The National Health Service (NHS) Act was promised in the Labour landslide election of 1945, passed into law in 1946, and the service itself launched in 1948: a non-contributory comprehensive service making all forms of medical, dental and nursing care, in hospitals or in the community, available free to the whole population, paid entirely from central government funding. I qualified from St. George’s Hospital in London four years later, and will retire from full-time clinical practice in 1988; the NHS allowed me to do my own work and refer my patients to the full range of specialist services during an entire working lifetime, without ever having to collect a fee. Several generations of British doctors have followed, with essentially the same historically novel experience.
We have come a long way since then; there have been huge changes in the work and effectiveness of medical care, and exponential growth in medical science which will require even bigger changes in the future. If advances in medical science are to be available for all of the people, the principles on which the NHS was founded must be both restored from their present shorn condition, and extended in entirely new directions. The NHS is under attack as never before, its enemies confident that medical care can again become a commodity on the market, many of its former friends confused and capitulating. The whole world has entered a dangerous time, perhaps most dangerous of all in our own destabilizing society.
Some Illustrative Autobiography
All history must be selective, and therefore judgmental. Its contemporary actors, by living through one set of experiences, are denied others. Like everyone else, my assumptions derive from my own background, experience, the books that I read and the books I avoided, and my readers deserve to be warned what these were.
I was what Americans call a ‘red diaper child’, my mother in the Labour Party, my father in the Communist Party, our home among other things a transit camp for anti-Fascist refugees from Austria, Germany and Italy. Both my parents were doctors, my father a GP recruited by the South Wales Miners’ Federation to help them in a dispute with general practitioners in Llanelli (a redleg?) who later went off to Spain as a surgeon for the International Brigades. Unlike most medical students in 1947, I knew exactly what I wanted to do before I left school; to become a general practitioner in a coal-mining community, because to me that was the highest possible ambition. Like others of that immediately post-war generation, I also felt unjustly spared. My survival was, quite possibly, accidental. Had I been born one year sooner, I might have died in the war, and therefore felt permanently bound not merely to enjoy the peace, but to win and defend it; and not just any peace, but precisely the peace that was won at that time, against Fascism and for a new era of the Common Man, as we still said in those days.
After qualifying in 1952 and disenchanted with teaching hospitals, I sought ‘real life’ as a House Physician at Kettering General Hospital in the East Midlands, just as general practitioner (GP) surgeons in provincial hospitals were beginning to be replaced by professionals. All routine and much emergency surgery in Kettering had always been done by GPs, helped once a week by a part-time consultant who travelled 100 miles by rail from London. About six months previously, one of the GP-surgeons had been presented with a young woman with acute intestinal obstruction, a condition easily reversed by early surgery but otherwise rapidly fatal. He opened the abdomen, to find multiple obstructions by scarring from Crohn’s disease. He excised four or five segments at several points along the seven metres of small intestine, leaving the loose ends to be reconnected. Then his troubles began; which end belonged to which? Never having met this unusual condition before, he had waded into the macaroni without planning his return. In those days emergency surgery was still regarded by patients as a gamble with death. If he had confidently reconnected the tubes as best he could, praying he hadn’t created any collisions, dead ends, or inner circles, he would probably have been acclaimed whatever the outcome. Being a man of integrity, he persuaded his GP-anaesthetist colleague to keep the patient unconscious for what turned out to be four hours with a small coppice of metal clamps splayed out from the incision, telephoned the London consultant, and waited for him to come up by the next train to sort it all out. Remarkably, the patient survived. It was the last anecdote of a closing era of GP surgery; the professionals put an end to all that, and not before time.
The General Hospital served two distinct catchment areas: on one hand, the pleasant market towns of Kettering and Wellingborough and their surrounding countryside, with deeply rooted populations of middling provincial gentlefolk and workers in farms, breweries, railways, shops and light industry; on the other, the steel manufacturing town of Corby, with a population largely imported from Glasgow. From Kettering we had people generally at an early stage of illness, with helpful, informative letters from their GPs, who often visited the wards or at least telephoned to see how their patients were getting on, and made use of the x-ray department and laboratory to investigate patients themselves before referral. From Corby we received patients with gross end-stage disease, and hastily scribbled notes from their GPs:
Dear doctor,
Billy Briggs, 22 Tipslag Terrace, Corby ? acute abdomen (or chest, heart, or whatever), please admit.
Yrs etc.
Hearts sank when requests for admission came from Corby. They were usually about some medical crisis, often avoidable by earlier diagnosis and appropriate action. The Corby and Kettering GPs seemed to work, as their patients lived, in different worlds. It was my first introduction to the divisions of medicine corresponding to the two nations of British society.
My boss was a bachelor who ran an Austin-Healey sports car, and endlessly complained to his junior staff about his poverty and sufferings under the NHS. I earned £250 a year looking after 20 men, 20 women and 16 children on acute medical wards, on call 24 hours a day, without right to any evenings or weekends off for six months except those personally wheedled from the boss. We differed about the NHS: he believed it would end enterprise and reward sloth, I thought it was the best thing that could have happened for the future of medicine. When he went off for the weekend he would fix me with his pale blue eye: ‘Hart: when I come back on Monday I don’t want to find the beds filled with rubbish. Old men with chronic bronchitis belong in Local Authority Part III accommodation, not this hospital.’ Some old man living alone with advanced smoker’s lung was sure to tip into pneumonia, and his GP, rightly acting as advocate, would press for admission. Though squalid dormitory geriatric accommodation did exist under Part III of the Insurance Act in what had been the Kettering workhouse, it was not bad enough to deter a queue to get in. The real choices were between solitary death at home, or a hospital bed with warm nursing, antibiotics (all requiring injection in 1952), and a good chance of recovery. That was my introduction to contradictions between what doctors were interested in and what mattered to patients.
I asked for a reference at the end of my six months, which read as follows: ‘Dr Hart has performed his duties as a House Physician adequately during the past six months.’ At the time this seemed faint praise, but only later did I realise it conveyed the same lethal message to any experienced medical employer as Hamlet’s note on his journey with Rosencrantz and Guildenstern; my introduction to the 18th Century structure of servility and patronage endured by all doctors for some of their lives, and by many for all of their lives.
My junior hospital career was therefore on course for self-destruct, postponed for a few more months by a consultant chest physician who persuaded me to work for him as registrar at the Watford Chest Clinic on the outskirts of London, dealing almost entirely with tuberculosis, then still a common cause of death. I was not properly trained for such responsibility, but the previous man in the job was an alcoholic with drug problems, and no other applicant could be found. The clinic was responsible for tuberculosis patients on the wards of a local hospital which had been a workhouse until 1948. The workhouse master and matron still lived in an elegant residence within the walls, waited on by high-grade mentally defective or so-called morally defective inmates. The barrack-complex contained geriatric and chest wards for sick people, as well as dormitory accommodation for the workhouse inmates who, though liberated by repeal of the Poor Law and advent of the Welfare State, had nowhere else to go. Men lived at one end of the building, women at the other. Most were old people without either money or relatives able to look after them, but there were also mentally or physically handicapped younger people, and several young homeless families. Young or old, married, widowed, or single, males over seven years of age were separated from females except at strictly enforced visiting times. The work was interesting but uncomfortable, not because of the Dickensian surroundings but because I knew I was under-trained. Sink or swim, I learned as I went along; I swam, patients sank.
Just before the lethal reference could catch up with me, I was saved and diverted prematurely into general practice in the wrong place. At the end of 1952 I was chatting to an old Irish GP, Dr Henry Blaker, in a corner dairy in North Kensington. He had retired from a lifetime of work for the Indian Medical Service in Calcutta, to buy a practice from an old colleague, Dr Sweeney, in the slums of North Kensington, with about 2,000 registered patients. His sight was failing from cataracts and he was no longer able to drive, doing his home visits on foot or on the underground. On hearing I was a Cambridge graduate, a fact which impressed him more than me, he asked me to join him as an equal partner starting tomorrow. Only later did I realize how exceptionally just he was; then even more than now entry into general practice, or into almost any other medical job, was difficult, and many established GPs took full advantage of this to exploit their younger colleagues with grossly unequal partnership contracts. Postgraduate experience before starting practice was still an optional extra generally reserved for entry into ‘practices of the better type’. North Kensington was Corby not Kettering country, and even the scanty hospital experience I had seemed much more than my local colleagues expected. Under personal pressures which are irrelevant here, I took the job.
Urban Industrial General Practice in the 1950s
The surgery was in what had been a large corner pub in Clarendon Road, off Holland Park. The area is now gentrified beyond recognition, full of media persons and croupiers at the Stock Exchange, but then it was the edge of one of the worst slums in London, stretching from the bottom of Notting Hill in the south, to Harrow Road and the Grand Union Canal in the north. The pub was all elaborately decorated plaster cornices, frosted glass, and engraved mirrors still advertising various ales, stouts, porters and whiskys. Dr Blaker’s surgery was in the saloon bar, the waiting room in a narrow adjoining room previously used for off-licence sales. It was nearly always full of people waiting to get in, often with more standing in the street, sometimes in the rain. Patients entered the consulting room at one corner, stepped down from the raised area previously behind the bar counter, and sat in front of an enormous oak desk covered with wooden boxes, books, urine test glassware, and unopened copies of the British Medical Journal. When I eventually sorted this out, I found one of the boxes contained a full set of equipment for post-mortem examination, with bone saws and knives of every size and description. A small working area of desk was cleared in front of the doctor’s swivel chair. Behind him was a threadbare printed fabric screen, folded and apparently rarely used. Behind this again was a low divan couch covered in American cloth and stuffed with horsehair, much of it bursting out through ulcers and abrasions acquired in forty or fifty years of combat. On the wall to his right was a large white semicircular washbasin with a single brass cold water tap, an amenity added a few months previously; Dr Blaker warned me not to pee in it, as some previous locums had done. Next to this was a metal stand with a china bowl and ewer, now redundant but, like the junk on the desk, kept on standby in case the 19th Century returned, a not unlikely event to any thoughtful observer. This time-warped impression was strengthened by a glass fronted cupboard set in the wall of the waiting room, still full of dusty medicine bottles waiting to be collected by patients whose names could still just be made out on the elegantly scripted labels. Apparently Dr Sweeney had done his own dispensing, and when the practice finally gave up competing with the local pharmacy this cupboard was simply locked and left as it stood!
There was no receptionist, so patients’ medical records, the small pocket envelopes devised in 1916 for the Lloyd George Act and still used by nine out of ten English GPs, were housed to the left of the great oak desk in a nest of wooden drawers. Virtually the only entries ever made were of medicines prescribed, but occasionally there would be a brief diagnosis (‘asthma’, ‘fractured femur’, ‘neurotic’) without any of the evidence on which the diagnosis was based. Useful clinical information, if any, was confined to hospital correspondence, folded and pushed into the record envelope in a more or less randomly ordered and increasingly tattered bundle.
Twenty to thirty patients came each morning, about the same number in the evening, and between these two sessions I was supposed to fit in about 15 house calls. There were nearly always two or three visits left to do after the evening session, together with any late calls. I would finish by 7.30 if I was lucky, by 9.00 if I was not. I did all the night work for that first year.
One year to the day after I started, without warning or discussion, I found a note from Dr Blaker on the desk to say he had retired and the practice was mine. I took a partner of my own age and we built up the practice to about 3,000 when I left in 1957 to resume my interrupted hospital training, this time on the children’s wards at Hammersmith Hospital. Workload steadily fell, reduced by good practice organization, employing a receptionist and dealing with the underlying causes of such clinical problems as were soluble, rather than sidestepping them with symptomatic treatment. When I left the practice, we often saw only ten or twelve patients at each session, despite a much larger population at risk.
South Wales in the 1960s
After another three years of junior hospital posts and some experience of epidemiological research, first with Richard Doll and later with Archie Cochrane, in 1961 I finally reached my original goal, a single-handed general practice in a small coal-mining community in the Afan Valley in South Wales. The daily consulting rate in Glyncorrwg was roughly the same as when I started in London: 20 to 30 patients at the morning session, the same in the evening, 12 to 15 home visits, for about the same number of people at risk. The time available for each consultation was 5 or 6 minutes, slightly more than was found in a large study of practices in Aberdeen ten years later, (Buchan, I.C., Richardson, I.M., ‘Time study of consultations in general practice’. Scottish Health Studies no. 27. Edinburgh: Scottish Home & Health Department, 1973.) but less than the average 8.25 minutes found in the most recent survey of GP workload in 1986. (‘Survey of GPs’ workload’, British Medical Journal 1987, 294:1241.) Unlike my London experience, improved practice organization had little effect on workload; the reserve of unmet need seemed inexhaustible.
The squalid conditions of industrial working-class practice I met, first in London and later in South Wales, were incompatible with the standards of clinical medicine taught in medical schools, denying self-respect and limiting the imaginations of GP and patient alike. They were essentially the same as those pilloried by Collings(Collings, J.S., ‘General practice in England today’, Lancet 1950,i:555-85) in his classic report in 1950 on British general practice. Thirty-four years later Eric Wilkes, Professor of general practice in Sheffield, described the same squalor in 1984 in a despairing paper entitled ‘Is good general practice possible?’ (Wilkes, E., ‘Is good general practice possible?’, British Medical Journal 1984; 289:85-6.) . British general practice has changed in my lifetime, but very unevenly and very incompletely. It has changed least of all in the old areas of heavy industry, where the real wealth of this country was originally made, and where poverty and unemployment are now most miserably endured.
General Practitioner and Referred Care
Having worked a lifetime in general practice, that is the point from which I see the NHS as a whole, and the people it serves; a close underview from where the action begins, rather than an overview from hospital specialism where some of it ends, or from the outer space of a university library.
To an extent unique in Western Europe and North America, the British medical profession is and has for well over 50 years been divided into two easily defined groups, with little overlap: GPs responsible for registered lists of patients, who care for them only in their own homes and communities; and consultant specialists responsible for all hospital work, assisted by young doctors in training (most of whom later become GPs), who only see patients on referral from GPs. GPs therefore remain generalists, whose real specialized skills are based on familiarity with a specific local population. All other levels of the NHS rest on general practice; the quality, efficiency, and effectiveness of specialists are limited not only by the resources made available to them by the State, but also by the quality and completeness of GP care.
The National Health Service created, and was designed to create, a dramatic improvement in both the extent and the quality of care by specialists in hospitals. It also suddenly extended GP care from the minority of male manual workers covered by the old Lloyd George Insurance Act, to the entire population. It vastly increased the accessibility of general practice but did nothing, and was not designed to do anything, to improve its quality. Clinical medicine in British general practice did improve between 1948 and 1967 (the first important structural reform of NHS general practice), but not at anything like its pace of improvement in hospital care. Nor were improvements selective for those social and geographical areas most in need of them. In general, the quality of all medical care, and particularly of GP care, was lowest where the needs of the population were highest; what I later described as the Inverse Care Law. Neighbourhoods with the worst health inherited the worst traditions, expectations and resources, and were least competitive in the market for well-trained, innovative young doctors. General practice remains an area of relatively poor performance, falling short even of its traditional task of meeting the immediate demands of patients for care of symptomatic illness; it is better, much better, than it was, but still far below what it should be. General practice is even now only beginning to accept its huge future potential for effective health conservation, through which its impact on the health of the general population could be greater than anything possible through specialist care in hospitals.
‘The Health Service is Hospitals‘
Most politicians, media persons, or members of the general public, asked for their mental picture of what is central, important, and effective in the NHS, will describe something going on in a hospital. For most people, hospitals appear to be virtually the only source of effective treatment for life-threatening or seriously disabling conditions; the job of GPs is to sort out major from minor conditions, referring major ones to specialists in hospitals, dealing with minor ones themselves. Planned government investment in hospitals throughout the land, in their staff, equipment, and buildings, with demand from the whole population limited only by the process of GP referral, was the great leap forward which made the NHS such a huge public success.
Until 1967, there was virtually no investment at all in general practitioner services, except what GPs themselves were prepared to spend from their own pockets. The 1966 Package Deal (also known as the GP Charter) brought some indirect public investment in the form of 70% reimbursement of wages to encourage employment of office and nursing staff, 100% reimbursement of rent for suitable buildings, and incentive payments for group practice. Eventually this almost wiped out two common features of industrial general practice; the seedy front-parlour surgery in the GP’s own home, and the squalid shop on the high street with a half-painted glass front, staffed only by a harassed GP’s wife. It reduced the proportion of GPs working single-handed from 43% in 1952, to only 14% by 1980. This did not always improve access for patients, but did encourage sharing of staff and equipment, and placed some limit on the idiosyncratic behaviour of GPs. Even this investment was not fully taken up. GPs are now entitled to claim 70% reimbursement of office and nursing staff wages up to two Whole-Time-Equivalent (WTE) staff for each GP. For the past ten years the actual number employed has stuck around 1.1-1.2 WTE per GP, and only about 15% employ their full entitlement; (Hart’ J T , ‘Practice nurses: an under-used resource’, British Medical ‘ Journal, 1986, 290:1162-3.)most GPs evidently don’t think they need a larger team.
The most important feature of public investment in general practice, however, is that it is neither planned nor plannable. Though GPs now accept some public investment, they are not publicly accountable, except in the narrow and negative sense that they are answerable for complaints. General practice has for seldom-considered historical reasons become a public service privately administered. GPs are independent contractors with government, to provide a public service on their own initiative, with little public control, all of it negative. Even within the narrow limits set by the maximum resources available through the present GP contract, quality of service depends on autonomous decisions by GPs.
Imagine the state of our national road network, if it were financed by a multitude of turnpikes, the quality of each stretch depending on local owners and local expectations; a few miles of motorway, suddenly replaced by a three-lane A road, then a narrow, rutted, unpaved lane, then another mile of motorway, and so on, each depending on the interest and integrity of its owner. It would be an inherently corrupt situation, since whatever he spent on his stretch of road he would be unable to spend on himself or his family. It would be cheap, and occasionally charming, but ineffective as a transport system. For the same reasons, general practice is also cheap, occasionally charming, and, if its task is so far as possible to maintain the health of the whole population, ineffective.
1935-1970: An Age of Optimism
Aneurin Bevan‘s bold nationalization and expansion of hospitals coincided with a worldwide wave of optimism about the effectiveness of medical science, and the feasibility of delivering it to all of the people.
The 35 years from the discovery of sulphonamides in 1935, the first antibiotics suitable for mass use by non-specialist doctors, were a golden age of uncritical faith in the social value of applied medical science. This began to collapse around 1970, with a general mood of radical criticism among young people, together with the beginnings of doubt and retreat from the commitments of the Welfare State and the social contract built on the double victory of 1945, the war and the Labour landslide election. Criticism of medical activity at all levels, focused particularly on high technology care in hospitals, has persisted ever since, both from ‘Left’ and from ‘Right’ perspectives.
Source of figures: Derived from Registrar General’s Decennial Supplement, England & Wales 1931, and Registrar General’s Statistical Review of England & Wales, various years. Figures reproduced from ‘Disorders which shorten life’, OHE 1966, by kind permission of the Office of Health Economics, London.
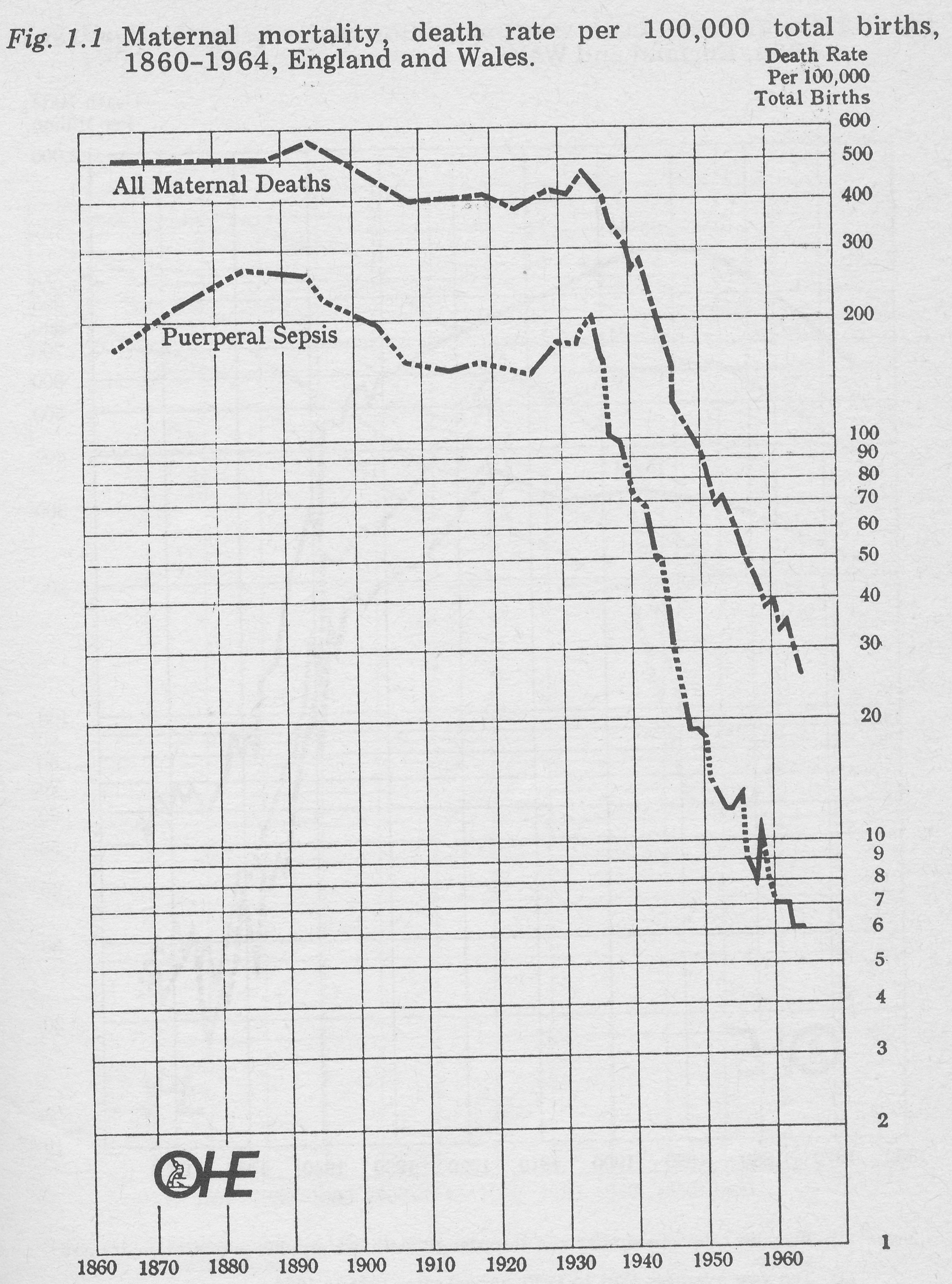
Fig 1-1 Maternal mortality, death rate 1860-1964, England and Wales.
Note: (1) Ten year averages 1861 to 1890, five year averages 1891 to 1930, annual rates 1931 to 1964. (2) Logarithmic scale.
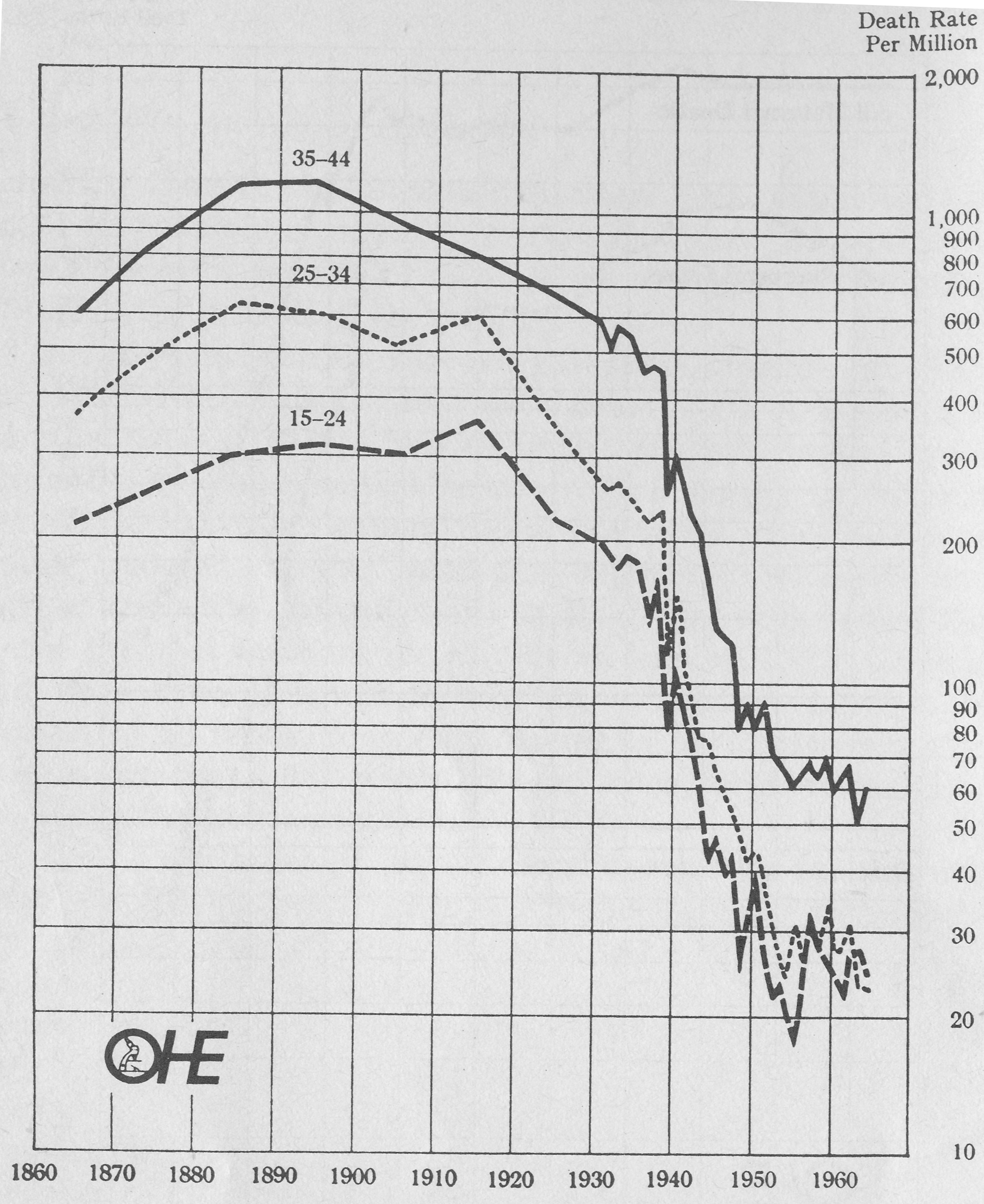
Fig. 1.2 Pneumonia, death rate per million males living, by age, 1861-1964, England and Wales.
Note: (1) Females rates are similar and in order to facilitate graphic presentation are not shown.
Ten year averages 1861 to 1930, annual rates 1931 to 1964. Logarithmic scale.
There is little doubt about the starting date for this era, which more than most historic turning points derived from precise technical as well as less easily defined social and political change. Dramatic effects on valid indicators of disease susceptible to sulphonamide treatment are shown in Fig. 1.1 for death-rates of women in childbirth (maternal mortality), (Loudon, I., ‘Puerperal fever, the streptococcus, the sulphonamides, 911-1945’, British Medical Journal 1987; 295:485-490) and in Fig. 1.2 for death-rates from pneumonia in young men.
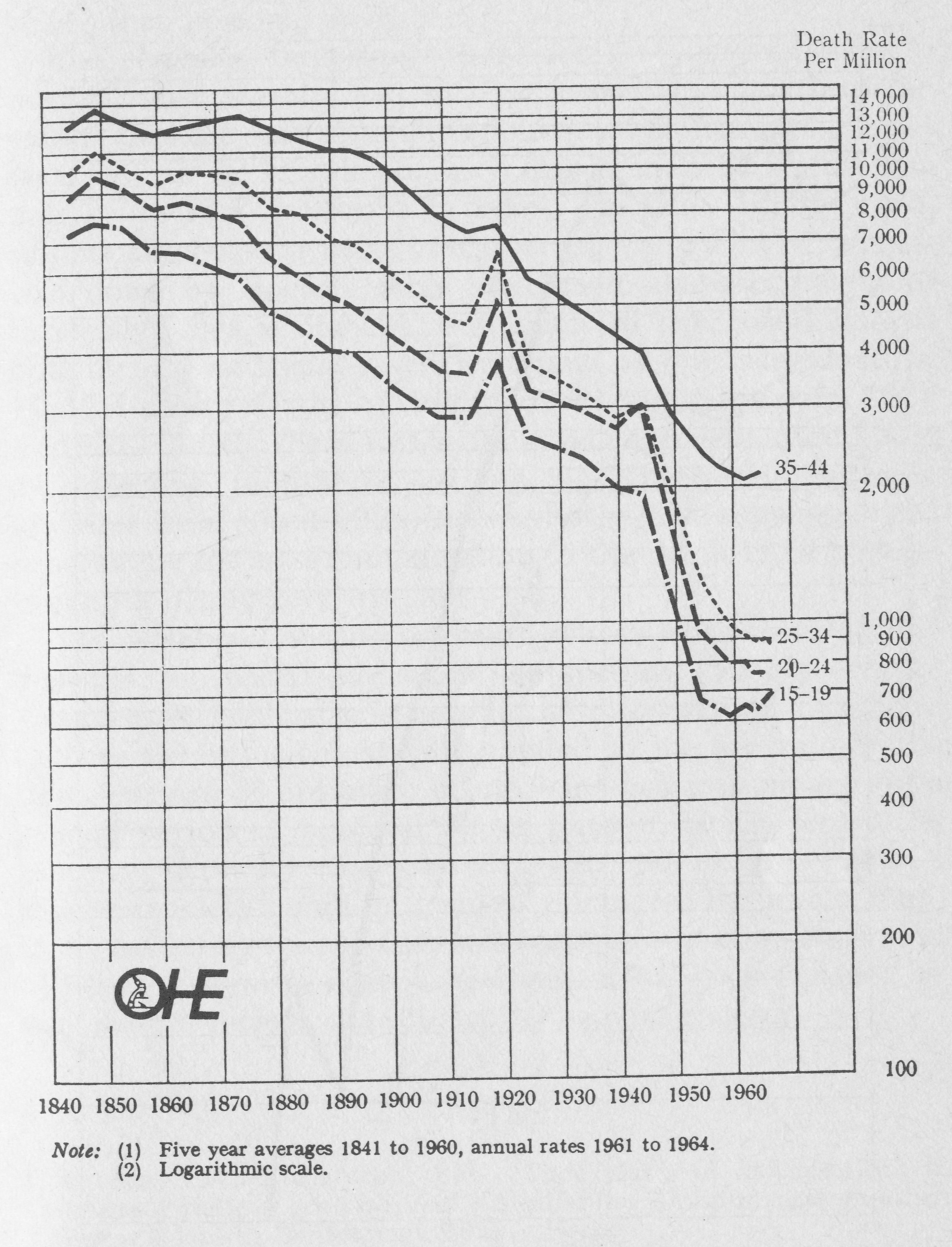
Clearly something dramatic happened in the mid-1930s to two common causes of premature death, but it is important to remember that this advance in effective treatment occurred against a background of steady improvement in death rates from all causes, which seems to have started around 1870 (Fig. 1.3), with full industrialization of the British economy, and the beginning of intensive rather than extensive exploitation of industrial workers. This improvement in health was probably caused mainly by improved nutrition, education, and housing, and by reduced occupational risks (in that order of importance), all of which have bigger effects on health than personal medical care.(McKeown, T., The role of medicine, Oxford: Blackwell, 1979.)
Fig 1.3 Death rates per million living from all causes, by age, 1841-1964, England and Wales.
Source: Registrar General’s Statistical Review, Part I. Figure reproduced from ‘The lives of our children: a study in childhood mortality’, OHE 1962, by kind permission of the Office of Health Economics, London.
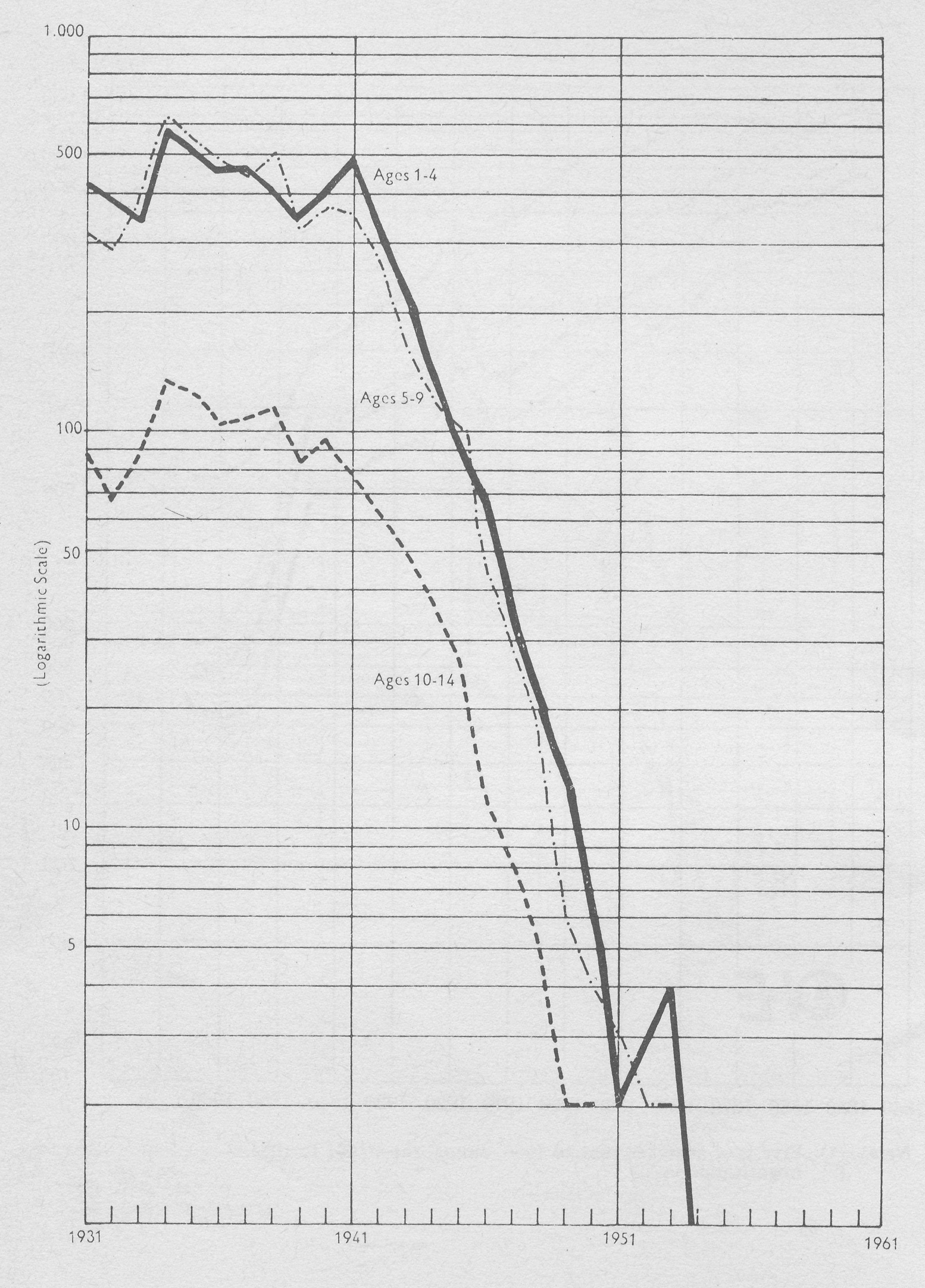
It is equally important to remember that advances in medical science only lead to improvements in health to the extent that they are generally applied; sulphonamides did not save women in childbirth or young men with pneumonia unless doctors prescribed them. On the other hand, sulphonamides were toxic in high dosage, and a lot of damage was done by doctors who used them inappropriately or carelessly. This is obvious, but seems to have been ignored both by pre-war Ministers of Health and by practising doctors. Fig. 1.4 shows deaths of children from diphtheria from 1931 to 1961. Clearly there was a dramatic improvement in 1941; an effective diphtheria vaccine had been commercially available from about 1922, but was not applied as an organized programme for mass immunization to the whole child population until nearly 20 years later.
The NHS is a social construct, whose advance or decline depends on social ideas and competing social pressures. Advances in medical science like the discovery of diphtheria vaccine are not automatically applied to the general population. The age of optimism in medicine was just one part of a general period of post-war liberal illusion, which denied the value or necessity of social struggle, and imagined that a classless society could be painlessly achieved by ‘levelling up’ in a consumerist, capitalist and corporate nation. That kind of liberal optimism died in Vietnam. It has been replaced by strategies of retreat, the subject of the next chapter.