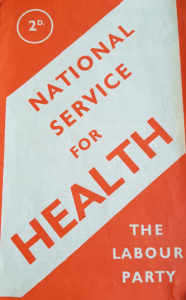
Do we need a State Medical Service? If so, on what lines should it be planned?
This pamphlet summarises the Labour Party’s answers to these two questions, which concern everyone in the land.
PART I IS A STATE MEDICAL SERVICE NEEDED?
Before answering the first question, we must decide what we require of the Health and Medical Services in general. (See Chapter I.)
We must know, broadly, what the existing Medical Service is like. (See Chapter II.)
We can then judge whether the Service, on its present basis, is likely to meet the need, or whether a State Medical Service is essential. (See Chapter III.)
Chapter I WHAT MEDICAL SERVICES DO WE NEED?
Britain’s Health Aim
The aim of the nation’s Health policy can be nothing less than the utmost possible fitness of body and mind for all the people. Full health; We cannot afford to aim at anything less than that; for full health is the greatest asset of an individual, and a healthy population is the greatest asset of a nation.
Health and Government
To achieve this aim we need as good a Medical Service as possible. We need much more than that, however. We need social action to create the conditions under which the healthy needs of the whole people can be satisfied. In truth, there is hardly any activity of government which does not affect health, directly or indirectly. If, through a sound social and economic policy, we can master poverty, we shall thereby do much to eliminate ill-health; for poverty is still the greatest single cause of ill-health. If, by good government, we secure for all good conditions of work, with full employment, and with ample opportunity for leisure and exercise; if, through our public services, the citizen can obtain well-built and well-placed houses, with sanitation, water, clean and plentiful milk and other nourishing food, clean air and as much sunlight as possible, and freedom from injurious noise; then the health of the nation will benefit far more from these causes than from much doctoring. If our economic and social conditions are such that no removable barriers stand in the way of happy parenthood and healthy childhood, then we may reasonably hope that the population, instead of diminishing sharply and progressively, will be kept replenished by a sufficiency of children, well-born and well-nurtured.
The full health that we aim at is to a great extent a consequence of good government.
No agency less universal in its authority than Government can secure for the whole people the conditions necessary for health; and no ill-health in any part of the population can be a matter of indifference to the people’s Government.
The Medical Service that we Need
Besides the various Services which affect health indirectly, we need the direct aid of a Medical Service. That Service should be:
- Planned as a whole, so that there are no gaps in it;
- Preventive as well as curative. It must be equipped for preventing every avoidable damage to the intricate working of body and mind, and for promoting the full flowering of every man’s and woman’s physical and mental strength; it must be positive as well as negative, helping those who are fit to keep fit, and those who are nearly fit to become fully fit. In addition, the Medical Service must provide for the cure of disease, the treatment of accidents, the care of the sick, the relief of suffering, the rehabilitation of the convalescent, maternity care and the medical treatment of children, etc.
- Complete, covering all kinds of treatment required. The Beveridge Report called for a comprehensive Health Service ensuring “that for every citizen there is available whatever medical treatment he requires, in whatever form he requires it, domiciliary or institutional, general, specialist, or consultant, and will ensure also the provision of dental, ophthalmic, and surgical appliances, nursing and midwifery, and rehabilitation after accidents.” (Beveridge Report, 427) This has been accepted in principle by the Government. A service which is to provide “whatever medical treatment” the citizen may require must include the service of a good general practitioner; an all-round service of specialists; good hospitals with enough beds; a nursing service in hospital and, when necessary, in the home; midwifery and other maternity services; a complete infant welfare and school medical service; health visitors; welfare workers; home help to those who need it for medical reasons; and provision for obtaining surgical appliances, dentures, spectacles, etc.
- Open to All, irrespective of means or social position. The Service must, as the Beveridge Report says, be available “for every citizen … without an economic barrier at any point to delay recourse to it.” Poverty must be no bar to health, no bar to a man’s right to life. There should be no lower limit of income, nor any upper income limit, for access to the benefits of the entire services.
- Efficient and up to date. The service must be amply equipped and endowed for research. Medical research workers should be enabled to keep in closest touch with fellow-workers at home and abroad, and all the doctors should have every encouragement and facility for sharing in research. In particular, provision should be made for “team-work” by the doctors, and for bringing together the resources of modern medicine in conveniently distributed Centres.
- Accessible to the public. It should be possible for a general practitioner to direct the public to a centre not too far from home where anyone could be examined by specialists and receive special treatment; and, if necessary, the doctor should be able to call in a specialist to the patient’s home.
- Preserve confidence between doctor and patient. Good doctoring is a very individual business. Patients should be able to change their doctors if dissatisfied, and have a choice of an alternative.
- Equitable for the Medical Profession. The Service must be so organised and paid as to afford a fair deal for the Medical Profession. The nation must tolerate no sweating or overwork of doctors, nurses, or other health workers. That involves having adequate specialist services, sufficient doctors, provision for the free time of health workers, and, amongst other things, a system of pensions for doctors and nurses who are past work. Whilst insisting that the Medical Service shall be available for “every citizen,” irrespective of capacity to pay, we must be sure that the burden of achieving this standard of equality does not fall on the shoulders of the most self-sacrificing members of a generous profession.
Lastly, the Medical Service should be so organised as to enable the medical profession to pull its weight effectively in all those tasks of democratic government which affect the nation’s health. More and more, in planning policy about food, housing, education, industry, etc., the nation will need the guidance of medical science.
Do you agree that this represents, broadly, the kind of Medical Service that the nation needs, as part of a comprehensive Health Service?
Chapter II OUR EXISTING MEDICAL SERVICE
Now, let us briefly review the nation’s existing Medical Service, and see whether it meets the needs outlined in the previous, chapter. We will preface this review by summarising Britain’s health record up to date.
Britain’s Health Record
Since the beginning of this century the health of Britain as a whole has substantially improved. The improvement has been partly due to the general advance of medical science, including the newer knowledge of nutrition; partly to Britain’s Medical Service; partly to the Social Services in general, including such recent developments as the issue of free or cheap milk, cod liver oil, and meals for school-children; and partly to other services, such as housing, which affect health indirectly.
When this century began, the health of a great part of the nation was very bad. For instance, as Sir John Orr has written, “At the beginning of the present century, in some industrial towns, more than half of the children in the poorer districts suffered from rickets to such an extent that those who recovered were left with permanent deformities of the skeleton.”
By the time the present war began, the chances of a child surviving to the age of 60 had greatly increased. There was a large reduction in deaths from tuberculosis. In particular, the infant mortality rate, which was due largely to faulty diet, had been halved. The death-rate in maternity cases has declined in recent years, and in 1938 the death-rate for children less than one year old was only a third of what it had been in 1901, though the death-rate for children under one month old showed little improvement. “The children of to-day,” Sit John Orr writes, “are taller and of better physique than their parents were at the same age.” In a number of infectious diseases, such as diphtheria, the death-rate has been reduced in recent years to a remarkable extent.
We cannot assume, however, that reductions in the rate of mortality always correspond with an increase in positive health. We must recognise that the physical standard of a great part of the nation remains deplorably low. The annual loss of work, energy, and happiness through avoidable ill-health mounts up to a stupendous sum in comparison with what we spend on preventive medicine and medical research. The mass evacuation of children from our crowded cities to the smaller towns and the countryside during the present war has forced the people of Britain to realise, as never before, how shameful and wasteful are the conditions under which a great number of their countrymen and women are still condemned to live. When this war began the nation’s food policy was not based on the food requirements of the people as a whole, but reflected rather the interests of trade. Nor is the nation’s health policy nationally designed or nationally controlled to meet the health requirements of the whole nation.
The lower the family income falls, the lower, generally speaking, is the standard of health. The infant mortality rate has been reduced to some extent in all classes of society, but the richest class has benefited nearly twice as much as the great bulk of the nation from the new knowledge that has made this reduction possible. (R.M Titmuss, Birth, Poverty and Wealth). The infant mortality-rate among the working class is double what it is in the richest section of the population. In 1936 the infant mortality rate per 1000 live births in Glasgow was 109 (which exceeds the rate in Tokyo or Buenos Aires) In Gateshead it was 92, London, 66; Surrey, 42! Tuberculosis is twice as prevalent amongst the poor as amongst the well- to-do, and the average stature of the well-to-do is three or four inches greater than among the poor.
The lower standard of health amongst the poor is due mainly to surroundings, rather than heredity. Statistics show that, as might be expected, the industrial areas are much less healthy than the countryside, and that in the counties of Durham and Northumberland the death-rate of children between one and two years is double the rate in the South-Eastern Counties outside the London area. We cannot do much to control heredity, but we can control our environment; and, if we will, we can have a health policy, as well as a food policy, based on the requirements of all the people.
The war has forced us to move in this direction. The food-rationing policy, for example, whatever its defects, has been such a move. We are now assured by the Minister of Food that the nation in general is better nourished on its war-time diet than it was before the war. What an indictment of pre-war policy this is. It means that the good resulting from improved distribution has out-weighed the injury resulting from the enforced reduction of the national food supply. Will the nation be content to ignore that lesson after the war? Or shall we insist, as to some extent we do insist in war-time, upon there being “bread for all before there is cake for any”?
So much for Britain’s health record. Now look at Britain’s health organisation.
The Control of the Health Services
Who plans and controls the nation’s Health Services? The answer is that a great many authorities are concerned, each controlling a bit, and that no one is in a position to make or direct a coherent plan of health services for the nation as a whole. One might expect that the Ministry of Health would be in a position to do this; but an outline of the powers now possessed by this Ministry will show that this is not the case.
Since 1929, the Ministry of Health has been charged with widely-increased responsibilities in England and Wales; but many important health services remain under other Government Departments, and great unofficial services such as the voluntary hospitals, the insurance companies, and all the doctors in private practice remain outside its control.
The Ministry has some measure of jurisdiction over some of the hospitals, but not all. This jurisdiction includes the special hospitals for infectious diseases, and the Poor Law infirmaries. The jurisdiction does not extend to the “voluntary” hospitals, which number about a third of the total. (For the development of special control over hospital accommodation during the war, see below)
The Ministry controls maternity and child-welfare, supervision of midwives, welfare of the blind. The School Medical Service is under the Board of Education, but with a Medical Officer common to both.
The Ministry of Health deals with housing, sanitation, water supply, river pollution, atmospheric pollution, and the regulation of food and drugs; but poisons are dealt with by the Home Office. The Medical Service in Factories is now the business of the Ministry of Labour, but Factory Inspectors are under the Home Office. Health in Mines comes under the Mines Department, Health in Shops under the Board of Trade, and Health in Prisons under the Home Office. The mental health services and the care of mental defectives are under the Board of Control.
Evidently, then, the direction of the nation’s Health Services is very divided. It is the result of a succession of legislative patches and does not make up a Comprehensive plan. It would be a mistake to assume that a system so evolved must work badly, or that it would necessarily work better if tidied up by a logically-minded theorist. But, in fact, the system does work very imperfectly, even without the added difficulties which war-time imposes. It often works very inconveniently for the patient. It does not allow the Ministry of Health to exercise a control wide enough to ensure an energetic, ccomprehensive, National Service for Health. The Ministry cannot make a rational plan for the economical use of the nation’s hospital service; it cannot adequately provide for a service of specialists to poor patients; it cannot ensure that the doctor’s service is expended where the need is greatest, since the Ministry’s control does not cover the doctor in private practice, and the doctors are largely dependent for their income upon paying patients. Above all, the Ministry, with so patchy a control, cannot do nearly enough to build up preventive medical services and to carry through a positive health policy based on a scientific assessment of the health requirements of the nation as a whole.
The Family Doctor
Turn now from the centre of our health defences, the Ministry of Health, to the front line of those defences—the family doctor, who receives fees from his patients. The system has rendered great service to the nation’s health, and the family doctor often serves as friend and adviser as well as general physician. Undoubtedly we shall continue to need a system of doctoring which preserves this relationship of confidence between the individual doctor and the patient.
The system as at present organised, however, is becoming increasingly unsatisfactory from the standpoint of the nation, of the patient, and of the doctor himself.
The Patient’s Standpoint
Consider the position first from the standpoint of the nation and of the individual patient:
(а) What is needed (as we have seen) is a service of preventive as well as curative medicine. But the family doctor, under present conditions, is not in a position to render such service; he is bound to be a sickness-man rather than a health-man. Called in only when there is recognised ill-health, he has little chance of helping the fit to keep fit, or the near-to-fit to become quite fit.
Moreover, it is difficult for the family doctor, under present conditions, to keep in sufficiently close touch with others who are in a better position than he is to prevent ill-health. During the past 60 years the nation has developed a wide range of public health services, which are manned by a new class of public health officer; but the family doctor has little opportunity of keeping in contact with these officers who work alongside of him. The curative and the preventive health services are not closely associated as they should be.
(b) As we have already said, the nation needs a medical service which is comprehensive, covering all kinds of treatment that may be needed, and open to all, irrespective of capacity to pay. Here, again, we find that the system under which the family doctor now has to work cannot produce such a service.
The family doctor, by himself, cannot provide a comprehensive service. Medical science is becoming so vast a field that specialisation becomes increasingly necessary; the family doctor cannot be a specialist in everything. Medical diagnosis is becoming much more exact, but may often need the service of a specialist. Medical treatment is becoming much more efficient, with new apparatus at its command; but in doing so it becomes more expensive. The general practitioner, who probably has only a small surgery to work in cannot possibly bring together all these new resources of knowledge, skill, and apparatus for the service of the patient; only some kind of Health Centre, supported by the community, can do that.
(c) Nor can the family doctor, by himself, supply a service that is truly open to all, for very many of the people who need a doctor’s attention, especially housewives and young people; are still debarred by poverty from going to him. Poverty makes a huge gap in the nation’s health defences—a gap which not even the most devoted and self- sacrificing of doctor can fill by himself. To some extent this gap has been, narrowed by the generosity of doctors, who often waive or reduce their fees for their poorer patients. It is obviously undesirable that a burden which should be the nation’s should be borne in this way. To some extent, the gap is narrowed by the public provision of free medical services, such as treatment-for tuberculosis and for venereal disease, free of charge where necessary; it is narrowed also by the Poor Law medical service, which makes some provision for the treatment of patients who are technically paupers. To a substantial extent also the gap is narrowed by the National Health Insurance Scheme, by which insured persons can secure certain medical attention and treatment from their panel doctor. But still the gap between medical needs and medical service remains a wide one. It is particularly injurious in the case of children, who. are not covered by the Insurance Scheme, and for whom the School Medical Service does not yet provide an adequate service. No mere tinkering with the system will close this gap. If we want a Medical Service which is open to all, comprehensive, preventive as well as curative, and based on relations of confidence between doctor and patient, we shall have to make some radical change in the present system of organising and paying for the service of home doctors.
(d) These are not the only weaknesses of the existing system of family doctoring, from the standpoint of the nation and the individual patient. The service is not nearly as efficient as it should be, within its present limits.
For one thing, the training of a medical student is so long and costly that doctors are recruited from too narrow a section of the population. A full medical education lasts at least five years and costs about £1,500. Scholarships and prizes, and in Scotland the Carnegie Trust, afford some relief, but in effect there is a very stiff entrance fee for this profession, which restricts recruitment to about one-sixth of the population. Here, surely, is a waste of ability which the nation cannot well afford. The accident of wealth should not be allowed to play this decisive part in the selection of doctors. Ability should be the only test.
A still more serious weakness is that doctoring is not, and cannot be, allocated in accordance with the real need of the population. Having no fixed salary or pension, doctors naturally tend to congregate where they are likely to make a good income, rather than in those fields where the need for doctoring is greatest. No public authority can now say to the doctor: “You are wanted in Durham or in the Rhondda Valley, rather than in Harley Street.” Wealthy private patients can pay the piper; and so to a great extent they can call the tune, even though this results in wasteful distribution of medical services which the whole nation needs to share.
The Doctor’s Standpoint
We have considered the present system of private doctoring from the standpoint of the nation and of the patient. There remains the question:. Is the system satisfactory from the doctor’s standpoint?
There is an increasing recognition in the. medical profession that it is very unsatisfactory. The conscientious doctor wants to be able to serve effectively in preventing ill-health; but he knows, better than, any layman, that at present, he cannot do this. He cannot even keep in touch adequately with the preventive work of the public health services. The doctor wants to see his patients supplied with whatever kind of treatment they need: but he cannot himself supply that treatment. He wants to spend his skill as a healer on those who most need it, regardless of their capacity to pay; but,: however generous his intention, having no assured income or pension, he is hampered in giving such service. The existing system.is not producing nearly enough doctors for the nation’s needs, and it makes no provision for the doctor to be “off duty; so the general practitioner is apt to be perpetually overworked. That is very bad for him, and also for his patients.
There is only one way in which these difficulties can be removed and that is by providing for “teamwork” between doctors, better contact between general practitioners and specialists, and fuller access to all the resources of modern medicine. That leads to the conclusion that, in the doctor’s interest as well as that of the patient, there must be well-equipped Health Centres throughout the country as part of a National Service for Health, and that the doctors should be whole-time, salaried officers of that Service.
National Health Insurance
We come now to the National Health Insurance Scheme, which was provided as u means of mitigating some of the defects of our private medical service which have just been noted.
The Scheme applies, broadly speaking, to all persons who work under an employer’s direction and whose salary is less than £420 a year (formerly £250). The insured persons are entitled to a certain amount of free doctoring by a specified doctor “on the panel ” and to a certain amount of drugs and medical, necessities. In addition, insured persons
can qualify for receipt of financial assistance during a period of incapacity. The Scheme entitles the doctor to a capitation fee for each person registered as being on his panel.
The Scheme has done a good deal to mitigate the defects of the old, wholly unorganised, medical system.
(а) It is not designed, however, for the prevention of ill-health but only for its cure. A doctor, when in panel practice, is in no better position for preventing ill-health than he is when acting as a private family doctor.
(b) The Scheme does not provide a comprehensive service, covering all kinds of treatment that may be needed. What is demanded of the panel doctor himself is no more than the elementary standard of doctoring which any and every general practitioner can provide.
Patients often complain that the panel doctor’s attention is perfunctory. This would not be surprising, for the panel doctor is not employed full time on this part of his practice, and he can hardly help feeling the pull of other, more lucrative, employment.
A very important deficiency in the service is that it does not entitle the insured person to hospital treatment, or to the service of specialists.
(c) The Panel Service, by its nature, is not open to all. It does not include the higher- paid, salaried worker, nor those who work on their own account, nor the dependents of those insured. More than half of the population is not covered by the Scheme; and, as we have indicated, even those who are included are not fully provided for.
(d) A further defect of the Panel System is that it does not provide sufficient guarantee for the efficiency of the doctors employed. A fact too little realised is that practices are bought and sold by doctors, and that anyone can buy a practice if he has a minimum qualification, and if he possesses, or can borrow, the requisite capital. The general public lacks the knowledge for appraising the quality of his service and his efficiency is not in fact subject to any adequate public control. If he has a manner which ingratiates him with his clients; he can retain and even increase his practice, even though his technical competence may be very low.
(e) Lastly, the scheme bears hardly on the doctor who desires freedom from financial anxiety coupled with freedom to do the best work of which he is capable. He cannot speak freely, bluntly, as a healer, or as a guardian of good health, if he has always to be thinking of pleasing enough patients to swell the list on his panel.
In short, the National Insurance System, for all its merits, does not meet more than a section of the nation’s need.
Hospitals
The nation’s hospital system is a curious medley. It includes some 2,000 public hospitals and some 1,000 so-called “voluntary” hospitals of various types. The public institutions are under the control of Local Authorities, democratically elected; the voluntary hospitals are responsible only to their own individual governing bodies. The public hospitals are paid for almost entirely out of rates and taxes, whereas the voluntary hospitals finance themselves as best they can by private endowment, by appeals to private charity, and by payments for services rendered.
All the medical schools in the country (except one) have grown up in association with some large voluntary hospital. It is in these hospitals that a large part of the nation’s medical research work is done:
(1) The Voluntary Hospitals have rendered great service, and have been maintained by devoted effort, much of it unpaid. Much of the medical work in these hospitals is done by “honorary staff,” who receive no monetary payment, but who may thus gain prestige and reputation; generally it is those who can afford to take this road who find their way to Harley Street and to highly-paid consultant practices.
The voluntary hospitals have to wage a perpetual fight for funds. Their income from charitable sources had increased before the present war, but not fast enough to meet their needs; and nearly a third of them were in debt. During the war, their financial position has been temporarily eased as a result of the State’s Emergency Medical Service, which is referred to below.
(2) The Public Hospitals were mainly built in the 19th century as Poor Law Hospitals or Institutions, or for infectious diseases. Many are still Poor Law Hospitals, controlled by Public Assistance Authorities. Others have been taken over by the Public Health Committees of County and County Borough Authorities, as Municipal Hospitals. Some of the public hospitals have been developed in recent years to a high, standard of efficiency by Municipal Authorities.
The public hospitals provide nearly three-quarters of all the available beds in the country, including nearly all the beds for infectious diseases, most of those for tuberculosis, and many for maternity cases.
The Ministry of Health exercises only partial control over the policy of these hospitals.
(3) During the war the Government has exercised partial control over all hospitals of any size, so as to operate the Emergency Medical Service Scheme which had been roughly planned before the war. Under this Scheme, beds were reserved in each hospital for “E.M.S.” cases, such as civilian war casualties and patients from the Forces. The Government has paid for the beds thus reserved. The Scheme has resulted in some grouping of hospitals and in the division of the country into a dozen large areas for administrative purposes. Some such Scheme has been indispensable for war purposes, but the existing Scheme could not meet post-war needs. It is without any adequate democratic control and without plan; it is largely controlled by representatives of the voluntary hospitals; and any attempt to make permanent the arrangements which were imposed for war-time purposes would be resented by the authorities in charge of public hospitals.
One of the defects of the hospital system as now organised is that the Voluntary Hospitals do not, generally speaking, provide beds for chronic cases, among which the majority are old people; so that the Local Authorities have to find accommodation for almost all such cases.
Reviewing the Hospital Service as a whole, it must be said that it lacks coordination; it lacks such provision for comprehensive planning as would ensure the location of hospitals where they are most needed and their use for the purposes most required in the national interest; it often lacks adequate provision for prompt and efficient treatment (There is, for instance, a great shortage of beds for the treatment of rheumatic diseases); and it also lacks a comprehensive system of financing which would eliminate the present scramble for charity, and would make possible a long-term programme of development.
Maternity and Infant Welfare
An efficient, co-ordinated service for mothers and for infant welfare is a national necessity, as was shown by the terribly high death-rate of mothers and infants before 1918. The Public Health Act, 1936 (which incorporates the Maternity and Child Welfare Act of 1918), permits Local Authorities to provide Ante-natal Centres for looking after expectant mothers, and Centres for infant welfare. The Midwives Act, 1936, requires Local Authorities to secure the provision of an efficient service of midwives. In practice, some Local Authorities do a lot, others very little. The agencies dealing with maternity in London, for example, are numerous and uncoordinated. A uniform maternity service, nationally planned and locally administered, is urgently needed.
School Medical Service
A School Medical Service is a logical corollary of making school attendance compulsory, if only because a child in poor health cannot get full benefit from education. It was not until 1907, however, that this fact was recognised by the beginning of a School Medical Service.
At present, this Service provides for free medical inspection of every elementary school child at least three times between the age of entering and leaving school; but sufficient time for a thorough and complete examination is rarely available. Local Authorities provide treatment for school-children’s minor ailments, practically free of charge. There is also some provision for treatment of teeth, eyes, nose, and throat, etc., but this is still very inadequate in some localities, especially as regards dental treatment, and some payment has to be made by the parents, save in special cases. Increasing provision has been made for supply of milk, cod liver oil, etc., and this has had a valuable effect on the children’s general health. Before the war there was provision on a small scale of cheap meals for children at school, and this has been extended during the war, where school equipment permits; but even now the scheme provides for only one-fifth of the children. Finally, the benefits of the National Health Insurance Scheme have lately been extended to cover employed children who have left school but are not yet 16.
Thus, we can say that the foundations of a School Medical Service have been laid. But evidently the service greatly needs expansion. All too often in the past, this expansion has been cramped by the demand for economy by Local Authority Committees; so that poverty has remained a bar to health just at the time of life when the foundations of health are being laid. (The old are voters, the young are not!) Let us remember, for the future, when dealing with Health Services for the young, that in no field of medicine is “economy” more likely to prove “false economy.”
Permissive Health Legislation
Much of Britain’s existing health legislation is “permissive.” Local Authorities are allowed to provide certain services, but may fail to do so. This applies, for instance, to the maternity service: much would be gained if the more backward Local Authorities would exercise the powers permitted so as to bring up their service for maternity to a standard comparable with that achieved by the more progressive authorities. The “permissive” laws ought in such cases to be changed into obligations.
Moreover, in some cases the powers of Local Authorities are limited in such a way as to make an efficient, comprehensive service impossible. Thus, Local Authorities can provide domiciliary treatment in the case of paupers but not for others. In the well- equipped cities children who are well enough to attend clinics can get first-class treatment for dental, eye, rheumatic, throat, and-ear troubles, etc., but if the child happens to be too ill to attend the clinic, the school medical service can do no more, and the parent can only call in and pay for a private doctor. Such anomalies ought to be cleared away by an “all-in” service.
Summary of Conclusions
The foregoing chapter has sought to show that the nation’s existing medical service, good though it is in many respects, is ill-planned and far from adequate for the needs of the nation as a whole. Further it is contended that there is need for more control at the centre; the Ministry of Health should be in a position to plan the lay-out of the nation’s hospitals, doctoring, etc, according to the nation’s need. The family doctor’s position is unsatisfactory; in particular, more “team-work” is needed, and the efficient doctor should have an economic security which the present system cannot give. Whilst the defects of the old system of private doctoring have been mitigated by the National Health Insurance Scheme, they have not been removed; and the Scheme does not provide a medical service which is comprehensive or open to all, or well-equipped for the prevention of ill-health. Moreover, the hospital system is an unplanned medley of public and voluntary institutions, without any unified control, and with many financial embarrassments. Certain services in particular, such as the provision for care of mothers before, during, and after child-birth, and the School Medical Service, are in special need of expansion.
How are these needs to be supplied? How are these defects to be remedied?
Chapter III WHY A STATE MEDICAL SERVICE IS NECESSARY
Having considered what kind of medical service is required and what the existing service is like, we can now answer the first of our two questions: “Is a State Medical Service Necessary?”
A Central Health Authority
We have seen that there is need for a Central Authority, empowered to plan the lay-out of the National Health Services, including the medical service, on the basis of a scientific assessment of the needs of the whole nation, and to see that the plan is carried into effect. We have seen, too, that this need is not now being met; the Ministry of Health lacks the power to pull the medical service into shape as a coherent whole.
The conclusion surely is that a Central Authority responsible to Parliament, must be given the powers appropriate to the central organ of a comprehensive National Service for Health. That Authority must be in a position, for instance, to weld together the separate sections of our hospital system into in economically-planned service. Just as the Ministry of War directs the strategic placing of the Home Forces for defence against invasion, so this Central Authority should be able to plan the strategic disposition of the nation’s defences against ill-health.
Local Health Authorities
The Central Authority, however, should not attempt to run the whole machinery. That would mean certain breakdown. Wide powers must be left to Local Authorities; it is they who must be responsible for the detailed administration of the service. That administration must be organised in units of convenient size; it must bring together all the necessary services at convenient Health Centres; and it must be elastic, allowing for considerable diversity of treatment. At present Local Authorities are not in a position to do all this; they cannot construct a comprehensive scheme which will govern the policy of voluntary as well as public hospitals; they cannot bring together a team of general practitioners at a series of Health Centres, or provide a full service of specialists to patients who need them. Nor can the necessary powers, with the necessary democratic control, be obtained except as part of a comprehensive National Health Service.
Doctors
The same conclusion emerges when we consider how the nation can obtain the services it most needs from the doctors, whilst affording to the doctors all the consideration that it owes to them? Unless the doctor has a salary, and a prospect of pension, which frees him from economic dependence upon paying patients, he cannot devote his full energy to the prevention as well as to the cure of ill-health. Unless the community provides that economic security, it cannot direct where the doctor’s work would best be used in the national interest. Only a salaried medical Staff, as part of a National Health Service, can meet the need.
National Health Insurance
It is sometimes suggested that the nation’s need can be simply met by extending the National Health Insurance Scheme. That is a mistake, as will be seen if the principles of Health Insurance are compared with the principles of a nation-wide Health Service such as is here proposed. The essence of any commercial insurance scheme, properly so-called, is that the insurer has to cover risks which he can calculate within a narrow margin of error; the premiums payable by the insured must be determined in advance and must be paid regularly; the insurance payments offered must be limited in amount and the treatment must be limited in character, and these benefits must be confined strictly to those who have paid the premium or are covered by it.
On the other hand, the essence of a nation-wide Health Service is that it covers risks to health which cannot be exactly computed; that the benefits it offers must include every kind of treatment needed by the patient, and must provide that treatment for as long as the doctor thinks necessary in the patient’s interest; and that no one should be debarred from these vital services by poverty or any other cause. It was agreed at the outset that the Health Service which the nation needs must be preventive as well as curative, comprehensive, and open to all. That means that we are calling for something different in kind from an Insurance Scheme. We want the whole nation to be the insurer, and the. whole nation to be the insured. What we want does not involve a mass of paper work, or filling-in of forms, or competitive offers of this and that special benefit as the reward for an increased premium. What we want, in short, is a comprehensive service for the health of the whole nation, provided by the nation, for the nation.
Hospitals
One more example must suffice.
We have seen that the hospital system has grown up haphazard and without adequate co-ordination. We have estimated that in some respects the hospitals are much below the standard of efficiency and equipment that should now be required. It is clear that the voluntary hospitals have to base their policy upon the uncertain outcome of a competition for charity, and are subject to no public control. How is it possible, without some unified planning and control, to build up a hospital service that is well adjusted to the need of the nation as a whole? Surely the conclusion must be that public and voluntary hospitals alike must be brought within a National Health Service on equitable terms.
SUMMARY OF CONCLUSIONS
We said in the first chapter that the nation needs a Medical Service which is planned as a whole; we have seen that no authority is now in a position to make such a plan or to see that it is carried out;
We said that the Service should be preventive as well as curative; but we have seen that neither the system of paid private doctoring nor the National Health Insurance Scheme is in a position to deal adequately with the problems of prevention of ill-health. Only a salaried State Medical Service can do so.
We said that the Service should be complete, covering all kinds of treatment required; we have seen that it is far from complete and can only be made complete by State action.
We said that the Service must be open to all, so that poverty shall be no bar to health; and we have seen that this provision for the nation as a whole can only be made by the nation as a whole.
We said that the Service must be efficient and up to date, providing for “team-work” and for convenient concentration of medical resources; but we have found that only the community can achieve this, by means of a health system which allows for a planned disposition of hospitals, doctors, etc.
We said that the system must offer a fair deal to doctor and patient alike; but we found that only a system of whole-time, salaried, and pensionable doctoring would meet these requirements.
We said that in the interests of true economy certain Services, such as the School Medical Service and the various Services connected with maternity and infancy, need expansion; only the community can provide for this expansion.
So it comes to this:
Do you, as a citizen, want a Medical Service that is planned and directed in accordance with the needs of the nation as a whole; or do you think that we had better muddle along with the present system, distorted as it is by the influence of private profit?
Do you not agree with the Labour Party that the Medical Service should be developed, as rapidly as conditions permit, into a State Medical Service, as part of a comprehensive National Service for Health?
PART II A STATE MEDICAL SERVICE
Assuming that a State Medical Service is needed, how should it be organised? What services should at render? Could the nation afford it?
Here, in brief, is the Labour Party’s answer.
Chapter IV LABOUR’S PLAN FOR A STATE MEDICAL SERVICE
The nation’s most precious asset—its health—is to be insured by the entire nation. So the nation must have, amongst other services, a State Medical Service which is sensibly planned so as to make the very best use of all the nation’s medical resources for the benefit of all.
Organisation
There must, therefore, be some Central Health Authority, competent to plan the Health Services as a whole, including the Medical Service, subject to the general control of Parliament, and competent to see that the plan is carried out, with due allowance for the diversity of local conditions.
There must also be some kind of Regional Authority, for the more detailed planning of the medical service and for its administration.
Besides this, there must be local units, under the general administration of the Regional Authority. Some of these operational units should be large enough to allow for the concentration of medical equipment and specialists at convenient centres, others should be small enough to make the service easily accessible to everyone who needs it.
The Ministry of Health
The Central Authority can only be the Ministry of Health. No other Authority has the Ministry’s accumulated knowledge of national health conditions; nor could any organisation less nation-wide in scope be held responsible to Parliament. In a matter which so vitally concerns the whole nation, it is Parliament, representing the whole nation, which must have ultimate control.
What has been said of the Ministry of Health applies, in the case of Scotland, to the Scottish Department of Health.
The powers of the Ministry will need revision, however. On the one hand, its powers should be extended to cover all the Health Services, including those now controlled by other Departments, such as the School Medical Service and the health service in factories; for technical reasons the medical services of the Armed Forces should be excepted. On the other hand, the Ministry of Health should be relieved of responsibility for services which affect health only indirectly, and which involve large-scale organisation. (This principle is being adopted in the case of housing.).
The Minister, of Health should continue to be responsible to Parliament.
Regional Health Authorities
Labour’s Plan for the reform of Local Government (see the Labour Party’s pamphlet, “The Future of Local Government”) recommends that the country should be divided into Regions, each having a Regional Authority for certain purposes of Local Government; and that these Authorities (unlike the regional organisation during the war) should be democratically elected. The Party also proposes that, for health purposes, each of these elected Regional Authorities should appoint a Health Committee for its Region. Under these Regional Health Committees there should be appropriate subcommittees.
Divisional Hospitals
(1) Within each Region there should be a series of Divisional Hospitals, associated with Divisional Health Centres.
The divisional unit must be large enough to justify a big, fully-equipped hospital, and the concentration of specialists of every type. It has been found by experience that an economic size for such units is one which includes a population of about 100,000 persons and requires a hospital of about 1,000 beds. In some cases it may be convenient to have larger “operational units,” with, say, 250,000 population and several Divisional Hospitals.
The Divisional Hospitals should be large and fully equipped, with from 600 to 1,200 beds; they should include departments for X-rays, for rehabilitation of patients whose powers have been temporarily damaged by ill-health or accident, and for other kinds of special treatment.
These should be General Hospitals, treating all kinds of cases except infectious cases or mental disease of certain kinds, apart from these exceptions, “special” hospitals should be eliminated. The system should provide for a certain amount of specialisation in the following way: The General Hospitals should be associated in groups, so that only one hospital out of a group of three or four would admit, say, skin cases, or eye cases; perhaps only one hospital in each Region would undertake rare specialised treatment such as plastic surgery or brain surgery. Thus, whilst in the main the Divisional Hospitals would be General Hospitals, specialised units would be included in them.
(2) For this reorganisation, the nation will need all, and more than all, the efficient hospitals that there are at present—both public and “voluntary.” All those that come up to standard and can be fitted into the scheme should be brought within a coherent plan—a plan that is reasonably elastic and constantly brought up to date. This means that voluntary, as well as public hospitals, must be brought into the National Scheme, on terms which will satisfy the nation’s sense of equity.
The Labour Party therefore proposes that the Government should lay upon Local Authorities the duty of securing a comprehensive hospital service, based on a coherent but adaptable plan, each plan covering a large area—a “Region.” All hospitals within the area, whether public or voluntary, general or special, should be required to come into and conform to this plan, undertaking only the type of work which is allotted to them in the plan. The standard of efficiency, and the conditions of service and staff should become the same for all, and all should be subject to inspection by inspectors responsible to the Ministry of Health. The voluntary hospitals should be required to admit all patients in accordance with a unified system of admission covering the whole hospital service.
A simple method of achieving the goal of a unified hospital system would be as follows. The voluntary hospitals might receive financial assistance in respect of the cases referred to them by Local Authorities, and the Local Authorities would become entitled to a share of representation and control on the Governing Board of the hospital which is proportionate to the services rendered to the patients thus referred. The effect of this scheme would be to ensure that before long the voluntary hospitals will come under the control of the Local Authorities, and that the conditions of service and staff in all the hospitals will become standardised. Thus we should have at last a unified hospital system, laid out on a rational plan, each section of the plan covering a sufficiently large area for efficient working.
(3) The staffing of Divisional Hospitals should be of the highest possible standard. A hospital of the size indicated would need a staff of about 50 doctors of various types. Specialists would see cases referred to them at the hospital, and should also be available for consultations at the Health Centres or in the patients’ homes. The specialists’ service should be so organised by the Divisional Hospital and the Divisional Health Centre in co-operation as to be available at short notice at all times.
It is important that the doctors working in the Home Doctor Service should be able to keep in close touch not only with the cases which they have themselves sent to the hospital, but also with the hospital’s general work.
Divisional Health Centres
The Government should require Local Authorities to establish Divisional and Local Health Centres as soon as conditions permit, and should offer grants for this purpose, sufficient to cover a large, proportion of the cost. Each Divisional Centre should, where practicable, be close to a Divisional. Hospital. Its equipment should provide for the widest possible range of services, including those that cannot always be provided at Local Centres.
There should be a laboratory adequate for the service of the Divisional Hospital and Health Centre, and it should be staffed and equipped on a scale sufficient to allow for research. The clinical pathologist in charge of a laboratory should co-operate with the whole staff of the division, including the doctors in general practice, so as to facilitate research work throughout the area.
Local Health Centres
In each divisional area there should be four or more Local Health Centres, each linked with the Divisional Health Centre, and each served by from eight to twelve general practitioners. In rural areas, these Local Health Centres may have to be much more numerous in proportion to the population, and may have a much smaller number of doctors—perhaps only one or two.
At these Centres patients would obtain the service of their home doctor; and through him they could draw upon a complete service of specialists at, or from, the Divisional Centre or Hospital. The Local Health Centres would also organise the services of midwives, home nurses, home helps, health visitors, and social welfare workers.
Health Records
One of the great advantages of a unified medical service, with Health Centres as proposed, would be that complete records of the health of all the people could be kept. The Health Centres, Local and Divisional, should have an appropriate clerical staff; and the clerical work should include the keeping of health records. The records would be available, in strict confidence, to all doctors in the unit who may require them, and would be sent to the Health Centre of any other area to which the individual may move.
The value of such continuous recording of the medical history of each individual, in health and in sickness, need hardly be emphasised. Suppose, for instance, that a boy is examined in the school medical inspection. Is it not obvious that the record of that inspection should be available in confidence to the doctor who may afterwards see the boy at the Health Centre, or at home? Presently, the boy may go away to some other part of the country, and may there need a doctor’s attention. Would it not be sensible that that doctor should have access, without difficulty, to the boy’s medical history? If the boy had to go into hospital, would it not be useful that the doctor in charge, during convalescence should have knowledge of the record of his case whilst in hospital and before he went there?
Only an organised, unified Medical Service, with an adequate clerical staff, can provide such a system of records.
Specialist Services
One of the developments most needed to make the nation’s Medical Service comprehensive is the provision of a service of specialists, available to all who need it. The plan outlined above will afford by far the best means of organising such a Service. (Some Local Authorities now find it convenient and economical to employ full-time specialists who divide their time between the clinics and the municipal hospitals. The existing law allows a local doctor to call in a specialist to a patient’s home, charging the cost to the Local Authority; but this applies only to maternity cases.)
Home Doctors
The general practitioner, or “home doctor,” is the first line of the nation’s health defences; and he must always retain that position. The confidential relation between doctor and patient is an indispensable part of a satisfactory health service. It is becoming apparent, however, that the present system of organising and paying for the doctors’ services has become increasingly unsatisfactory from the standpoint of the nation, of the patient, and of the doctor himself. The patient is not getting a service that is preventive, comprehensive, open to all, and fully efficient. In particular, the nation’s resources of doctoring are ill distributed, and the doctor’s conditions of employment do not adequately protect his own health, or his freedom as a guardian of health.
In the Labour Party’s opinion, therefore, it is necessary that the medical profession should be organised as a national, full-time, salaried, pensionable service.
Doctors and nurses, as well as the rest of the medical profession, should have fixed hours of service; though in the doctor’s case an emergency may of course arise which will upset his normal time-table.
The service must be national, i.e., supplied and paid for out of taxes and rates. We cannot have a Medical Service which covers all the medical needs of all the people unless all the people contribute to the cost, and unless the doctoring can be distributed in accordance with the needs of all the people.
The service should be full time. Suppose that it were not full time, but that the doctor was partly employed in private practice. Either his service for the State would be just as thorough and conscientious as his service when treating fee-paying patients as a private doctor, or else his standard would differ. If patients could get his full attention, however, without paying a fee during half the day, they would hardly go to him during those hours when a fee would be charged. It would be intolerable that his service as a State doctor should be less adequate than the service rendered for private fees.
National Service for Health is a service honourable enough for any recruit; it should be a service well enough paid and protected to meet the needs of every doctor in a democratic Britain.
The service should be salaried and pensionable. The State should make equitable provision for the security of tenure and superannuation rights of all the members of the State Medical Service; and it will be necessary for reasons of equity to devise a scheme of compensation for the value of doctors’ practices in which doctors have invested capital. Only when the doctor is thus paid will it be possible to set him free to do his best work in the wide field of preventive, as well as curative, medicine. Only so will it be possible to ensure that the service of doctors is distributed in accordance with a disinterested estimate of the nation’s needs. Only so will it be possible to protect the doctor against the overwork which is often the consequence of his own devotion to his great task as a healer.
It may be that for a while some doctors will wish to be left out of the State Scheme, and remain dependent upon private practice. The nation should make the service so efficient and complete that no patient could desire a better and every doctor will wish to serve in it.
Midwives
The service of midwives should be organised through the Local Health Centres, and the midwives should form a team with the obstetrical doctors. Much of their work will be in the homes of mothers, but they must also be in close touch with the Maternity Section of the Divisional Hospital.
Health Visitors
Health visitors should be available at the Health Centre and in the home. They should become a strong link between the family and the medical staff of the Health Centre. In particular, they should be concerned with protecting the health of infants, and with education in the preservation and development of full health for all in the home.
Social Welfare Workers
In any Health Service, trained social workers have an important place, especially so long as surroundings—such as bad housing—contribute so largely as they do in our industrial towns to the production of disease. Such workers should be able to contribute substantially to the improvement of “environmental” conditions affecting health.
Home Helps
Home helps are at present available in some areas to assist mothers with new-born infants. This system should be developed so that home help can be provided in homes where the mothers have been removed to hospital, or are prevented by whatever cause from attending to home and family.
Nurses of the Home Nursing Service
Local Authorities should be required to establish a complete Home Nursing Service in every locality. The nurses should work with the medical staff of the Health Centres, and the admirable personnel now employed in the District Nursing Service should be taken over by the Local Authorities and increased where necessary.
Hospital Nursing Service
Hitherto, the nursing profession has commonly been grossly underpaid and over-worked. It is only recently that a major effort has been made to remedy this by State action. Those who have ever been in hospital know how much their comfort has depended upon the nurses’ unfailing care, no matter how irritable and unhappy the patient may sometimes have felt. It is then that one has realised something of the strain under which the nurses have to live. The community would be blindly ungrateful and very foolish if it did not ensure a fair deal for nurses in regard to working conditions, salaries, pensions, and training.
School Medical Service
At present the School Medical Service is very inadequate, and, as already noted in Chapter II, little medical service is available for school-children without cost to the parents. The Labour Party holds strongly that free treatment in the School Medical Service should be instituted without delay. If a child requires treatment and is not being attended by the family doctor at home, the School Authorities should send the child to the Health Centre or Hospital, for treatment free of charge to the parent.
There should be at least four medical inspections of school-children during school life, instead of the standard of three inspections as at present, (when the school-leaving age is raised the number of inspections should be increased) and these should be thorough, instead of being summary and superficial, as is too commonly the case now.
In addition, there should be annual inspections of teeth, sight, and hearing. Twice a| year all school children should be weighed and measured. A special inspection should be made not only after a child has developed definite symptoms of illness but whenever the child’s physical and mental progress is found to be below normal.
Maternity Service
The care of mothers and infants has long been organised as a separate service. In developing this service, so as to fill its essential place in a State Medical Service, the experience of the existing schemes will of course be a necessary foundation.
Here, in brief, is the Labour Party’s Plan for a complete National Maternity Service. It is assumed that the aim of the service will be the safety and comfort of the mother and baby; that all personnel concerned must be fully capable for their job, and should co-operate closely, before, during, and after the confinement; and that all the services should be co-ordinated under the Regional Health Committee.
(1) Ante-Natal Service
There should be ante-natal supervision of all expectant mothers, and, when necessary, treatment. For this purpose, ante-natal clinics are essential and should become an important part of the work of the Local Health Centres. Patients should (as now) be encouraged to attend the clinic, both for medical examination and for advice and help as to preparations for their confinement (such as the early booking of a midwife or hospital bed). The clinics should be staffed from the Maternity Department of the Divisional Hospital. The Dental Service at the Health Centre should be available for the treatment of expectant mothers.
Health visitors will also be attached to the Centre, and will be in a position, through their normal visits to patients’ homes, to ensure that the advice given to mothers at the clinic is understood and carried out. The health visitor will also be able to advise whether the mother’s home conditions are, or can be made, suitable for her confinement, or whether this should take place in hospital. (In general, all first confinements, and all confinements which are likely to show some departure from the normal, should take place in hospital.) If the staff of health visitors is adequate and competent, and if the other services are manifestly of a high standard, the health visitor should be able to allay unnecessary anxiety and to persuade the mothers to make full use of the services offered.
(2) Confinements
(а) Home Cases
Every effort must be made to ensure the efficient working of the Midwives Act, 1936, with the direct appointment of qualified and competent midwives by the Local Supervising Authority. This service should be organised from the Health Centre.
Sterilised maternity outfits should be available for all mothers. A uniformly good set should be provided and regarded as part of the necessary equipment of the midwife.
Ample provision for domestic assistance must be ensured. The Local Authority should have a service of suitable women for employment as “home helps,” a regular salary being paid for full-time work. Domestic assistance should be available for special cases during pregnancy, and for a longer period than two weeks after the confinement, whenever necessary.
(b) Hospital Cases
The hospital provision for maternity cases must be adequate, and must include beds for emergency cases of all kinds. The patients should remain in hospital for not less than the minimum period of 14 days. It is desirable that there should be small wards of not more than four beds. Proper isolation accommodation must be provided, with all precautions against puerperal infection.
Whether the confinement is in hospital or in the patient’s home, labour should be made as painless as possible; provision must be made for anaesthesia. In hospital this is easy; at home, methods which the midwife can use should be developed and taught.
(3) Post-Natal Services
As far as possible all patients should be seen after childbirth by the same staff as were responsible during the ante-natal care and at the birth. At least one full examination of the patient should be made, and advice should be available at the Health Centre. It is important that further home help should be provided when required, and that there should be convalescent homes to which mothers can be sent after childbirth for periods of rest if necessary.
Tuberculosis
Among the diseases connected with poverty, none is more deadly than tuberculosis. Wherever we find poverty, poor food, over-crowding, over-work, lack of good air, there we find a high tuberculosis rate.
Between the wars, the death-rate from tuberculosis in England and Wales was reduced by more than half, but even so the deaths in 1938 amounted to 26,000. With the outbreak of the present war this improvement was sharply reversed, especially in Scotland. The Government have taken one important step to deal with this, by providing for cheap and rapid X-ray examination, so as to identify the disease while it is still amenable to treatment. But this provision for improved diagnosis will not have its proper effect unless certain other conditions are satisfied. There must be adequate subsistence allowances for a patient’s family during his or her absence; otherwise the patient will be tempted to postpone until too late the opportunity—which is also a social duty—of undergoing the treatment even at a time when he may still be feeling well. The same applies to the provision of home help. There must be adequate staff and accommodation in hospitals and sanatoria, so that patients are not kept waiting. Further, when the patient is convalescent, there should be provision for “rehabilitation,” with suitable work, both for infectious and non-infectious cases. In all these respects, new developments are needed, as part of the State’s comprehensive Medical Service.
Industrial Health Service
A very important part of the National Health Service will be the provision of preventive, as well as curative, health services in industry, especially in factories. At present, factory legislation only prescribes minimum standards as to health, safety and welfare conditions in the factories. There are not nearly enough official Factory Medical Inspectors. Industrial Medical Officers are now employed in large factories; but they are paid by the employer, which unduly weakens their position, and which may give rise to professional difficulties as to the confidential relationship between doctor and patient. A large development of the work of Factory Inspectors and Medical Officers is required, to prevent occupational maladies, to improve factory conditions and amenities, etc. In particular, Medical Officers should be in a position to advise freely on measures needed to prevent ill-health and over-strain, especially in dangerous occupations, and to recommend improvements in the statutory standards for health, safety and welfare.
The industrial health service is of course a specialised service, but needs to be interwoven and co-ordinated with the National Health Service as a whole. The work of industrial Medical Officers should be fitted in with that of the Inspectors, so as to provide a complete service of health, safety and welfare by a team, comprising the Factory Inspector, and the doctor, industrial nurse, welfare workers, and the worker themselves.
Mental Health Services
Much needs to be done about the Mental Health Services, i.e., those concerned with mental illness, neurotic illness, and mental defect.
If the reform of these services is to be carried through with the necessary energy, public opinion must become more awake to the importance of the subject, and more enlightened about mental sickness and suffering. In 1938 the number of persons in England and Wales notified as being under care for mental disorder was 158,723. In addition there were 89,904 mentally defective patients in institutions and under statutory care. The net cost for mental hospitals and certified institutions was £11 ½ million.
Whilst there is now a growing realisation of the influence of mental factors on the health and happiness of every citizen, there is still an unfortunate tendency to regard mental illness as shameful, and as leading inevitably to long residence in a mental hospital. In consequence, patients and their relatives are reluctant to seek advice in the early stages of mental illness, when the prospect for recovery is good provided that modern forms of treatment are applied.
The amount of incapacity and suffering due to neurotic illness (which is often associated with some physical cause) is still much too little realised; very many of the neurotic patients seen by general practitioners could be cured if suitable treatment were available.
As for mental deficiency, permanent retention in an institution is necessary in many cases, at least in the present state of medical knowledge; but a good many of the less backward cases, given suitable training and after-care, are capable of becoming useful members of the community.
The main reform needed is that the Mental Services should be incorporated in the National Health Service. The close connection between mental and physical health is becoming clearer and patients and health workers alike would benefit from more interchange of knowledge and service between the mental and other sections of the Health Service.
One much-needed reform is the reduction of the size of the very large mental hospitals, and especially the reduction of the size of wards. At present, such wards not uncommonly provide for 80 to 100 patients; 25 would be a reasonable maximum. Too many mental hospitals are simply institutions where custodial care is given but where modern treatment and proper classification of patients is not available, owing to shortage and unsuitability of staff, equipment, and funds.
Little provision is made for in-patient treatment of neuroses in civilians; and, whilst most cities now have out-patient clinics for psychological cases and child-guidance clinics, these are totally insufficient for present needs.
It is important that there should be wards in large general hospitals, staffed by suitably trained doctors and nurses, for treatment of neurotic cases and the early stages of mental illness. This will help to ensure that those needing in-patient treatment will seek it early, undeterred by the stigma attaching to the word “mental”; it will help also to ensure fullest co-operation between workers in the physical and psychological fields.
In industrial health, specialists in psychology can help in many ways, e.g., by suggesting suitable work for children leaving school, by correcting conditions of work liable to cause nervous strain, and by ensuring, with the help; of social Workers; that people who have recovered from some mental trouble, do not, on returning to work, go into jobs of a kind likely to make the trouble recur.
Treatment in an institution is often necessary for mental cases. But segregation of such patients has its dangers, as the law recognises; and the statutory provision for the visiting of such patients by competent laymen is a humane safeguard which should be maintained and developed.
It must be recognised that such reforms, involving reorganisation, new building, and increased staff, will need more expenditure. But in these as in other Health Services, preventive medicine and early treatment is a true economy, and the humane and efficient care and cure of the sick is a responsibility that the community dare not evade.
Finance of the Scheme
How should the finance of a comprehensive National Medical Service be organised? The Labour Party considers that the necessary expenditure should be drawn:
- Partly from national taxation, expended directly by the Ministry of Health (e.g., for the National Health inspectorate);
- Partly from national taxation; allocated by the Ministry of Health to Regional Authorities in the form of percentage grants;
- Partly from rates payable to Regional Authorities.
The Ministry of Health should allocate to each Regional Authority a grant amounting to a percentage of its approved health expenditure; the object being
- To provide a Health Service which is preventive, comprehensive, open to all, and efficient as judged by national standards
- To even out the present inequalities of standard between different areas.
The Ministry of Health should be empowered to exercise “powers of default” in the event of continued failure by a Regional Authority to carry out its functions as a Health Authority in accordance with the principles and standards nationally laid down.
CAN WE AFFORD IT?
The need for a comprehensive Medical Service is literally a “vital” need. We have given solid reasons why that need can only be met by a State Medical Service, nationally planned, locally administered, and financed out of public funds. There remains the crucial question: “Can we afford it?”
One might answer with truth that we cannot afford not to afford a service so necessary for life; but no such facile answer should satisfy us; or, indeed, could satisfy a Chancellor of the Exchequer. Before asserting that the nation should undertake to foot this bill, we must have an adequate idea of the cost of the present service and of the reorganised service.
Pre-war Cost of Existing Service
Before the war Great Britain spent on the treatment of the sick about £140,000,000. £45,000,000 of this went in doctors’ and dentists’ fees, £40,000,000 on public and voluntary hospitals, and £25,000,000 on medicines. Besides this £140,000,000 for treatment of the sick, there was an expenditure of some £8,000,000 on certain preventive medical services, such as the School Medical Service and the Maternity Service.
These figures do not include certain items difficult to assess, such as fees to nursing homes. Nor, it should be noted, do they include cash benefits paid under the insurance schemes; for these should properly figure as part of the loss resulting from ill-health rather than as part of the bill for medical treatment.
The Cost of Ill-health
About £32,000,000 was paid in cash benefits under the insurance schemes in cases of sickness or disablement. The economic loss through stoppage of work by ill-health represents, roughly, a further £120,000,000.
Thus, we may say that the loss resulting from ill-health, together with the cost of the medical services, came to over £300,000,000 a year.
Post-war Cost of Existing Service
After this war, the cost of treatment of the sick, if the medical service were to remain organised as at present, would probably be somewhat higher than before the war, owing to some increase of prices, the need for rebuilding hospital accommodation, and other developments. Let us put the figure at £155,000,000 instead of the £140,000,000 spent before the war. Presumably, also, the cost of the School Medical Service and Maternity Service will increase. It appears then, that, if the Medical Service remains organised as at present, we may expect to pay about £165,000,000 for a service which, as we have seen, will be neither comprehensive nor open to all.
Cost of a Comprehensive Service
The cost of a comprehensive service for the treatment of the sick (not including cash benefits) was carefully examined in the Beveridge Report. The figure was arrived at in consultation with the Ministry of Health and Department of Health for Scotland, so it can be regarded as the most expert estimate we can get at present. It is meant to cover “comprehensive health and rehabilitation services for prevention and cure of disease and restoration of capacity for work, available to all members of the community.” The figure is £170,000,000 a year.
The Report proposes that this cost, should be defrayed out of public funds, subject to a grant-in-aid of £40,000,000 from the Social Insurance Fund.
It will be noted that this figure of £170,000,000 is very close to what we shall be spending on the existing service after the war—about £165,000,000; but the Beveridge estimate is to cover a much wider service.
It must not be assumed that we could not have a more complete service for the same money, if the system were reorganised by the State. The pre-war expenditure of £140,000,000 on treatment of the sick has been carefully analysed by the Socialist Medical Association and by Dr. Stark Murray. They estimate that, if the service were replanned as a State Medical Service, we could get far more than we now get for £140,000,000. For instance, we could increase our hospital accommodation by 25 per cent, and spend £7,000,000 a year on medical research instead of some £400,000 as at present; and we could have the full service of 40,000 doctors, 14,000 dentists, 24,000 pharmacists, etc.
Even if the Beveridge figure of £170,000,000 were to be somewhat exceeded, the burden would still be a light one, having regard to the importance of the need and the size of the national income. That income has been increasing, remember, at the rate of about 1 ½ per cent, annually; there is no reason to anticipate that such an increase will not be resumed soon after the war.
The money we spend on health is not money poured down the drain or blown into space; much of it is productive, since it buys not only release from the frustration and pain of ill-health, but also fulness of life, new strength for new endeavour. At any given time we have in this country about 800,000 people who cannot work owing to ill-health. If, through the State’s new service of preventive medicine and rehabilitation of the disabled, one quarter of this number can be restored to fitness for work, the value of the extra capacity for work by the 200,000 people will amount to something like £60,000,000 a year.
So it comes to this. We shall be spending approximately £170,000,000 a year on the existing service, with all its defects. For about the same money, we could have a comprehensive service, economically planned and open to all.. Which is the more economical investment? The Labour Party has no doubt as to the answer. In the interests of the nation’s health, vigour, and happiness; in the interests of true economy; in the interests of the medical profession as well as the interests of the sick, the Labour Party appeals to every citizen to support this great reform—the organisation of a National Service for Health.
| PRICES, POST FREE | |
|
s. |
d. |
| 1 copy – – – | 3 |
| 12 copies – | – 1 | 6 |
| 50 copies – . 1 – 6 | 0 |
| 100 copies – – – 12 | 0 |
| April, 1943 | |
| Reprinted September, 1943. | |
