It’s interesting to go through the how structure of NHS changed in the last thirty years. I have worked and been through the best times, worst times been through all these stages since 1980. The number of patients visiting doctors has not changed in proportion to the number of doctors employed but the morale has declined.
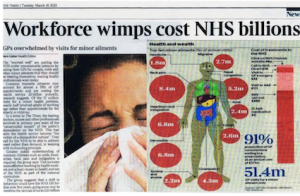
The problem in the NHS is because there are too many chiefs and less horses to pull the cart. Statistics do not give you a clear picture and tell you what and how the very people who claim to defend patient care have systematically vandalized the healthcare system.
You may think I am crazy but I blame the doctors and nurses and patients for killing the goose that once laid golden eggs. In no other country in the world can incompetent doctors or nurses survive because people who consult them have a choice to find another one. In UK the cost of private care is exorbitant so not many can afford. I do not say the quality of care offered in the private sector is better but the way you are managed may be. Doctors and nurses in private hospitals are more polite, spend time to explain and are courteous when compared to some doctors working in the NHS. We must not forget doctors working (SHO & Registrars) in the NHS are over worked, underpaid, and are very stressed.
People who rush to hospital with simple common problem are more demanding and expect special treatment and are also the first ones who complain if they don’t get what they want. This has resulted in doctors shying away, retiring and simply emigrating. They are also not aware about the cost of care because they are told “Its Free”.
When I worked as a locum GP, I estimated the cost of consulting was around £90-£120 per patient. As a GP on call visiting one patient at home was approximately £400-£600 per patient. This could go as high as £6000 if the doctor spent six hours managing a patient at home.
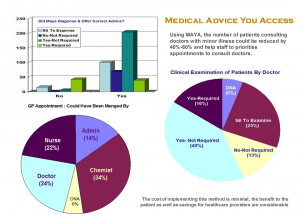
Knowing NHS will not cope and worried about spreading infection, I started collecting data and compiled a list of common presenting symptoms and my diagnosis. After analysing the result, I found only 24% of the patients who consulted doctors as an emergency actually had some illness that required a doctor’s advice and only 16% of patients required clinical examination (this includes seeing a rash). More than 40% of patients who demanded emergency appointments with common symptoms were between 18-40 years.
Whom Can We Blame?
The politicians, doctors, nurses or the patients? I think we all must share the blame equally.
- The politicians for promising what they cannot deliver and thriving on gaining your support and votes.
- Doctors for encouraging patients with trivial problems to consult and offer treatment just to make sure the patient feels happy. This is because the income in the surgery increased depending on the number of patients and not based on the type of patients they cater for. I have found surgeries in affluent areas have senior partners seeing only private patients and locums or salaried doctors taking care of NHS patients.
- Nurses who think their duty is to keep an eye on doctors and forgot their duty is to take care of patients. It looks as if they have lost their passion and think they know more about disease, drugs and treatment than the doctors. They are often spending more time blaming under staffing for all the problem that goes on instead of getting on the job and doing what they can to help patients under their care.
- Patients who abused the system, demanded treatment, referral and prescriptions. These people not only wasted their time but also increase waiting time for people who need help.
How Do You Think We Can Solve The Problem?
We must save the NHS to help poor people, sick children and people with serious illness living in UK. The reason I am saying this is because the threat of antibiotic resistance and emerging infection is real. If NHS goes private, poor and the needy will find it very hard to survive.
This may not be the best solution, but I have created this with great passion with a mission to help reduce cross infections that now threaten our very existance.
People rush to consult a doctor is when they experience severe pain or when they think they have symptoms that may be potentially serious. I developed a simple tool that will help you differentiate minor from serious illness. I have spent almost six years to develop this and is based on research and understanding the pathophysiology of common illness. I have used the same principle to triage, patients, doctors, and nurses when I worked as a doctor in the hospitals, out of hours emergency care, private healthcare and MOD for almost thirty years.
The tool differentiates conditions that require clinical examination from the ones who do not require any clinically examination. I think it is safe because I have used the same principle over and over again for almost thirty years and never failed to differentiate common from serious illness. Working as a registrar in pediatrics, I have always taught GP trainees this method to help them differentiate sick children they can manage in the community from the ones who they must refer to hospital.
Since walk-in-clinics were established in UK, the number of patients consulting me with complications increased. This was mainly because the nurses are made to follow protocols (algorithms) that often fall apart. The diagnosis, advice and treatment can be wrong resulting in delay to consult a doctor. Nurses who sat in my surgery for twelve days are allowed to examine, request investigation and offer treatment in nurse-led practice or local walk-in-clinic. My tool is designed to reduce visiting these clinics and encourage you to speak or consult a doctor in the hospital when necessary.
 Duty of every doctor is to make sure people who trust and expect good, honest advice get advice that is based on knowledge, experience and not one that is printed in a flow chart. I felt very uncomfortable and sad to see too many mistakes committed by nurses working in the walk-in-clinics and nurse-led practice and some doctors working in the Out Of Hours or Primary care centers (they are also expected to follow protocols).
Duty of every doctor is to make sure people who trust and expect good, honest advice get advice that is based on knowledge, experience and not one that is printed in a flow chart. I felt very uncomfortable and sad to see too many mistakes committed by nurses working in the walk-in-clinics and nurse-led practice and some doctors working in the Out Of Hours or Primary care centers (they are also expected to follow protocols).
The delay in diagnosis or treatment resulted in complications that any experienced doctor would have prevented if the patient consulted them first. This is what is called as “Negligence”. The reason I picked up the or identified problems is because I worked for twenty years in acute and intensive care and so read notes and ask questions. Patients who consult doctors late will never know mistakes have been committed by others unless they complain because it is considered un-ethical for doctors to instigate complaints.
I raised my concern and informed authorities that this practice of allowing nurses to work as doctors with no supervision or formal medical training under supervision is harmful for patients and is un-ethical. Patients access healthcare to speak or consult a doctor and so must be given the opportunity to consult and not advised to consult nurses and offered treatment based on protocols and guidelines.
As a doctor we strive hard to diagnose illness early, offer treatment only when necessary and certainly not inflict pain and suffering.
 This tool is simply, can be replicated and will defiantly help reduce the number of people access NHS, cost and allow more time for doctors or nurses to manage patients who need help. This tool was developed to help reduce cross infections. Doctors (Gps) can contact me via email (srivatsa@doctors.org.uk) to get the link to the software (FREE) or ask me to get the fridge magnets to use by patients and help receptionists and patients organise appointments in the surgery. This will reduce the stress and boost moral of doctors, staff and patient satisfaction.
This tool is simply, can be replicated and will defiantly help reduce the number of people access NHS, cost and allow more time for doctors or nurses to manage patients who need help. This tool was developed to help reduce cross infections. Doctors (Gps) can contact me via email (srivatsa@doctors.org.uk) to get the link to the software (FREE) or ask me to get the fridge magnets to use by patients and help receptionists and patients organise appointments in the surgery. This will reduce the stress and boost moral of doctors, staff and patient satisfaction.
Not many people know how the doctors work and certainly cannot understand how doctors think. Unfortunately, majority of doctors working in the NHS know why the system is failing but are too scared to come out and be open. Doctors (I would not classify GPs to be the best ones to lead the NHS) know how they can help because they are only people who know what goes on inside a consultation room.
I am sure NHS will survive if we (doctors, nurses and patients) can all join hands to help bring in changes. People in power who manage the NHS are more often than not not clinicians and starting the cart in a wrong direction and will certainly fall out from the cliff.
REFERENCE
- Jerome Groopman. How Doctors Think, First Mariner Books 2008
- John Riddington Young; The Hospital Revolution. John Blake Publishing
- Kadiyali M Srivatsa, Preprinted assessment sheet. Qual Health Care 1996
- Medical Ethics – Do No Harm (Video)