The late 1960s was a time of ideological confusion when the idea of social progress generally lost the association with science it had in the 1930s. The medical age of optimism began to seem an age of credulity. In 1971 Cochrane (Cochrane, A.L., Effectiveness and efficiency, London: Nuffield Provincial Hospitals Trust, 1971.) was the first of a series of authors presenting fundamental criticisms of the theory, practice and profession of contemporary medicine in Britain and North America (Powles, J., ‘On the limitations of modern medicine’, Science,Medicine and Man 1973; 1:1-30; Fuchs, V.R., Who shall live?, New York: Basic Books, 1974; Cochrane, A.L., ‘1931-1971: a critical review with particular reference to the medical profession’. In, Medicines for the year 2000, pp. 1-11. London: Office of Health Economics, 1979.) which were rapidly accepted by an unusually wide range of opinion-formers from both ‘Left’ and ‘Right’ traditions. In its most popular form, and with an irresponsible use of evidence setting it apart from the medical pioneers of this trend, it was presented by Ivan Illich in his book Medical nemesis, (Illich, I., Medical nemesis: limits to medicine, London: Marion Boyars, 1976.) which sold over 3 million copies worldwide. He accused doctors of expropriating the personal right of patients to control their own health, from a combination of greed and intellectual arrogance. He accused the medical profession of being the main danger to public health, as he had pilloried teachers as the main enemies of education in his previous book Deschooling society. Illich went to extraordinary lengths in pursuit of his medical enemy; here is a sample:
Medical civilisation tends to turn pain into a technical matter and thereby deprives suffering of its inherent personal meaning. . . Culture makes pain tolerable by interpreting its necessity; only pain perceived as curable is intolerable.
Like any intellectual fashion achieving wide influence, Illich’s argument used some elements of truth, though nearly all his evidence was derived from medical sources, suggesting that medical science was more self-critical than his theory allowed. It still seems extraordinary that so weak an argument was taken so seriously, even in authoritative medical journals like the British Medical Journal and the Lancet, which devoted pages of self-doubt to an assault which would once have been brushed aside as a trivial impertinence. Ten years later, the Lancet still has space for random reflections of Chairman Illich, of a banality too complex and pretentious for analysis either as prose or scientific argument. (Illich, I., ‘Body history’, Lancet 1986; ii:1325-7.)
The most credible explanation for this seems to be that many intellectual leaders of the profession were already looking for ways to justify their own retreat from the full social implications of making all important advances in medical science available as a human right to the whole population. Assured of sponsorship, doctors still wanted to provide effective skills whatever the cost; but as the State set limits on its sponsorship for innovative medical science, the profession discovered new doubts about its mass application, though medical science itself was unquestionably in better shape than ever before.
Common to all these intellectual critics were the following beliefs:
- That medical care has contributed little to improvements in health or expectation of life compared with nutrition, education, and conditions of life and work.
- That doctors and their public have expected too much from attempts to restore health by surgical or biochemical excision or substitution, which now incur increasing and eventually prohibitive costs for diminishing returns.
- That personal medical care should therefore retreat to a more modest role in curing seldom, relieving often, and comforting always.
This currently dominant set of ideas I shall refer to as the Liberal Critique, since it has all the historic qualities of Liberalism: scholarly backing, humane intentions, appeal to both Left and Right intellectual radicals without embarrassment to either, and ability to interpret defeat as victory. This is a savage description, but anger is justified; not because these three conclusions are untrue, but because of the increasingly obvious social and political context in which only these truths have been proclaimed, while others, less convenient to this scoundrel time, have been forgotten. The Liberal Critique has disarmed professional resistance first to revision, then to destruction of the post-war social settlement of which the NHS was an important part.
Does Medical Care Matter?
The view that medical care contributes less to health than nutrition, education and conditions of life and work is not new or original. It is difficult to think of any important innovator in medical thought who has not held this opinion. If you take a thousand people and lock them up, their first thoughts are of food, not doctors. The more primitive life is, the more important food and shelter become, but a society that is becoming more rather than less civilized gives more not less priority to education and health services, in that order. Even in specialized hospital medicine, outstanding innovators like Paget, Osier, Albutt, Pickering and Platt always conceded the pre-eminent role of nutrition, education, and living and working conditions, compared with the salvage work they performed. Like pioneers in any field, they may sometimes have expected too much from attempts to restore health by surgical or biochemical excision or substitution, but again this is not new, and the general public, encouraged by press entertainers, has been far more credulous than its doctors. In Britain more than most countries there has been a vigorous tradition of medical scepticism ever since the Second World War, probably because until recently nearly all doctors were in a free public service rather than trade, and therefore had fewer incentives to deceive either themselves or their customers.
The novel feature of the Liberal Critique is not this rediscovery of the dominant importance of environment for health, and our still limited ability to cure illness, but its emphasis on a diminishing role for medical care; not only the alleged pettiness of its actual contribution, but of its potential contribution in the future. The question would have been easier to understand around 1905, when the only major diseases in which medication influenced outcome were syphilis and heart failure, and effective surgery was limited to injuries and a few abdominal and obstetric emergencies. The rate of successful clinical innovation, far from levelling out or diminishing, is increasing every year. Seeds of a vast expansion of innovation in applied medical science were sown with the discovery of the structure of DNA in 1953, ‘a revolution in the biological sciences comparable to that in physics earlier this century’. (Weatherall, D., ‘Molecular and cell biology in clinical medicine: introduction’, British Medical Journal 1987; 295:587-9.) Medicine is applied human biology. It took about 40 years for nuclear physics to find a practical application; 34 years after Crick and Watson we are already beginning to see evidence that ‘medical sciences are about to enter the most exciting period of their development’.
Undeniably, basic medical science is advancing with accelerating speed. Practical applications in teaching hospitals, though most of them still depend on basic medical sciences of the pre-molecular era, are already arriving faster than we can assimilate them within present staff resources.
There is no real doubt that these new techniques are increasingly effective. Coronary artery bypass grafts (CABG) are a good example. When they began to be widely used in the United States in the early 1970s, thoughtful doctors had mixed feelings. On the one hand, CABG relieved the symptoms of chest pain from coronary heart disease (angina) almost completely in about 70% of cases, and increased survival by about 50% over the first seven years following operation for the minority of patients with angina who have left main coronary artery disease (about 13% of cases), with less than 3% mortality from the operation itself.
CABGs may appear to support the view that effective medical care now incurs increasing and eventually prohibitive costs for diminishing returns, but this is so only if the technique is applied without an overall policy for control of coronary disease. Once-for-all surgical costs for CABG are £2,500-£4,500 at 1983-4 prices, not all that much more than the cost of modern medical care for the expected lifetime of angina patients. (Williams, A., ‘Economics of coronary artery bypass grafting’, British Medical Journal 1985; 291:326-9) The difference in cost, around £2,500, is about the same as the cost of one total hip replacement operation. Surgical costs are more than twice as high in marketed, fee-paid care systems such as that in the USA, so in terms of cost-effectiveness, the case for CABG is stronger in a free public service, where surgeons are paid by salary. Like all new surgical treatments for common conditions, the technique becomes cheaper as it becomes perfected and standardized; the more advanced centres are now well into the next generation of surgical procedures for coronary salvage, coronary angioplasty, an essentially simpler procedure which provides a rebore of the original vessel instead of replacing it, an even safer and much cheaper procedure. These techniques are effective and should be generally available without delay to those who need them, a policy which in no way contradicts the need simultaneously to step up health promotion, prevention and anticipatory care.
One of the saddest recent developments in the NHS is the attempt to supplement inadequately funded NHS heart surgery by getting coronary surgery done privately under contract to the NHS, as my own Health Authority in West Glamorgan has recently decided to do. NHS units are still the sole source of training for the very specialized surgical teams which perform these operations, whether they ultimately work in the NHS or the private sector. Farming the work out to private contractors working for profit accelerates the destruction of the training, research and development facilities on which all progress depends.
Though coronary death rates have fallen in USA, Australia, and New Zealand by about one-third over the same period that CABG has been in wide use in these countries, heart surgery has been estimated to contribute only 4-5% of this reduction. ( Goldman, L., Cook, E.F., ‘The decline in ischemic heart disease mortality rates: an analysis of the comparative effects of medical interventions and changes in lifestyle’, Annals of Internal Medicine 1984; 101:825-36.) It is still not clear why these big falls in coronary mortality have occurred, nor why they appeared first in the USA and Australia, and have hardly occurred at all in Britain and Sweden; on the whole, the most convincing evidence is for a reduction in average blood total cholesterol because of changes in the composition of quantity of fat in common foods, which have occurred in some countries and not others. There is no doubt at all that they do reflect changes in the way people live more than changes in medical care, except insofar as medical advice may accelerate changes in personal behaviour, on a scale sufficient to affect fashion. There has certainly been a stark contrast between the active advocacy of coronary prevention as well as surgical salvage by doctors in the USA, and the passivity of British doctors. (Beaglehole, R., ‘Medical management and the decline in mortality from coronary heart disease’, British Medical Journal 1986; 292: 33-5.) There is still much that is unexplained about coronary disease. Big reductions in coronary atheroma in young men preceded any big shifts in adult eating patterns, exercise, smoking or heart surgery by about ten years. They may at least in part have been caused by contrasts between childhood and adult nutrition in the entire cohort of men born between about 1910 and 1940. ( Marmot, M.G., Shipley, M.J., Rose, G.A., ‘Inequalities in death: specific explanations of a general pattern?’, Lancet 1 984; i:10003-6.; Forsdahl, A., ‘Are poor living conditions in childhood and adolescence an important risk factor for arteriosclerotic heart disease?’, British Journal of Preventive & Social Medicine 1977; 31:91-5.) These questions are important, because molecular biology is going to give us weapons that act upon causal mechanisms in very large numbers of people, rather than the primitive strategy of salvaging advanced disease.
There is no longer any doubt that CABG is a real advantage to patients carefully selected on clinical grounds, or that surgical salvage should have a useful, though relatively small and eventually diminishing part to play in any overall strategy for dealing with coronary disease. This was exactly the (unplanned) sequence followed for rheumatic valvular damage, the principal cause of early death from heart disease before coronary disease began to be common in the 1930s; a rapid but incomplete decline because of changed living conditions, accelerated and completed by surgical salvage. The difference between surgical valve repair or replacement in the 1950s and ’60s, and CABG today, is that free access to surgery on the basis of need alone is no longer expanding for the whole population.
Studies in Sweden suggest that the justifiable annual demand for CABG would be around 300 per million population, if all suitable cases were accepted in the age-range 45-54. Reviewing the provision of CABG in Wales in 1983, the Royal College of General Practitioners found the operation was being offered at 7% of this ideal rate in Wales, and 80% of it in the London (SE Thames) region, after subtracting cases ‘imported’ from other regions, ( Report of a Working Party. ‘Stitches in time’, Welsh Council, Royal College of General Practitioners, 1983.) although male death rates in middle age from coronary disease in the South Wales valleys are about one-third higher than in England and Wales as a whole, and nearly twice as high as in the South East. ( Hart, J.T., ‘The marriage of primary care and epidemiology”, Journal of the Royal College of Physicians of London 1974; 8:299-314.) Unlike facilities for open heart surgery for rheumatic valvular disease, regional availability of CABG is unrelated to need. In the absence of an active policy for preferential development in areas of high coronary mortality, there is a large element of social selection because of the lower expectations and therefore lower effective demand of poorer and less well-informed people, even in a system of free care. There is no evidence that any such policy is currently pursued or planned.
Even if coronary surgery were available in proportion to regional need, no matter how successful it might be tactically, it could not be an effective mass strategy. Without organization of anticipatory care and prevention it only offers a personal short-term technological fix to a small high-risk minority, instead of tackling what is essentially a long-term behavioural problem for the whole population. Though molecular biology may give us alternative solutions, even these will probably have to be applied to whole populations at risk rather than to a few with advanced damage.
The truth is that until we have successful prevention, we must have salvage; if we want to remain a civilized country, both strategies must be pursued, and for everyone. I have yet to meet any well-informed person who, having developed angina uncontrollable by stopping smoking, by medication and by minor restrictions in exercise, does not want a skilled surgical opinion. Whatever their views on grand social strategy, the experts all seem to make intelligent and discriminating use of high technology salvage for themselves and their families, and they still do this through the National Health Service whenever they can. In practice, even within the NHS we already have a two-tier system, in which a minority of well-informed people, and those with unusually energetic GPs, gain access to the best high-technology salvage, while the majority go by default.
In an under-funded public service, as more people rightly make more sophisticated demands, waiting lists lengthen, and more people have to seek treatment privately. This is only beginning with CABGs, of which only 0.1% were done privately in 1981, but it is well established for hip replacement, 26% of which were done in the private sector in the same year. New techniques are either introduced reluctantly and inadequately, as with CABG, or in some regions abandoned almost completely to the private sector, as with vasectomy and termination of pregnancy. Using available data from various years from 1981 to 1984, private market penetration had reached 1% for obstetric care, 1.5% for mental handicap, 2% for chronic mental illness, 4% for acute mental illness, 13% for all elective surgery, 35% for long-stay institutional care of the elderly, and 47% for terminations of pregnancy.
Paying More and More for Less and Less
Of course, believers in the Liberal Critique deplore all this. They would like everyone to enjoy the same quality of care as themselves, but (they argue), Britain in its post-imperial state is becoming a poor country, in which painful choices have to be made; to them it is obvious that with limited resources, the first things to go from a shorn public service should be luxury items like high technology medical care. The argument has even influenced people who consider themselves Marxists. Writing in Marxism Today, Dr Steve Iliffe (Iliffe, S., ‘The painful path to health’, Marxism Today 1986; 30:34-8) has come to believe that:
the guiding principles of the National Health Service are no longer workable. . . overall staffing levels should be kept constant. . . budget restraints on health authorities should be maintained. . . principled objections to charges for services should be overruled. . . Medicine is steadily becoming less cost-effective. . . money will come from different directions in different places, ending the pretence of a tidy monolithic institution. If this happens, we will be in debt to the Conservatives for the instability they once inflicted on the biggest institution in Europe outside the Red Army, and also on the traditions of the British Left.
Iliffe gives CABG and total hip replacement as examples of rising costs with diminishing effectiveness. He can hardly deny that these procedures are effective in making thousands of lives enjoyable rather than miserable. As techniques become standardized, costs fall, particularly if they are organized in a non-profit public service. The proportion of our Gross National Product spent on medical care has risen only from 4% in 1949 to 6% in 1981, is still less than any other country in Europe, and almost half that in the USA. The rate of fall of age-specific mortality has, of course, declined as more people reach a healthy old age, and more deaths result from natural senescence, but effectiveness of medical care in improving the quality of life has enormously improved. There is no evidence that this tendency will diminish; on the contrary, the immense potential benefits of advances in basic biological science have hardly been tapped. It has been estimated that 25-30% of hospital beds, and probably an even higher proportion of all NHS spending, goes on care during the last year of life, ( Cartwright, A., Hockey, L., Anderson, J.L., Life before death, p. 79. London: Routledge & Kegan Paul, 1973.) either terminal care or more less unsuccessful salvage. In the light of current medical knowledge, this proportion is too high, but that means an increased investment in care in the community at earlier stages of disease, rather than a reduction in care of advanced disease and terminal illness.
Social Causes of Disease
Believers in the Liberal Critique nevertheless maintain that because in an ideal world each pound spent on better food, housing or education in deprived sections of the population would yield greater health benefits than each pound spent on medical care, public spending should follow the same order of priorities. Granted the unlikely premise (an ideal world), this would be true, and the argument is important.
Although death rates at all ages have been falling ever since 1870, the difference between death rates for the rich and the poor has been widening since the 1930s (Fig. 2.1). Mortality differences for women follow the same trends, but are more difficult to interpret because women are classified by their husbands’ occupations.
Fig. 2.1 Standardized Mortality Ratios (100 = average mortality across all classes) by social class, 1931-81, men 15-64, England and Wales.
| Class | 1931 | 1951 | 1961 | 1971 |
1981 |
| I professional |
90 |
86 |
76 (75) | 77(75) |
66 |
| 11 managerial |
94 |
92 |
81 | 81 |
76 |
| III skilled manual and non-manual |
97 |
101 |
100 | 104 |
103 |
| IV semi-skilled |
102 |
104 |
103 | 114 |
116 |
| V unskilled |
111 |
118 |
143 (127) | 137(121) |
166 |
* Figures have been adjusted to classification of occupations used in 1951. ** Men 20-64 years, Great Britain.
Source: Wilkinson, R.G., ‘Socio-economic differences in mortality: interpreting the data on their size and trends’. In Wilkinson, E.G.. (edA Class and health: research and longitudinal data, London: Tavistock Publications, 1986.
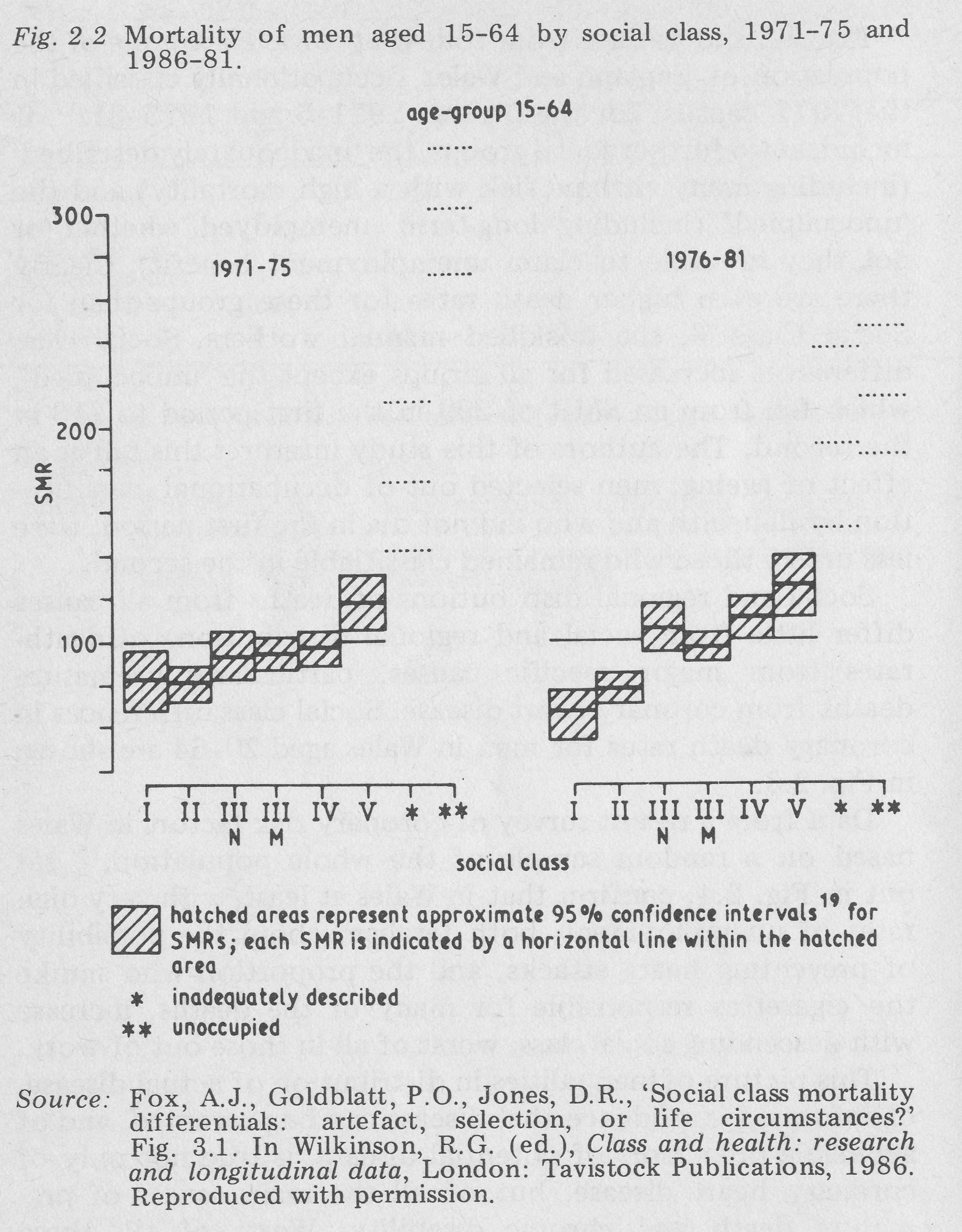
Fig 2.2 Mortality of men aged 15-64 by social class, 1971-75 and 1986-81.
Fig. 2.2 shows data from follow-up of a 1% sample of the population of England and Wales, occupationally classified in the 1971 census, for the periods 1971-5 and 1976-81. (Fox, A.J., Goldblatt, P.O., Jones, D.R., ‘Social class mortality differentials: artefact, selection, or life circumstances?’ In Wilkinson, R.G. (ed.), Class and health: research and longitudinal data, London: Tavistock Publications, 1986.) It includes two further social groups, the ‘inadequately described’ (including many chronic sick with a high mortality) and the ‘unoccupied’ (including long-term unemployed whether or not they are able to claim unemployment benefit). Clearly there are even higher death rates for these groups than for Social Class V, the unskilled manual workers. Social class differences increased for all groups except the ‘unoccupied’, which fell from an SMR of 299 in the first period to 213 in the second. The authors of this study interpret this fall as an effect of ageing; men selected out of occupational classification by ill-health and who did not die in the first period, were less unlike those who remained classifiable in the second.
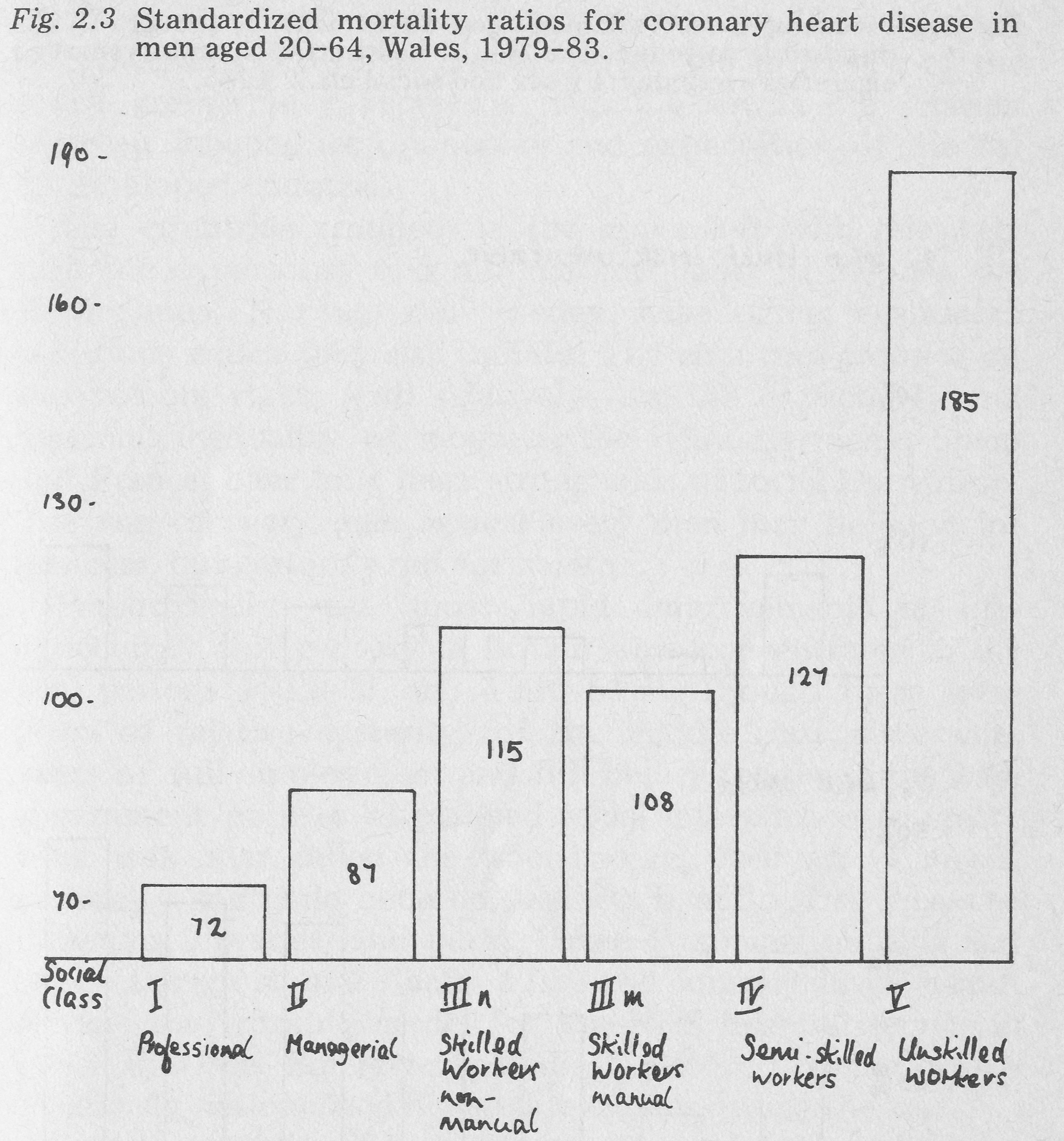
Fig 2-3 Standardized mortality ratios for coronary heart disease in men aged 20-64, Wales, 1979-83.
Social and regional distributions of deaths from all causes differ little from social and regional distributions of death-rates from major specific causes, particularly premature deaths from coronary heart disease. Social class differences in coronary death rates for men in Wales aged 20-64 are shown in Fig. 2.3.
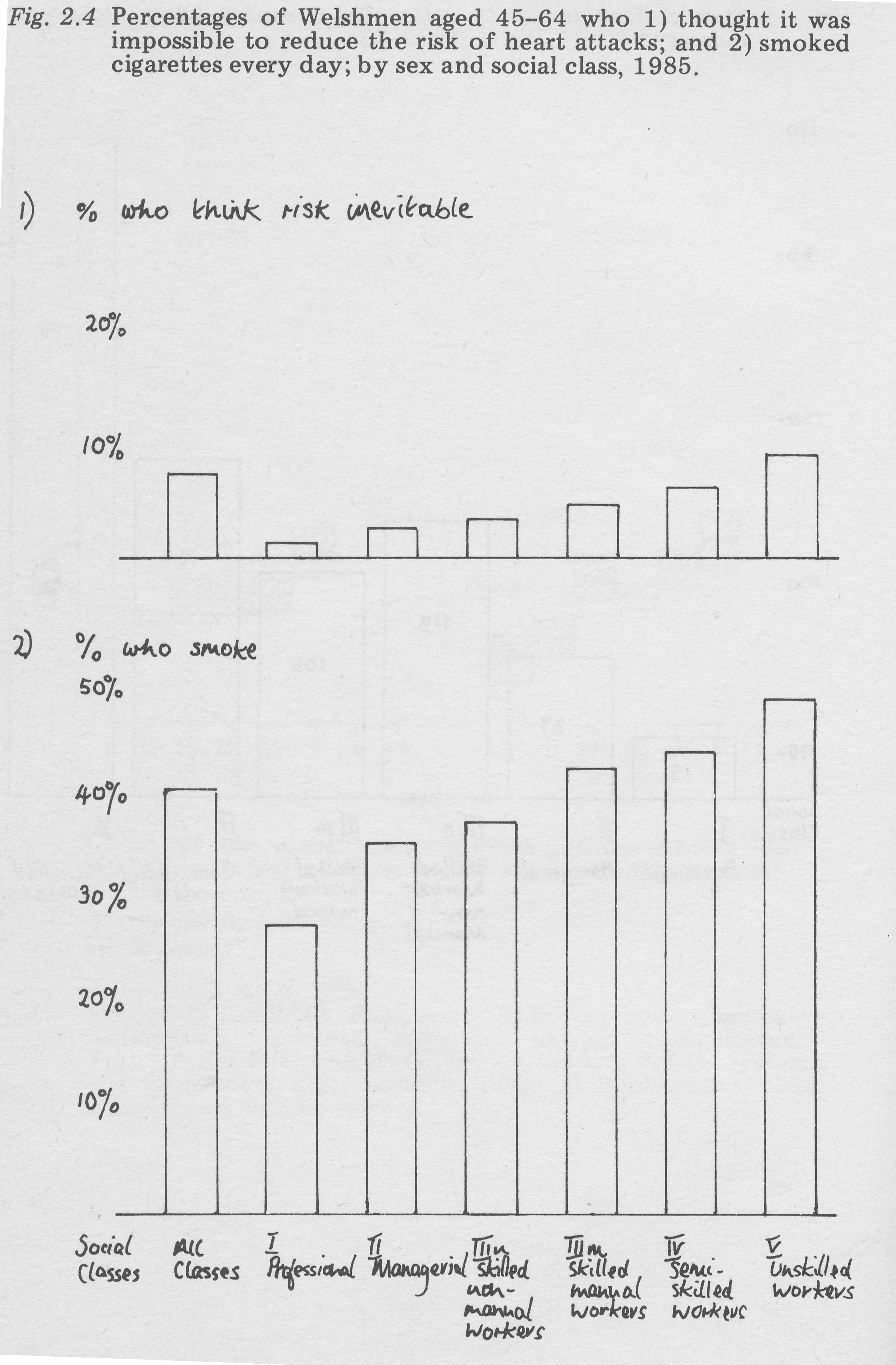
Fig. 2 4 Percentages of Welshmen aged 45-64 who 1) thought it was impossible to reduce the risk of heart attacks; and 2) smoked cigarettes every day; by sex and social class, 1985.
Data from a recent survey of coronary risk factors in Wales based on a random sample of the whole population, (Nutbeam, D., Catford, J., ‘Pulse of Wales: social survey supplement’, Heartbeat report no. 7, Cardiff: Heartbeat Wales, 1987.) set out in Fig. 2.4, confirm that in Wales at least, with very high rates of unemployment, both fatalism about the possibility of preventing heart attacks, and the proportion who smoke the cigarettes responsible for many of the deaths, increase with descending social class, worst of all in those out of work. This picture of inequalities in distribution of actual disease, of informed confidence that disease can be prevented, and of avoidable precursors of potential disease, is true not only of coronary heart disease, but of all the main causes of premature death and chronic disability. Worst of all, these inequalities are increasing. The available evidence was presented in the Report of Sir Douglas Black’s Committee on Inequalities in Health in 1980, powerfully reinforced by a wide range of subsequent research reviewed by Wilkinson, Marmot, Blaxter, Wadsworth and others. (Wilkinson, R.G. (ed.), Class and health: research and longitudinal data, London: Tavistock Publications, 1986.)
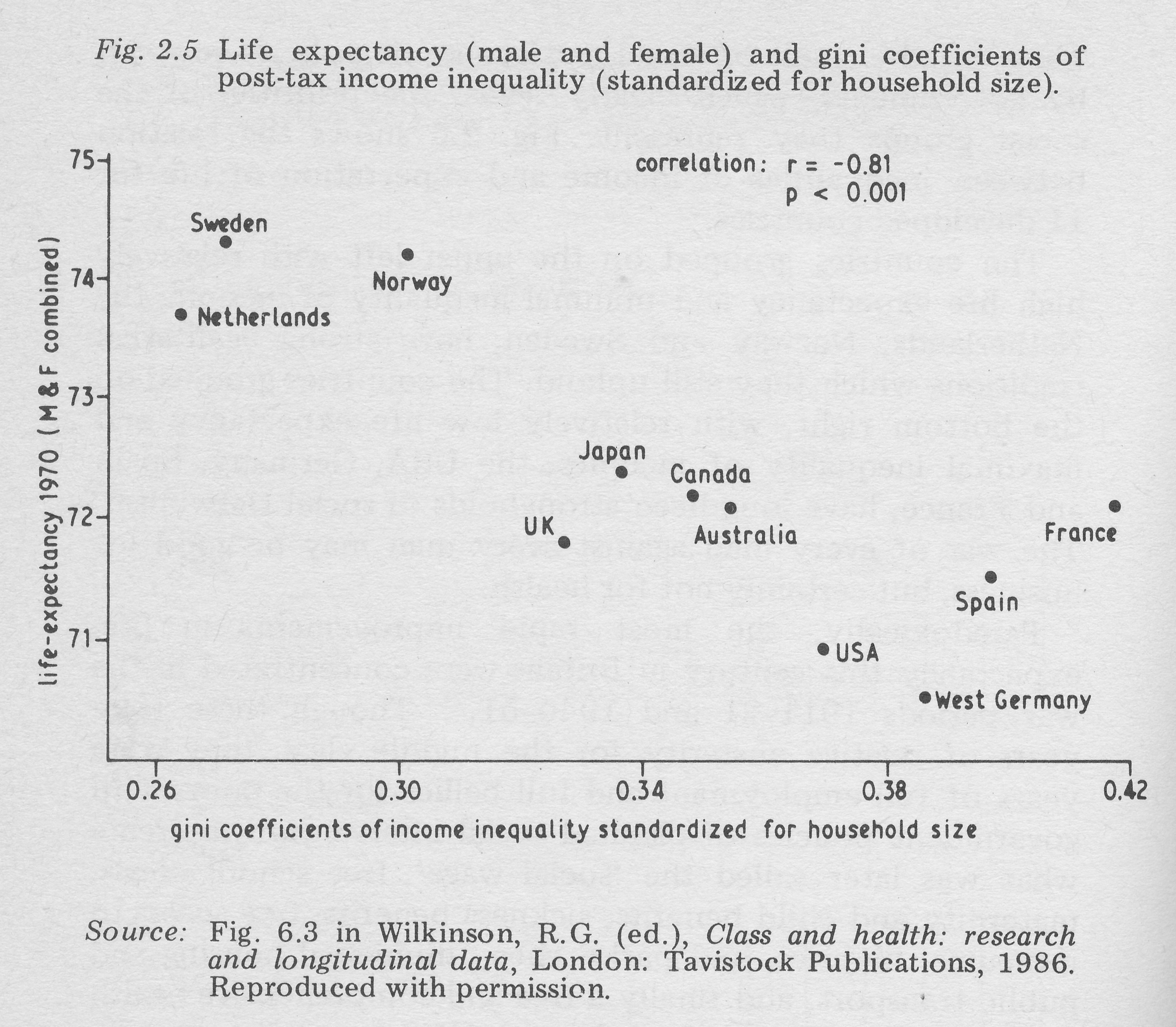
Social inequalities in health are neither just nor inevitable. They are the result of social and economic policies adopted by governments, which clearly reveal the priorities of the social groups they represent. Fig. 2.5 shows the relation between inequalities of income and expectation of life for 11 developed countries.
Fig. 2.5 Life expectancy (male and female) and gini coefficients of post-tax income inequality (standardized for household size).
The countries grouped on the upper left with relatively high life expectancy and minimal inequality of income, the Netherlands, Norway and Sweden, have strong egalitarian traditions which they still uphold. The countries grouped on the bottom right, with relatively low life expectancy and maximal inequality of incomes, the USA, Germany, Spain and France, have long been strongholds of social Darwinism. The war of every man against every man may be good for business, but certainly not for health.
Paradoxically, the most rapid improvements in life-expectancy this century in Britain were concentrated in the war periods 1911-21 and 1940-51. (Winter, J.M. Quoted in Wilkinson, R.G., Class and health: research and longitudinal data, London: Tavistock Publications, 1986. , p. 110.) Though these were years of relative austerity for the middle class, they were years of full employment and full bellies for the poor, with government policies of planned social intervention to create what was later called the ‘social wage’; free school meals, maternity and child benefits, sickness benefits, free access to museums, libraries, and parks, cheap municipal housing and public transport, and finally a free and comprehensive health service; the working model for the NHS hospital service in 1948 was the Emergency Medical Service scheme which effectively nationalized hospital resources during the war.
Investment in a shared infrastructure of free services is a political choice, of proven effectiveness. Before the Second World War, infant mortality in Stockholm varied according to socio-economic group from 14 to 49 per 1,000 live births; today it is below 7 per 1,000 live births, with virtually no difference between socio-economic groups. (Dahlgren, G., Diderichsen, F., ‘Strategies for equity in health:report from Sweden’, International Journal of Health Services 1986; 16:517-37.) Governments, like our own in 1945 or in Scandinavia today, can choose to increase the social wage relative to personal incomes, or they can revert to sale and purchase of these elements of civilization, piece by piece, every man for himself, as Thatcher Conservatism does today.
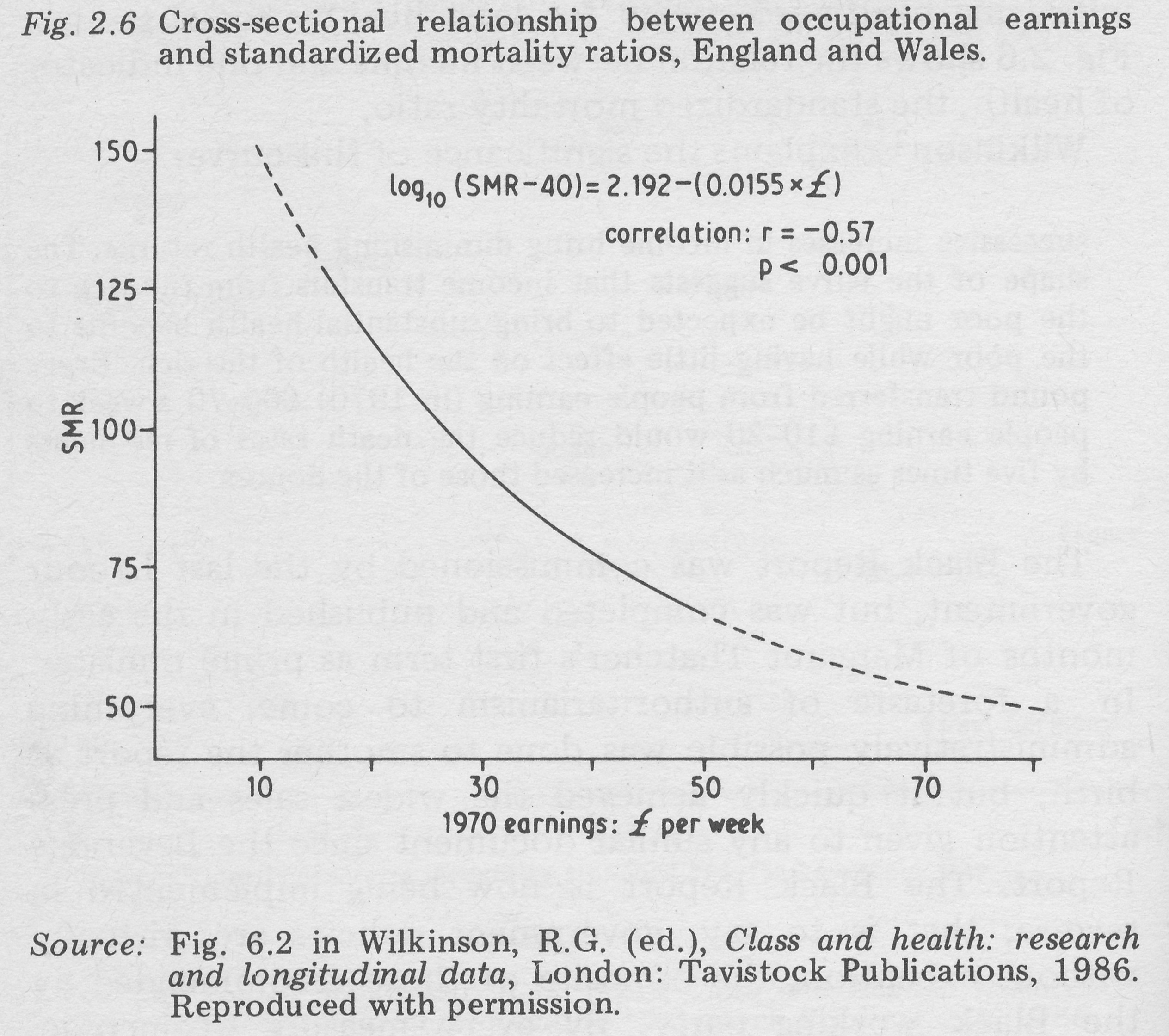
Fig. 2.6 Cross-sectional relationship between occupational earnings and standardized mortality ratios, England and Wales.
Redistributive income policies are another way of improving health selectively for least healthy social groups. Fig. 2.6 shows the relation between income and one indicator of health, the standardized mortality ratio. Wilkinson ( Wilkinson, R.G., ‘Income and mortality’, p. 109 in Wilkinson, R.G. (ed.), Class and health: research and longitudinal data London: Tavistock Publications, 1986.) explains the significance of this curve:
successive increases in income bring diminishing health returns. The shape of the curve suggests that income transfers from the rich to the poor might be expected to bring substantial health benefits to the poor while having little effect on the health of the rich. Every pound transferred from people earning (in 1970) £60-70 a week to people earning £10-20 would reduce the death rates of recipients by five times as much as it increased those of the donors.
The Black Report was commissioned by the last Labour government, but was completed and published in the early months of Margaret Thatcher’s first term as prime minister. In a foretaste of authoritarianism to come, everything administratively possible was done to smother the report at birth, but it quickly achieved the widest sales and press attention given to any similar document since the Beveridge Report. The Black Report is now being implemented in reverse; that is to say, government policies are, virtually without exception, the opposite of those recommended by the Black working party. By every measure of income, education, housing, availability of employment, nutrition, participative sport facilities, nicotine and alcohol dependence, and increasingly by access to sophisticated medical care (curative or preventive), Britain is becoming a more divided and unequal society.
A Strategy for Advance
The first step in devising strategies for more effective, and cost-effective, health services must be to oppose this policy of de-civilization. Scholars seeking solutions within limits set by the de-civilizers deceive themselves, and disarm and confuse what should be, and will become, a previously unimaginable social alliance of professional and public opinion for resumed social progress. Some advocates of the Liberal Critique have had useful things to say, and progressives can learn from them, but the essence of their strategy is retreat; an inglorious abdication from previous beliefs about the potential effectiveness of medical care, the potential value of medical science, the dignity and independence from the market of Medical Professionalism, and the feasibility of real social advance.
Our health services have developed not in an ideal, painless world of armchair social strategies, but in the real, bitter world of injustice consciously and deliberately maintained by real, powerful people who gain from things as they are, in which the distribution of wealth and power is never changed without struggle. Priority investment in social infrastructure, redistributive personal income policies, and higher priority for health service spending rather than preparation for war or reduction in personal income tax, are not rival alternatives. None of them will be pursued by a government which assumes that what is good for the Stock Exchange is good for the nation; all of them would be pursued by a government concerned with the health and happiness of all of the people.
On the other hand, realistic strategies for renewed advance must start from where we are, with the people we have. We cannot devise ideal solutions on a blank page, without regard to where we have come from, or where medical science is going. The content of potentially effective medical care has changed, both because of changes in public health, and because of advances in medical science, requiring big changes in the structure and staffing of care, most of all at primary care level.
We have to consider a set of historical choices, in a way that has not faced doctors since they first began to define their professionalism in the early 19th Century. (Loudon, I.S.L., Medical care and the general practitioner 1750, Oxford: Clarendon Press, 1986. Together with Rosemary Stevens’ book, this is the best detailed account of the rise of British medical professionalism.) If we wish to continue the association of Medical Professionalism with Medical Science, we must prepare to accept solutions outside the limits of professionalism as then defined.