Whilst attention has been paid to issues around Hospital Standardised Mortality Ratio (HSMR[1]) at Mid. Staffs I have examined simple mortality rates. The use of HSMR remains controversial as the ratio is influenced by issues around quality and depth of coding as well as interpretation and recording problems. I used figures which were not subject to coding or interpretation. The mortality rate is just the number of deaths divided by the level of activity, easy to use and understand. You could just look at the number of deaths but almost all hospitals are dealing with increasing levels of activity. Crude mortality rates are valuable as time trends rather than as a basis for comparing hospitals.
The first graph shows the mortality rate for non elective (emergency) care at Mid. Staffs. To correct for well known seasonal factors the figures are for whole years ending at the date shown.
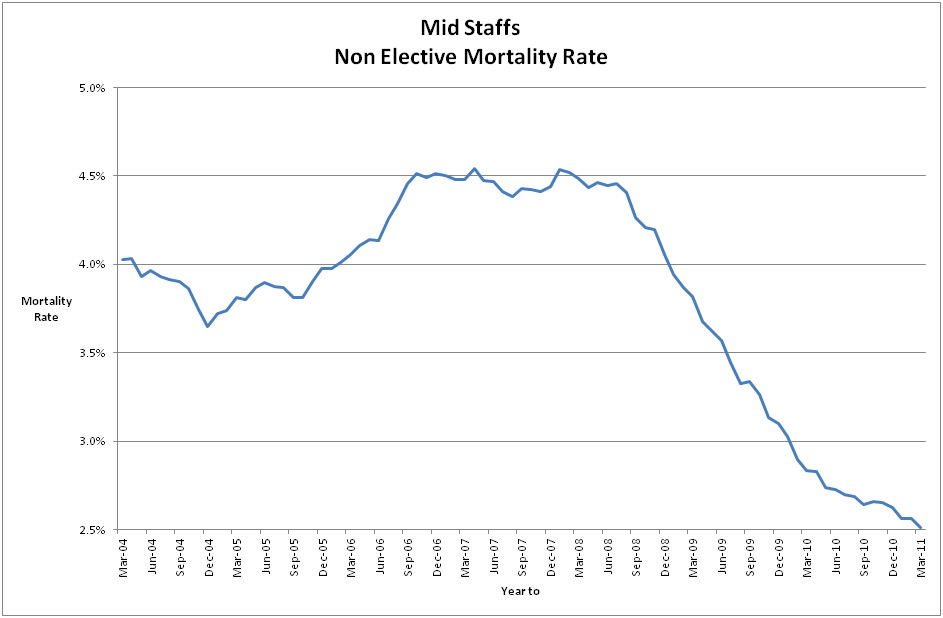
Having looked at many hospitals’ data, and at the various different ways of measuring the mortality rate, I can comment that it is unusual for this type of graph to show anything other than a consistent downward trend with random variations around the trend. The anomaly with Mid. Staffs is a prolonged period of increasing rates. But the upward trend commenced during 2004 and by 2006 it looks as if remedial actions have worked, and by 2008 there is a rapid improvement. The Trust was awarded Foundation Trust status in February 2008 and in March 2008 the Healthcare Commission launched an investigation into high mortality rates in emergency admissions for the period 2005 – 2007 during which the mortality ratios were consistently high, which reported in March 2009 – leading to Francis 1.
So they looked at the right period but by the time the report was published and the Francis enquiry was set up it looks very much as if corrective action had been taken. This is not what Francis reported.
The second graph looks at Mid. Staffs. death rates in comparison with two other hospitals, one with a historically high mortality rate and HSMR and one with a low mortality rate and HSMR and also for the entire Eastern Region. For this the deaths are actually in the 56 diagnostic groups (as used by DR. Foster) which comprise around 85% of deaths.
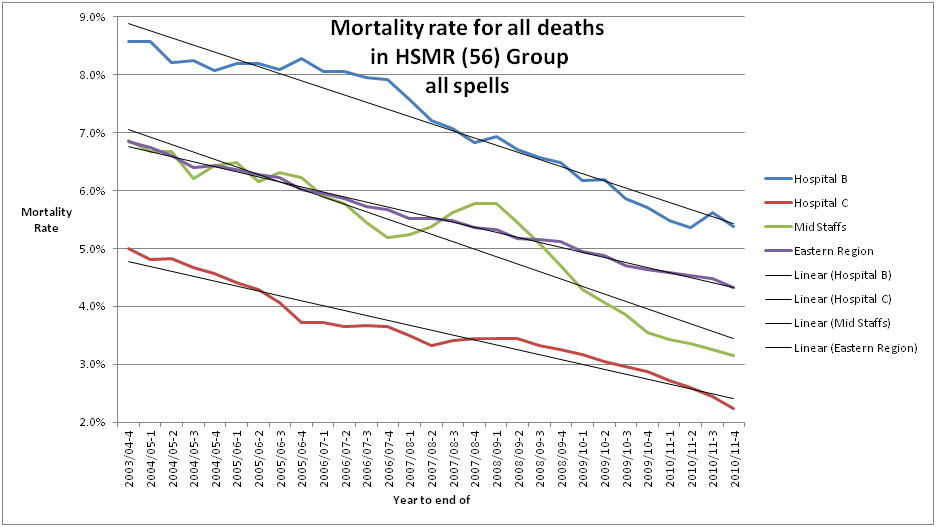
This shows that in terms of death rates Mid. Staffs was pretty average and well below the worst. Again the period of upward trend around 2005 – 2007 would merit investigation.
Crude death rates are actually of little use in comparing hospitals with each other, but trends are important. Overall you could simply say that anyone who just looked at the number of deaths or the death rate at Mid. Staffs without any reference to HSMR or anything sophisticated would have seen there was something going on.
But none of this leads to any conclusion about excess deaths or avoidable deaths.
[1] There is now also a Summary Hospital (level) Mortality Indicator (SHMI) which is based on all deaths from all causes both in hospital and within 30 days of discharge but which will exclude in the denominator those spells which were for day case and zero LOS. This will be a better measure but still subject to coding and other error.
Steve Walker on the myths of avoidable deaths
