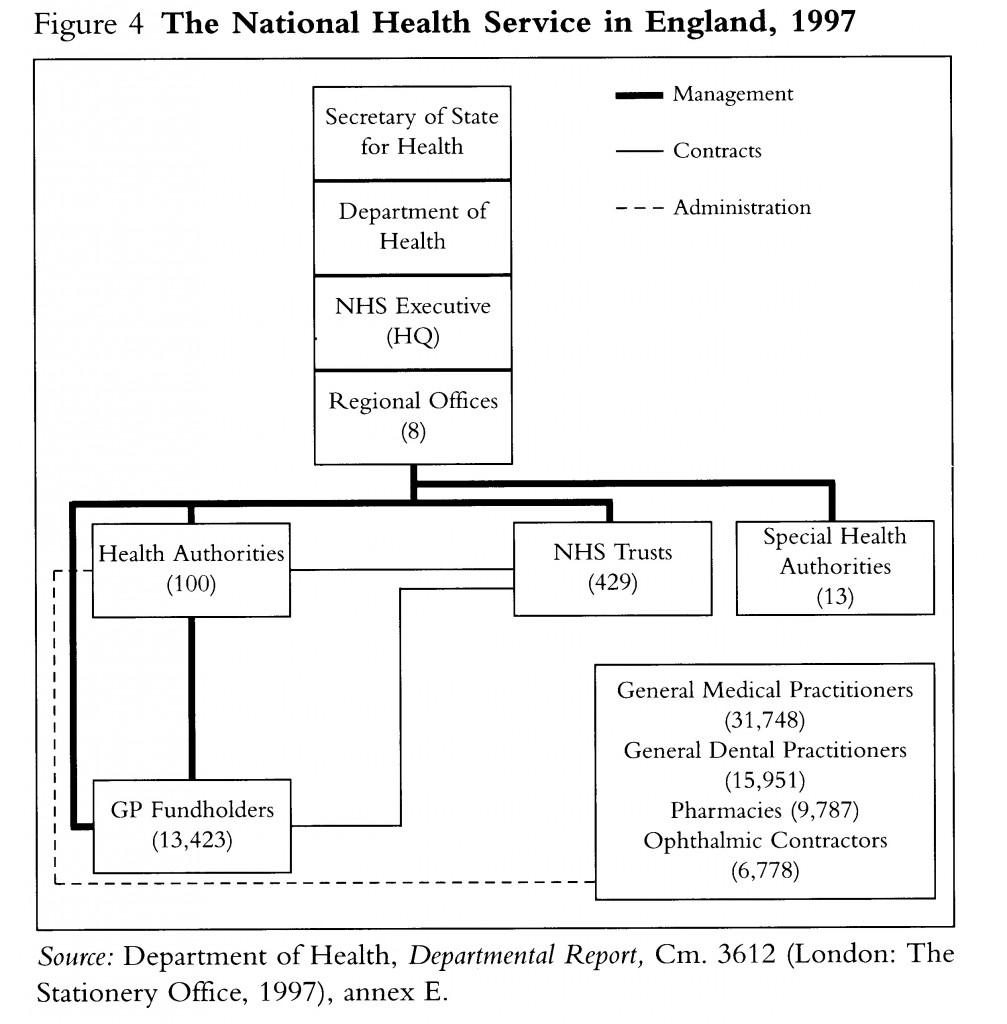
IV WORKING FOR PATIENTS
Between 1979 and 1997 the Conservatives eagerly embraced Sir Keith Joseph’s zeal for strong management, in the course of which they also effectively dismantled the entire health service edifice that he had created, as indicated by a comparison of Figures 3 and 4. By 1997, the only part of the 1974 structure remaining in its recognisably original form was the Community Health Council. This is itself a paradox, since the CHC was the first part of the Joseph system proposed for demolition at the outset of the Thatcher administration. This bald summary perhaps conveys an impression that the actions of the Thatcher administration in the field of health care possessed a firm sense of direction, consistent with changes taking place elsewhere in the welfare state. In fact, the Thatcher government showed little sense of the sure-footedness in health that it displayed elsewhere in welfare policy. Indeed, some of the Conservatives’ policy preoccupations, pursued periodically throughout the 1980s, such as insurance funding of health care, were futile and time-wasting. They were also counterproductive because they undermined confidence in the government’s commitment to the NHS.15
Although the Thatcher team is remembered for its Working for Patients initiative, its first effort at structural change was announced in Patients First, published with in a few months of entering office. Most of the Patients First reforms were implemented in 1982. By contrast with Labour’s dramatic intervention in 1945, at this early stage the Conservatives introduced only minor and uncontentious changes, and there was an emphasis on continuity. There were virtually no premonitions of the policy objectives embodied in the Griffiths Report or in Working for Patients. Indeed Patients First was subversive to later-adopted policies through its commitment to decentralisation, consensus management, and through its perhaps intentional obstruction of steps towards both the extension of cash limits and the integrated management of hospital, community and family practitioner services. Even the biggest change introduced by Patients First, the removal of the area tier, although unwelcome to local government on account of the latter’s attachment to the principle of coterminosity, was not intended as a foretaste of the Conservatives’ later assaults on local government.
After Patients First, the direction of policy was much affected by the new taste for remitting problems to small teams of outsiders, sometimes headed by leading businessmen. It has already been noted that at the time of the Joseph review in the early 1970s, the government’s bvjsiness team had been spurned in the interest of management solutions more congenial to the NHS professions. By contrast, under Mrs.Thatcher the businessmen were likely to carry the day and it was the turn of the NHS professions to be sidelined. The Griffiths management review was the first dramatic manifestation of the new mode of policy-making.
This was the first occasion since the start of the health service that important changes were brought about in the face of professional opposition. It was therefore a major precedent. The government was, however, somewhat slow to push home its advantage. It was for instance more circumspect in its handling general practitioners than of their colleagues in the hospital sector. With reference to the independent contractors, the government proceeded along the customary course of green and white papers, and interminable consultation. Again following a long tradition, this exercise culminated in grass roots protest leading to rejection by the general practitioners of the new contract. It was eventually imposed in 1990. This may have seemed like a humiliation of the general practitioners, but in fact the contract was not a particularly radical venture; indeed, in many respects it was just as much a creature of the professions making as were its predecessors in 1948 and 1966.16 The government aspired to turn the clock back to 1948 by placing the burden of remuneration on the capitation payment. Although the profession complained about this change, a modification in this direction also suited it, and the compromise adopted broadly coincided •with the profession’s wishes. Even on the bitterly contested question of introduction of a compulsory retirement age for general practitioners, this had long been advocated by expert bodies reporting on primary care.17
The general practitioners may have enjoyed favourable treatment with the contract, but they were at last swept up into the cauldron of change in the course of the reforms announced in the White Paper, Working for Patients, issued in January 1989. Few would dispute Mrs.Thatcher’s claim in the Foreword that her government’s proposals represented the ‘most far-reaching reform of the NHS in its forty-year history’.18 However, since many of the main proposals for change were vague or optional, it was far from evident at the date of publication that general practitioners or others within the health service would be vitally affected by this policy declaration. The unusual circumstances of origin and formulation of the White Paper reinforced this air of uncertainty. By contrast with the health service reorganisations of 1948 and 1974, the 1989 proposals (as with Griffiths) were not preceded by a long period of gestation and negotiation with relevant interest groups. The Conservative 1987 general election manifesto gave no intimation that the government was contemplating anything more radical than continuation of its existing programme to secure better value for money. In view of its major policy commitments in the fields of education, housing and local government, and in the absence of any settled policy concerning the long-term future of health care, the idea of structural overhaul of the NHS, although recognised as a desirable objective, was ruled out for the third term of the Thatcher administration.
It is well known that the government was blown off-course by the financial crisis affecting the health service in the autumn of 1987, with the result that it was forced to address as a matter of urgency the problems of additional resources and cost containment. In view of the ideological standpoint of the government, this inevitably involved a further review of alternative funding of health care, and also policy options for more radical means of improving the productivity of the system. Such an exercise was attended by dangers of adverse publicity, as witnessed in the autumn of 1982 when consideration of radical ideas about cutting back on government expenditure on the NHS had been wrecked owing to damaging leaks emanating from Cabinet wets.19 It was therefore decided to remit this review to a small group of ministers and senior advisers such as Sir Roy Griffiths, who could be trusted to safeguard confidentiality and to steer discussions along the right lines. This tightly defined interdepartmental ministerial group even excluded the health ministers for Scotland and Wales until the eleventh hour. As with the earlier Griffiths management review and other exercises of a similar type, this route to policy-making kept the bodies representing the NHS workforce very much at bay. Certain doctors were involved on the sidelines, but they were selected on the basis of their individual qualities. The most vociferous outside influence emanated from a small group of activists associated with Conservative think tanks. This group mounted the most spirited pamphlet and press campaign to be witnessed since the idea of a national health service was first debated during the Second World War. By contrast, during 1988 the voices that had been dominant on all previous occasions, representing the political left, the health professions, or local government, were very much relegated to the sidelines.
The Thatcher review was without precedent in the history of policy-making in the NHS. The 1968 Green Paper was produced under similar conditions of secrecy, but this exercise was thought not to be controversial, since it was merely regurgitating the well-regarded Porritt scheme, and it was at least the direct product of the health department itself. During 1988, DHSS (from July 1988 Department of Health), played the lead role, but the Treasury was more active than in previous reorganisations, and the Prime Minister and her advisors also exercised a continuous influence. At the beginning of the Thatcher review it was by no means certain that any significant structural changes would be entailed by its findings. Although outsiders close to the review team actively promoted the idea of an internal market from the outset of the exercise, there were few early indications that this would be the main outcome. Key proposals by which the White Paper is now remembered, such as hospital trusts, or general practitioner fundholding, were included only as an afterthought or with the greatest reservation. Had it not been for accidental factors, Working for Patients might have been a much less ambitious document, containing nothing more than building on the existing programme for improving the use of resources, including the greater integration of consultants in managing resources, moves towards the Patient’s Charter, further extension of the role of the private sector, and perhaps minor steps in the direction of greater self-government in hospitals. Even in the summer of 1988, there was every chance that the government would pronounce against any general structural overhaul. Echoing the caution that surfaced before the 1987 general election, more radical propositions might well have been deferred until after the 1992 election, and then might only have been ventilated in a Green Paper.
This late conversion to more radical objectives accounts for the ambivalent character of Working for Patients. Contrasting with the detailed blueprints preceding the 1948 and 1974 reorganisations, Working for Patients provided only the vaguest signposts concerning the scale and character of many of its more important provisions. The direction and extent of the journey depended on the determination of the Secretary of State and the ability of the newly-formed NHS Management Executive to mobilise incentives for change. Kenneth Clarke proved himself the equal to Bevan in his pertinacity and degree of commitment to the new scheme; also like his predecessor, Clarke was forced to contend with much scepticism within his party and even among cabinet colleagues. In this respect Clarke ranks with Bevan in the degree of his personal influence on the shape of the British health care system. With Clarke’s backing, the internal market changes were implemented more rapidly than was ever anticipated at the outset, in the process generating further pressures for structural change. Consequently, as indicated in Figure 4, by the date of the 1997 general election the Working for Patients changes had somewhat fortuitously turned into the radical overhaul anticipated by Mrs.Thatcher in 1989.
V INTERNAL MARKET TO INTEGRATED CARE
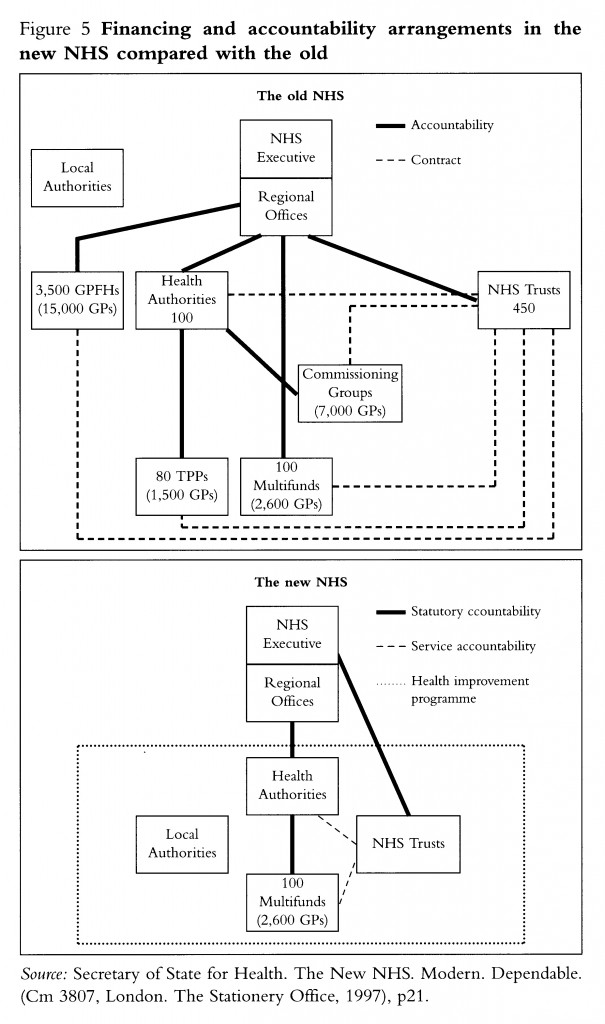
Paradoxically, the massive and painful structural overhaul of the health service undertaken since 1991 has not been accompanied by anything like the unfettered operation of a competitive market of the kind widely-advocated in Conservative circles. Indeed, by the end of the most recent Conservative administration, the term internal market was falling into disuse on account of its self-evident inappropriateness. However, the internal market retained its salience in the political context, and it proved a prime target for attack by New Labour. The three recent White Papers on the future of the health service in England, Scotland and Wales fulfil Labour’s election pledges by announcing the government’s intention of replacing the internal market by what it calls integrated care20. In practice, many of the key features of the system introduced since 1989 are likely to be retained or become only slightly modified. Many of the likely changes represent continuation of trends established by the Conservatives, suitably refined to blend with the policy ethos of New Labour. In other respects, however, as evident from Figure 5, it is clear that Labour is following the Thatcher path and embarking on a further phase of structural overhaul of uncertain scale and direction that could ultimately transform the health service to the same extent as the Working for Patients changes. It is of course too soon to comment in detail on the most recent phase of reorganisation policy-making. On the one hand, formulation of the new policy was even more hurried and secretive than in the case of the 1988 Thatcher review; on the other hand it can be legitimately claimed that the main lines of the present policy were clearly signposted in the 1997 Labour election manifesto. Somewhat surprisingly, the current wave of overhaul is the first occasion upon which major changes in the health service have been signalled in a general election manifesto.
It remains to be seen whether Labour will prove able to endow its plans with a greater degree of certainty and credibility than proved possible with respect to the internal market reforms. The above survey gives little room for complacency. The historical record suggests that architects of major structural transformations in the health service have perhaps been too readily convinced by their own propaganda, and have overestimated the capacity of their schemes to bring about improvement and generate satisfaction among the NHS -workforce and users of the service. Regrettably, the evidence of history supports the conclusion of Professor Reinhardt that episodes of reorganisation tend to replace one unsatisfactory system by another, and therefore serve to generate further pressures for change. Even worse, the time intervals between episodes of major structural reform have progressively diminished to the point that the NHS risks becoming caught up in a vortex of permanent upheaval.
The change of direction signified by the recent White Papers presents a fresh opportunity for reassessment, the rebuilding of confidence and restoration of morale within the health service. The public and the health service workforce deserve respite from gratuitous political interference, but they also need convincing that the new policy framework will endow the health service with a degree of stability that has so far proved unattainable. In the course of its interventions, Labour -will need to prove that it is not subjecting a great national institution to the vagaries of a policy lottery.
As Professor Reinhardt indicated, it is difficult to resist pessimistic conclusions concerning the prospects for reform. However, in the UK we should gain heart from the example of the early health service. Although in the age of managed competition, the command and control system adopted by Bevan has sunken out of favour, it should be remembered that in conditions of great austerity, Bevan’s health service proved remarkably successful, and it achieved great efficiency gains compared with its pre-war market predecessor. Bevan’s health service not only earned the confidence of the public and the NHS workforce, but its achievements were sufficiently solid to withstand scrutiny in the mid-1950s from the economist C. W. Guillebaud and his committee, and from a related distinguished report from Brian Abel-Smith and Richard Titmuss21. At that date the NHS faced serious problems, but there was no sense that the system was out of control, and every confidence that with a modest injection of additional resources and continuing improvements in efficiency, the service would prove permanently viable. Given the great reserves of experience and wisdom available to the NHS as it nears the millennium, there is every reason to believe that the same spirit of confidence concerning the future could be restored and enhanced.
VI THE WAY AHEAD
However laudable their objectives, the 1974 and 1991 reorganisations of the health service scarcely merit selection as textbook planning operations. Although the reorganisation problem -was handled very differently in the two cases, each involved a degree of arbitrariness and lack of rationality that was likely to impair success in problem solving, and inevitably fuelled widespread dissatisfaction with the resultant reforms. Hopefully, Labour will now observe the lessons to be gained from these mistakes of the not so distant past. It is not unreasonable to expect modern government to desist from gratuitous interventions, and adopt a more scientific and systematic approach to the problems of organising and managing the health service. Government should not only adopt a more solid basis of evidence for proposed changes, but should also subject innovations to critical testing before they are applied more generally.
Governments have been notoriously reticent to subject their brainwaves to experimental verification. The wartime coalition government promised experiments with health centres, but there had been virtually no testing of health centres when the health departments sanctioned the sudden rush for health centres in the mid-1960s. With respect to the 1974 reorganisation, the government ignored pleas for experimentation with different types of reorganisation conducted on a regional basis. In the 1980s, friends of the government such as Enthoven argued the case for experiment with respect to the Griffiths management changes and the key recommendations of the 1989 White Paper. These views were reinforced by others during the debate on Working for Patients, but were ignored.22 Of the 1991 changes, fundholding -was the most obvious candidate for controlled experiment, but this innovation -was forced ahead regardless of the consequences. No thought seems to have been given to slowing down the pace of the change pending correction of the self-evidently defective performance of the great majority of existing fundholding practices found by the Audit Commission.23
The recent White Papers on the future of the health service give grounds for optimism that a more undogmatic and exploratory approach to policy-making is being adopted with respect to the organisation of the future health service. For instance, the English White Paper, following ministerial statements to that effect, in its concluding sentence, promises that with respect to its key proposal for Primary Care Trusts, evaluation of early progress will precede their universal application.24 There are consequently signs that the government is absorbing lessons from the more scientific approach to policy that is increasingly prevalent in the operations of the health service at grass roots level owing to the influence of such diverse factors as evidence-based medicine, performance measurement, and the various applications of audit.
It is important that every effort should be made to improve the effectiveness of such instruments of analysis. Their full potential will not be realised without the introduction of mechanisms of institutional advocacy and support separate from the Department of Health and the NHS Executive. In recent years, the Conservative Government took steps in this direction by introducing the Clinical Standards Advisory Group and the Research and Development Programme. The Labour government has continued this trend with its proposals for a programme of new evidence-based National Service Frameworks, a National Institute of Clinical Excellence and a Commission for Health Improvement.25 The government declares its intention to determine that ‘the services and treatment that patients receive across the NHS should be based on the best evidence of what does and does not work and what provides best value for money’.26
These sentiments precisely echo the ethos of the new public management that took root during the Thatcher administration.27 Arguably the single new public management innovation having the greatest impact on the health and personal social services was establishment of the Audit Commission. This was formed in 1982 and its remit was extended into the health service in the 1990s. As we are repeatedly reminded in the reports of the Audit Commission, it is concerned with ensuring that the bodies under its scrutiny adhere to statutory regulations and that they have made proper arrangements for ‘securing economy, efficiency, and effectiveness’ in their use of resources.28 Since entering the health care field, the Audit Commission has issued about forty reports on health and community care, many of them value for money exercises, and dealing with a wide range of specialties. Some of these reports have been concerned with monitoring the development of internal market changes. Although sometimes making recommendations unpalatable to professional bodies, reports of the Audit Commission have generally been regarded as competent and constructive. Sometimes, as in the case of the above-mentioned 1996 report on GP fundholding, the Audit Commission has been less flattering than other research studies about the success of a flagship government policy. The reports of the Audit Commission have performed a wide range of functions, ranging from promotion of central government policies to testing the water on tentative ideas about the development of care. In practice the role of the Audit Commission has therefore not been limited to the monitoring and control of implementation of existing policy. It has often crossed the line into providing guidance on the future development of policy. However, for a variety of reasons outlined below, the latitude of the Audit Commission for recommending departure from existing policy is distinctly limited.
Taking into account the Audit Commission, other established central advisory bodies, and proposals for a National Institute of Clinical Excellence and a Commission for Health Improvement, the government seems to be reinventing the comprehensive central expert advisory machinery which was built up between 1948 and 1979. Most of this was swept away by the Thatcher administration in its early assault on public interest quangos. These bodies varied greatly in their competence, but at their best they produced useful and important reports. The National Audit Office and the Audit Commission have subsequently covered some of the same ground. These later reports possess certain advantages, but it cannot be claimed that the Audit Commission and National Audit Office constitute a credible substitute for the previous central advisory machinery. Indicative of a tendency to use the existence of audit machinery as an excuse for eliminating other agencies of inspection and advice is provided by the recent abolition of the Health Advisory Service. The latter was one of the few surviving remnants of the inspectoral and advisory structure in existence before 1979. It had been in a vulnerable position for some time as it had been precluded from fulfilling the ambitious remit intended by its creator, Richard Grossman. There must now be the further danger that existence of the Audit Commission will be used as the excuse to mop up the small residue of other independent sources of advice and inspection such as the Social Services Inspectorate.
Hopefully, the tendency towards monopolisation on the part of the Audit Commission will now be counteracted by an evolving central advisory apparatus which will improve the quality of guidance provided to ministers on policy issues. The various agencies are likely to be free of the inertia and medico-political interference that hampered the old advisory structure. However, in other respects, the new structure will be inferior to the old. The bodies established will vary in their statutory character and degree of independence, and they will lack a structured relationship with one another. This mixture of disparate elements will leave substantial gaps, but it is also likely to throw up problems of duplication. Owing to their necessarily independence and regulatory functions, the National Audit Office and the Audit Commission cannot be integrated with the rest of the central advisory structure.
Despite the strength of its current contribution, and its amassing of new spheres of activity, the Audit Commission is not in a position to assume a role of supremacy in the provision of policy guidance in the health service. The reputation of the Audit Commission will suffer if it is expected to carry more -weight than it can reasonably be expected to bear. As its title reminds us, the Audit Commission, like the National Audit Office, remains primarily concerned with financial audit, and this role must not be undermined by too many distractions. The role of the Audit Commission with respect to the NHS is also limited by its status as an omnibus body, approximately two-thirds of the functions of which lie outside the health service. Other disadvantages of the Audit Commission result from its statutory obligation to operate within the framework of prevailing government policy, and also its strong working ties with the Department of Health, the NHS Executive and health service management.29 At an extreme this places limitations on the choice of topic for investigation, thereby possibly restricting entry into sensitive policy areas, in favour of innocuous and uncontentious subject matter. The success of the Audit Commission with respect to the health service does not therefore obviate the need for other central instruments of policy guidance free from the restrictions applying to the statutory audit bodies, less slavishly committed to cost-cutting, more genuinely concerned with effectiveness, capable of applying more varied investigative methodologies, open to a wider range of representations, and possessing greater transparency in their enquiries.
Although there is obviously an important continuing role for the Audit Commission, the government’s ideas about a National Institute of Clinical Excellence or a Commission for Health Improvement represent steps towards reinforcing the effectiveness of the central regulatory and advisory machinery. But there is self-evidently need for a more comprehensive mechanism of policy guidance at the centre than is currently in existence. The case for such a mechanism -was recognised when the Ministry of Health was set up in 1919; at that time the government established separate Consultative Councils for Medical and Allied Services for England, Scotland and Wales. The first product of the former was the celebrated Dawson Report, after which the Council was frozen out of existence largely on account of over-ambitious interpretation of its remit. This episode caused the medical profession to insist on the establishment of a comprehensive statutory central advisory machinery at the outset of the NHS as one of the conditions of its entry into the service.30 As I have already indicated, this over-complicated structure was only partly successful, but in 1979 a mistake was made when the policy of demolition rather than reinforcement was adopted.
In the present circumstances, an alternative worthy of further exploration would be to carry the present reforms to their logical conclusion and establish a National Health Service Commission to exercise the powers residing in existing bodies and extend its remit to all aspects of the health service. Its role would then be as comprehensive as the Law Commission in its field of existence. Over the thirty years of its existence, the Law Commission has demonstrated the value of a central body of this type, and if anything its reputation is higher now than ever before with respect to modernising the legal System.31 There is no reason -why a Commission established at a similar level for the health service should not attain a similar degree of authority and usefulness in the modernisation of the health service. Similar expedients have been tried to a limited extent elsewhere, and they have in some cases been an outstanding success. The argument for a strong independent source of advice to ministers is now stronger than ever before owing to variety of reasons, including: the decline in the role of elected authorities, the great power now exercised by the NHS Executive and its regional offices, the reduced role of the Department of Health, the dismantling of separate professional divisions within the health department, and the less comprehensive character of primary legislation.
The government and health service establishment will naturally be timid about such a radical proposition. Ministers and bureaucrats dislike sacrificing their control over sources of advice. The existence of a NHS Commission would of course not diminish the capacity of ministers to employ other avenues of advice. But they themselves now concede the need for central agencies possessing a degree of statutory independence and possessing wide-ranging responsibilities. It is recognised that such independent bodies are essential for maintaining the confidence of the professions and the public. A NHS Commission will certainly be resisted on the grounds that it will be captured by the medical profession and because it could lead to expenditure implications. In order to command credibility, the Commission would certainly include a strong medical voice, but the members would not be delegates representing vested interests. As in the case of other expert bodies, they would be appointed on the strength of their independent authority, and be joined by colleagues of similar rank representing other professions engaged with health care. The Commission would also make recommendations entailing expenditure implications, but these need not invariably point in the direction of increased expenditure, and they would obviously be framed in a spirit of responsibility with respect to economic realities. In fact the more serious danger is that the Commission would, like the rest of the machinery of audit and policy, risk being too heavily controlled and inhibited from freedom of action. The real test of a NHS Commission would lie in its capacity to challenge received wisdom, and its ability to produce reports of similar gravity to the Dawson Report and then afterwards survive the predicable depredations of its detractors to undertake further constructive activities of similar merit. This would necessitate stepping into territory forbidden to the Audit Commission and even investigating such controversial matters as rationing, health service charges, capital charges, the Private Finance Initiative, or the present government’s proposals for structural changes in primary care. In the course of time the NHS Commission wmild undertake a comprehensive review of main policy problems affecting the health service, in effect acting like a Royal Commission on the health service, but conducting its work in a more deliberate and expert manner. For this purpose it would need to employ the facilities of research in a much more effective manner than the Royal Commission that reported in 1979, and which remains the only official high-level enquiry undertaken into the UK health services in the course of the present century.32 I am convinced that a NHS Commission granted a full measure of responsibility would bring to bear a weight of intelligence greater than available from any other source. It would be in a position to make a constructive contribution quite as important as that of the National Audit Office and Audit Commission. The existence of a variety of agencies of accountability, audit and expert advice at the centre ought to be welcomed as a natural development of the new public management. In this spectrum of central bodies, the NHS Commission would be the only one systematically open to all relevant expert opinion, and the representations from bodies representing the voice of patient groups and communities. In this respect the Commission would contribute in a modest way to reducing the scale of the democratic deficit that has opened up in the health service, and which constitutes one of its most glaring deficiencies.
My proposal may seem somewhat Utopian, but I gain comfort from the recent decision of the government to overcome bitter bureaucratic and producer resistance and set up a Food Standards Agency. Integral to this proposal is a Commission charged with the ‘protection of public health in relation to food’. The government anticipates that this body will possess wide-ranging powers to commission research, conduct surveillance, and formulate policy and legislation. Its conclusions would be ‘unbiased and based on the best available scientific advice, provided by experts invited in their own right to give independent advice’. In addition, its reviews of policy are intended to be ‘open, transparent and consultative’, subject to public scrutiny, and with full rights of access to the voice of the public. Finally, the government is confident that the work of the Commission will constitute a contribution to efficiency and economy in the use of resources.33 If these principles had been observed when the government undertook the reviews that led to the 1974 and 1991 NHS reorganisations, the public might now be less anxious and the NHS workforce less demoralised about the state of the health service. With respect to that part of its health associated with food, the public is now about to gain the protection of a Commission. I am merely asking that this principle should be applied to the health service as a whole. The government has in fact been reaching towards the conception of a NHS Commission ever since Morant designed the Ministry of Health in 1919, but periodic efforts at implementation have been impaired by lack of conviction. The fiftieth anniversary of the NHS provides an ideal opportunity to realise this far-sighted objective of the original architects of the Ministry of Health.
References
1 Sir Douglas Black, A Doctor Looks at Health Economics, OHE Annual Lecture 1994, London, Office of Health Economics, 1994, p.31.
2 Uwe. E. Reinhardt, Accountable Health Care. Is it compatible with social solidarity? OHE Annual Lecture 1997, London, Office of Health Economics, 1998, pp.5, 69.
3 Secretary of State for Health, The New NHS. Modern. Dependable, Cm 3807, London, The Stationery Office, 1997; Secretary of State for Scotland, Designed to Care. Renewing the National Health Service in Scotland, Cm 3811, Edinburgh, The Stationery Office, 1997; Secretary of State for Wales, NHS Wales. Putting Patients First, Cm 3841, London, The Stationery Office, 1998.
4 The Establishment of the NHS in 1948 and its reorganisation in 1974 and 1991 are reviewed in R. Klein, The New Politics of the NHS, 3rd edn, London, Longman, 1995, and C. Webster, The National Health Service, A Political History, Oxford, Oxford University Press, 1998. These introductory books give guidance on the more specialised literature.
5 G. Rivett, From Cradle to Grave. Fifty Years of the NHS, London, King’s Fund Publishing, 1998.
6 The New NHS. Modern, Dependable, p.2.
7 Ministry of Health, Consultative Council on Medical and Allied Services. Interim Report on the Future Provision of Medical and Allied Services, Cmd. 693, London, HMSO, 1920.
8 C. Webster, ‘Birth of the Dream. Bevan and the Architecture of the National Health Service’, in G. Goodman ed., The State of the Nation. The Political Legacy of Aneurin Bevan, London, Gollancz, 1997, pp. 106-29.
9 Medical Services Review Committee, A Review of the Medical Services in Great Britain, London, Social Assay, 1962.
10 Royal Commission on Medical Education 1965-1968 Report, Cmnd. 3569, London, HMSO, 1968; Report of the Committee on the Local Government and Allied Personal Social Services, Cmnd. 3707, London, HMSO, 1968; Royal Commission on Local Government in England Report, Cmnd. 4040, London, HMSO, 1969.
11 National Health Service. The Administrative Structure of the Medical and Related Services in England and Wales, London, HMSO, 1968.
12 R. H. S. Crossman, A Politician’s view of health service planning, Glasgow, University of Glasgow, 1972 (Maurice Bloch Lecture 13).
13 C. Webster, The Health Services since the War, ii, Government and Health Care. The British National Health Service 1958-1979, London, The Stationery Office, 1996, pp.461-2, 496-504.
14 The NHS Corporation and chief executive idea was also seriously considered in the md-1960s, for details of which, see Webster, The Health Services since the War, ii, pp.334-6.
15 C. Webster, The National Health Service. A Political History, pp.153-6.
16 M. Marinker, ‘General Practice and the New Contract’, in G. Bevan and M. Marinker, Greening the White Paper, London, The Social Market Foundation, 1989, pp.8-17.
17 Royal Commission on the National Health Service. Chairman: Sir Alec Merrison. Report, Cmnd. 7615, London, HMSO, 1979, para 7.18; London Health Planning Consortium, Primary Care Study Group, Primary Health Care in Inner London, London, DHSS, 1981.
18 Secretaries of State for Health, Wales, Northern Ireland, and Scotland, Working for Patients, Cm 555, London, HMSO, 1989, Foreword.
19 P. Riddell, The Thatcher Government, Oxford, Martin Robertson, 1983, pp. 132-6.
20 The New NHS, para 1.3.
21 Report of the Committee of Enquiry into the Cost of the National Health Service, Cmd. 9663, London, HMSO, 1956; B. Abel-Smith and R. M. Titmuss, The Cost of the National Health Service in England and Wales, Cambridge, Cambridge University Press, 1956.
22 Bevan and Marinker, Greening the White Paper, pp.35-44.
23 Audit Commission, What the Doctor Ordered. A Study of GP Fundholders in England and Wales, Audit Commission, 1996.
24 The New NHS, p.81.
25 The New NHS, para 7.6.
26 The New NHS, para 7.5.
27 C. Hood, ‘The “New Public Management” in the 1980s: Variations on a theme’, Accounting, Organisations and Society, 1995, 20, 93-109; N. Rose and P. Miller, ‘Political Power beyond the State: Problematics of Government’, British Journal of Sociology, 1992, 43, 173-205.
28 Local Government Finance Act 1982, section 15.
29 M. Bowerman, ‘Time to Repositon Public Audit?’, Public Finance Foundation Review, 1996, 9, 3-6; M. Power, The Audit Society. Rituals of Verification, Oxford, Oxford University Press, 1997; P. A. West, Understanding the National Health Service Reforms. The Creation of Incentives? Buckingham, Open University Press, 1997, p.176.
30 C. Webster, The Health Services since the War, i, Problems of Health Care. The National Health Service before 1957, London, HMSO, 1988, pp. 241-56.
31 S. Cretney, ‘The Politics of Law Reform – A View from the Inside’, Modern Law Review, 1985, 48, 493-517; G. Zellick, ed., The Law Commission and Law Reform, London, Sweet and Maxwell, 1988.
32 Royal Commission on the National Health Service. Chairman, Sir Alec Merison. Report. Cmnd. 9615, London, HMSO, 1979.
33 Minister of Agriculture, Fisheries and Food, The Food Standards Agency. A Force for Change, January 1998, Cm 3830, London Stationery Office, 1998, paras 1.2,1.10,2.4.